Flexor Digitorum Profundus Muscle
Table of Contents
Flexor digitorum profundus Muscle Anatomy
Human forearm muscles called the flexor digitorum profundus are responsible for flexing the fingers, or digits. Because its muscle belly is located in the forearm and it operates on the hand, it is regarded as an extrinsic hand muscle.
This muscle connects the distal phalanges of the second to fifth digit to the proximal portion of the ulna. Flexion of the fingers at the metacarpophalangeal and interphalangeal joints is its primary action. But it also helps with the hand’s flexion at the wrist.
Forming the muscular elevation felt and seen on the posterior surface of the forearm medial to the subcutaneous posterior border of the ulna, it is the strongest and largest muscle in the forearm.
Lumbricals in the palm arise from the flexor digitorum profundus tendons on the sides.
Considering that it receives innervation from two distinct nerves, this muscle is hybrid or composite.
Origin
It originates from,
- medial olecranon
- upper three quarters of anterior and medial surface of ulna as far round as subcutaneous border
- narrow strip of interosseous membrane.
Insertion
It inserts into the distal phalanges of medial four fingers.
Blood Supply
The anterior interosseous artery supplies blood to the muscle.
The anterior (or volar) interosseous artery, a branch of the common interosseous artery, supplies blood to the FDP. The anterior interosseous artery is accompanied by the palmar interosseous branch of the median nerve. Muscular branches of the artery supply the flexor pollicis longus (FPL) and FDP muscles.
Lymphatics Drainage
Both superficial and deep lymphatic vessels make up the venous and lymphatic drainage of the FDP. The cubital lymph nodes, which are located close to the medial humeral epicondyle, receive the outflow of the superficial arteries surrounding the basilic vein. The axillary lymph nodes are the destination of vessels around the cephalic vein. The major deep veins are followed by the deep lymphatic vessels, which ultimately come to an end in the humeral axillary lymph nodes. These channels also drain lymph from the FDP.
Nerve supply
The median nerve (anterior interosseous) and ulnar nerve supplies the muscle.
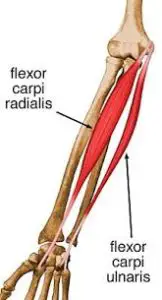
The portion of the FDP connected to digits 2 and 3 is innervated by the anterior interosseous branch of the median nerve (AIN). The ulnar nerve (C8, T1) innervates the muscle portion connected to fingers 4 and 5. The only muscles of the anterior forearm compartment not innervated solely by the median nerve are the flexor carpi ulnaris (FCU) and the flexor dorsiflexor.
Starting from the distal side of the cubital fossa, the median nerve descends between the FDS and FDP. At the mid-forearm level, the AIN splits from the median nerve dorsolaterally. The only purpose of the AIN is motor.
Action
It flexes distal interphalangeal joints, then secondarily flexes proximal interphalangeal and metacarpophalangeal joints and wrist.
Function
Flexor digitorum profundus muscle is a powerful flexor of the fingers. As it pulls the distal phalanges towards the hand, it causes flexion of the digits 2-4 at the metacarpophalangeal and interphalangeal joints.
The muscle can act on its own but it usually works in synergy with the flexor digitorum superficialis, lumbricals, and flexor digiti minimi brevis muscles to perform this action. This muscle is also an accessory wrist flexor, aiding the flexor carpi ulnaris, flexor carpi radialis, palmaris longus, flexor digitorum superficialis, and flexor pollicis longus muscles to flex the hand at the wrist joint.
Muscle Relations
The medial region of the forearm flexor compartment is where the flexor digitorum profundus is located. Throughout its whole length, it is situated deep to the flexor digitorum superficialis muscle. The median nerve travels across the lateral aspect of the muscle’s anterior surface in the forearm.
The flexor digitorum profundus tendons are situated in close proximity to the flexor digitorum superficialis tendons. Each of the four tendons crosses the space defined by the flexor digitorum superficialis terminal slips en route to the distal phalanges of the digits. The flexor digitorum profundus tendons’ deep surfaces are where the hand’s lumbrical muscles attach.
Anatomical Variants
Ruptures of the flexor tendon can occur spontaneously in physiologic types of FDP. Usually coming from the same muscle belly, the two ulnar FDP tendons split in the carpal tunnel or forearm. However, in certain people, the FDP tendons of digits 4 and 5 may fuse at the midpalmar region. This abnormality makes the FDP finger 5 tendon more susceptible to rupture by weakening it against shearing pressures. The FDP tendon without any muscle attachment to the distal phalangeal bases is an extremely uncommon variation.
Embryology
Around the fourth week, the dorsolateral cells of the somites give rise to the upper limb musculature, which migrates into the limb to produce muscles. As the limb buds elongate, the muscle tissue divides into flexor and extensor components, with the direction of each component regulated by connective tissue derived from the lateral plate mesoderm.
Sonic hedgehog is secreted by the zone of polarizing activity at the posterior border of the upper limb to regulate anterior-posterior patterning. After the limb bud forms, brachial plexus nerves enter the mesenchyme. The FDP is finally supplied by the ventral branches, which also create the ulnar and median nerves.
Strengthening Exercise:
1. Ball Grip Exercise:

