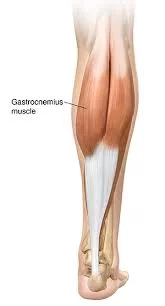
Gastrocnemius Muscle
Table of Contents
Gastrocnemius Muscle Anatomy
The gastrocnemius is located with the soleus in the posterior (back) compartment of the leg. The lateral head originates from the lateral condyle of the femur, while the medial head originates from the medial condyle of the femur.
Its other end forms a common tendon with the soleus muscle; this tendon is known as the calcaneal tendon or Achilles tendon and inserts onto the posterior surface of the calcaneus, or heel bone. It is considered a superficial muscle as it is located directly under the skin, and its shape may often be visualized through the skin.
Origin
Gastrocnemius originates as two heads from the femur. The medial head originates from the popliteal surface of the femoral shaft, and the posterior surface of the medial condyle. The lateral head originates from a facet on the upper lateral surface of the lateral condyle of the femur, where it joins the lateral supracondylar line.
Insertion
The aponeurosis gradually narrows and fuses with the fibres of another deeper muscle, the soleus, to form a large tendon called the calcaneal (Achilles) tendon. The calcaneal tendon attaches to the posterior surface of the calcaneus in the foot.
Nerve supply
The gastrocnemius is innervated by the ventral rami of S1 and S2 spinal nerves, carried by the tibial nerve into the posterior compartment of the leg.
Blood supply
Both medial and lateral heads of gastrocnemius are supplied by the lateral and medial sural arteries, which are direct branches of the popliteal artery.
The gastrocnemius muscle’s venous blood is drained by the popliteal vein. On the medial side of the popliteal artery and the lower border of the popliteal muscle, the popliteal vein is created by the union of the saphenous vein, posterior tibial veins, and anterior tibial veins. Ascending, it becomes the femoral vein after passing through the adductor’s aperture. Cockett veins are perforating veins that affect blood flow as a calf contracts.
Venous Drainage
There are two types of lymphatic vessels in the lower limb: superficial and deep. The medial, lateral, and superficial gluteal collectors are the subcutaneous groups of veins that emerge from the integuments and drain into the superficial inguinal lymphatic grouping. From the bones, muscles, and joints, the deep vessels emerge as satellites of the deep vessels, which ultimately terminate in the deep inguinal lymph nodes.
The efferent arteries of the lateral aortic group of the lumboaortic lymph nodes are located in the lumbar lymph nodes on the left and right. They get their drainage from the splanchnic branches of the aorta into the sub-umbilical area of the abdominal wall, the pelvic wall, the perineal wall, the lower limb, and the vascularized territory.
Actions
At the talocrural joint, the gastrocnemius is a potent plantar flexor of the foot. Moreover, it bends the leg at the knee. The gastrocnemius and soleus are typically regarded as members of the triceps surae group. These are the foot’s crucial plantar flexors. The muscles are strong and sizable. The force required for propulsion while walking, running, and jumping comes from the gastrocnemius.
Relations
The inferior borders of the popliteal fossa are formed proximally by the lateral and medial heads of the gastrocnemius. The medial head is partially covered by the semimembranosus tendon, whereas the lateral head is partially covered by the biceps femoris tendon. The muscle is superficial throughout the rest of its length, showing both bellies through the skin.
The deep fascia divides the tiny saphenous vein and associated sural nerve from the muscle’s superficial surface. Between the muscle’s lateral head and the biceps femoris, the common fibular nerve passes. The tibial nerve, the popliteal vessels, the soleus, and the plantaris muscles are located deep in the gastrocnemius. The flexor digitorum longus, flexor hallucis longus, flexor tibialis posterior, and other deep flexor muscles are situated deep in the gastrocnemius.
Embryology
The development of the skeletal muscles occurs in the eighth week of pregnancy. The paraxial mesoderm, which is derived from the somites in the post-otic area, is the source of the gastrocnemius muscle.
The myotomes, sclerotomies, and dermomyotome of the somites vary. The lateral dermatomyotome’s lips are the source of the muscle precursors. Transverse striations, a characteristic indicator of muscle maturity, mark the final stage of muscle growth. The myotubes, or progenitor cells of muscle fibers, are present at this stage.
Variations
Anatomy and nature always store remarkable variations and adaptations. This also applies to the gastrocnemius. There is an additional soleus muscle and the gastrocnemius tertius, an auxiliary muscular district that is an essential component of the muscle. Rarely can one find these auxiliary muscles bilaterally and concurrently, with no impact on tibial nerve innervation or joint function. If the gastrocnemius tertius were to come into touch with the popliteal artery and result in an arterial entrapment, it might produce issues in the popliteal fossa.
The literature contains anatomical variances. You can locate a quadriceps gastrocnemius muscle in particular. The tibial nerve innervates this variation, however, practitioners are unsure if it produces dysfunctions and diseases.
The gastrocnemius may exhibit abnormalities related to the place of origin rather than head count. This includes the lack of a head, especially the lateral one. An instance of compression of the popliteal vein and popliteal artery resulting from an abnormality in the lateral head of the gastrocnemius origin has been documented in the literature. Secondary pulmonary hypertension was caused by the venous and arterial thrombus that developed as a result of this change.
Assessment
Initially, the physician should watch the patient’s gait, compensatory mechanisms, and any variations in the two calves’ muscular architecture. In order to avoid conditioning the patient or their perception of pain, the physician will palpate the tone of the muscles on both the fleshy level and the fascia (aponeurosis and tendon). Examine the ankle and knee passively following active motions.
Gastrocnemius Muscle
Stretching exercise:
- Stand facing a wall. Keep a distance between you and the wall of approximately 3 feet. Take one step toward the wall with your right foot.
- Place both palms on the wall. Bend your right knee.
- Lean forward, keeping the left leg straight and the left heel on the floor you will feel a stretch in the left leg calf muscles.
- Hold for 30 to 60 seconds. Repeat 2 to 5 times, or as instructed.
- Switch the legs and repeat.
Strengthening exercise:
- Double-Leg Calf Raise. Calf raises are the classic calf-strengthening exercise. They use your body weight to strengthen and tone the gastrocnemius.
Starting position: Stand near a wall for balance. Place your feet hip-width apart, and make sure your ankles, knees, and hips are in vertical alignment to protect your joints.
Action: Press down into the balls of both feet to raise your body upward. Keep your abdominal muscles pulled in so that you move straight upward, rather than shifting your body forward or backward. - Seated Calf Raise. You can do this exercise at home or at the gym on a calf exercise machine. The exercise works both the gastrocnemius.
Starting position: Sit on a firm, sturdy chair with your feet flat on the floor. Keep your knees aligned directly over your feet. Don’t let your knees turn in or out. Lean forward placing hands on thighs near knees pushing down to add resistance.
Action: Press slowly down into the balls of your feet to raise your heels as high as you can. Next, slowly lower your heels. Repeat. - Calf-Building Sports: Taking part in the following sports will help you both strengthen and tone your calves.
- Running, walking, and hiking are excellent calf-strengthening exercises, especially when you go uphill. The steeper the climb, the more your calves have to work.
- Running sports such as soccer, basketball, and tennis demand that you run, jump, and push off your calf muscles to accelerate or change direction quickly. So they’re great for toning calves.


Deformity:
In equinus deformity-related gastrocnemius muscle.

Correct Evaluation of the Equine Foot
The operator must apply around two kilograms of force while placing the hand beneath the sole or the head of the second metatarsal in order to properly complete the Silfverskiold test.
In the event that the patient has a non-rigid flat foot, the heel is in a valgism posture; in this scenario, pure dorsiflexion does not occur, and the hindfoot joints allow the movement to manifest itself on an oblique plane.
The hindfoot has to be in a neutral or slightly varied posture to enhance test execution and produce a smooth movement. It is possible to do the Taloche test or the Taloche sign in advance of this test. The patient will not be able to maintain the orthostatism if it is resting on an inclined plane (a tablet) if the gastrocnemius muscle is contracted.