- Hold the ball tightly in the palm of your hand.
- Squeeze the ball, hold, and relax.
- Repeat ten times, for two sets.
The Power Web is a circular grid made out of resistant rubber that allows the individual to perform a wide array of exercises. The power web is mainly used to build up grip strength in the hand by working on the muscles that flex the fingers. The main finger flexor muscles worked are the flexor digitorum profundus, which flexes the very distal finger joint, and the flexor digitorum superficialis, which flexes the fingers at the knuckles. The secondary muscles worked are the flexor digiti minimi, which flexes the little finger, the flexor indicis, which flexes the index finger and the flexor pollicis longus and brevis and opponens pollicis which all flex the thumb.
Stretching exercise
Standing or sitting, extend the arm in front of you and with a fully extended or locked out elbow, take the wrist into extension and use the other hand to pull the wrist towards you to increase the stretch (Palmaris Longus). Using the other hand pull on the fingers to include a stretch for the Flexor Digitorum Superficialis & Profundus.
Standing 90 degrees to a wall, abduct the shoulder to 90 degrees. With the elbow fully extended or locked out, place the palm of the hand (fingers up) upon the wall. To increase the intensity of the stretch, squat down about 5% first, then place the hand, fingers flat and displaced upon the wall and come to the fully standing position again.

Clinical Importance
Typical FDP wounds consist of the following:
Flexor digitorum profundus (FDP) pain
In clinical practice, flexor digitorum profundus (FDP) pain is a frequently reported symptom that might have a range of underlying causes, from inflammatory diseases to overuse injuries. The flexor digitorum profundus is one of the main flexors of the fingers and is essential to hand function, hence pain in this muscle is an important concern.
Lumbrical plus finger:
Lumbrical plus finger can be caused by rupture of the FDP tendon or amputation of the tendon distal to the lumbrical origins. When trying to flex the fingers, the disease appears as a paradoxical extension of the IP joints.
Quadrigia:
This disorder is caused by the fusion of the FDP tendons to the index finger and the medial three digits. FDP tendon suturing to the extensor tendons, FDP tendon adhesion or amputation, and excessive distal advancement of the FDP tendons after surgery are common reasons. Because the tendons cannot move independently, the patient is unable to produce a full fist and has a weak grasp.
Jersey finger:
This is a rupture of the FDP tendon near the base of a distal phalanx. In 75% of cases, this disease affects the fourth digit. When the DIP joint is extended forcefully, the FDP muscle belly contracts to its maximum, resulting in jersey finger. Based on the degree of tendon retraction and the existence of a fracture, jersey finger cases are categorized using the Leddy and Packer classification.
When at repose, patients may report experiencing soreness and tenderness over the volar distal finger. In addition, the affected finger is somewhat extended in relation to the other fingers. It is possible to palpate the proximally retracted flexor tendon along the flexor sheath. Quadrigia is frequently caused by jersey finger.
AIN injury: The FPL and FDP become paralyzed when the AIN is damaged. Patients are unable to create the “ok” sign as a result.
Volar Compartment Syndrome
Fractures of the radial, ulnar, or supracondylar bones can result in volar compartment syndrome. The symptoms of this illness include weakness in the flexion posture of the fingers, soreness across the volar side of the forearm, and pain on passive finger or wrist extension. The most effective treatment is fasciotomy.
Surgical Importance
The following are some operational methods for FDP avulsion, often known as jersey finger:
- direct restoration of tendons
- Tendon reinsertion with a dorsal button
- Open reduction and internal fixation
- Flexor tendon grafting in two stages
- Distal arthrodesis between the phalanges.
It is recommended to do tendon reinsertion using a dorsal button and direct tendon healing three weeks after the damage. Prompt repair avoids quadrigia, DIP contractures, and the incapacity of the FDP tendons to move freely.
When sufficient healthy tissue is present, direct tendon repair is carried out, which involves suturing the damaged tendon back together. When a tendon is avulsed from its attachment place on the bone, tendon reinsertion using a dorsal button is advised. A metallic or plastic device called a dorsal button helps to reattach the tendon to the bone, as opposed to directly mending the tendon ends.
When there is tendon retraction to the DIP joint or the palm along with a significant avulsion fracture, open reduction internal fixation (ORIF) of the fracture fragment is advised. In order to reach the wounded area, the surgeon makes an open incision during ORIF. After realigning the broken bone or tendon, internal fixation tools such as screws and plates are used to secure the fragments.
For FDP injuries lasting more than three months, two stages of flexor tendon grafting are recommended, and the DIP joint has a complete passive range of motion. In order to suture a healthy tendon graft into the damaged FDP tendon, it is typically taken from the forearm.
A salvage treatment called DIP arthrodesis—which involves fusing the affected finger’s DIP joint—is recommended for long-term injuries that have become stiff.
The flexor tendons can be exposed as much as possible within their fibrous sheaths when the volar technique is used. This method permits digital nerve and vascular repair, fibrous flexor sheath exposure during pus draining, and FDP tendon exploration and repair.


2 Comments