Tibial Nerve Entrapment
The tibial nerve tract is superficial and easy to physically hear in the popliteal cavity and somewhat below. It may be palpated in both of these locations. When the nerve reaches the ankle region, it changes its name to the posterior tibial nerve and continues into the tarsal tunnel, passing deeper than the posterior tibial artery and vein as well as the flexor retinaculum.
Another location where the tibial nerve can be contacted is behind the medial malleolus, which is located slightly below and medially of the calcaneal tendon. To find the malleolus, use your thumb, then slowly move your finger in a horizontal manner toward the tendon. The patient is frequently unaware that it is a painful location.
In contrast to the tarsal tunnel, where it is more commonly entrapped, the tibial nerve is rarely entrapped in the popliteal hollow. Various factors can lead to this amount of deformity, including tumors, prior interventions, trauma, systemic illnesses including diabetes, neurological disorders, and deformities of the same foot. To elicit the painful or paresthesia sensations, a stress test using the Tinel test might be performed.
Calcaneal Tendon Rupture Evaluation
The Simmonds-Thompson sign, also known as the Thompson squeeze test, is a semiotics technique used in the objective evaluation of the lower limb. If the test results are good, it means that the calcaneal tendon has completely ruptured. The patient is placed in a prone posture with their feet resting over the side of the bed, and the examiner crushes their calf between their fingers. Normal circumstances result in the plantar flexion of the foot due to the squeezing of the muscle masses; nevertheless, full-thickness tears of the posterior calcaneal tendon structures produce excruciating pain and immobility of the foot.
Physiotherapy for Tears
The RICE protocol (Rest, Ice, Compression, Elevation) is the course of therapy for an anatomical lesion within the first 24 to 48 hours. By using this therapy, irritation, and lesion exacerbation are prevented. This treatment plan calls for rest, bandaging, elevation of the affected limb, and 20 minutes of ice three to four times a day.
In most cases, analgesics (which are better than nonsteroidal anti-inflammatory drugs [NSAIDs]) and muscle relaxants are used together since inflammation following an injury is the body’s natural healing process. Depending on the severity of the injury, the athlete’s time away from the field may vary, spanning from one week to two months.
Following an injury, the muscle heals the lesion, producing fibrous cicatricial tissue, which makes the muscle’s connective tissue less elastic. In the event that the muscle is immobilized, a scar with freely orientable fibers forms; in the event that the muscle is kept in motion, the resulting connective tissue fibers are arranged in a force-line-based pattern and exhibit greater elasticity. In order to make the muscle more elastic and prevent recurrences, exercise is required once the lesion has healed, which calls for instrumental physiotherapy using CO2 laser, ultrasound, and Tecar treatment.
It’s crucial to stretch and reinforce eccentrically. Usually, muscle-tendon ultrasonography is the preferred examination; however, if the lesion is deep within a well-developed muscle, magnetic resonance imaging can be required.
Rupture of the Calcaneal Tendon
The duration of the rehabilitation treatment for calcaneal tendon rupture is approximately 12 weeks, with three sessions per week alternating between the gym and the swimming pool. The sessions include massage therapy for the calf muscles and scar, physical therapy for pain and swelling, and articulation exercises to restore strength and proper gait.
An isokinetic test can be used to gauge the leg’s muscle strength after around three months. In order to expedite the athlete’s return, the treatment regimen must be tailored to the athlete’s sport and take into account the special technical gestures of the activity they perform.
Certain gastrocnemius muscle disorders may benefit from the application of elastic bands to the affected muscle tissue. When trigger sites are present, tape has been shown to be effective in symptomatology reduction.
It appears that there is a reason to tape the calcaneal tendon in order to prevent sports-related injuries.
Osteopathy
When there are scars, an osteopathic treatment using mild methods may assist to enhance function and stop additional discomfort.
Patients with tendinitis have demonstrated improved plantar flexion amplitude and a reduction in symptomatology when treated with osteopathy.
Dry Needling
Dry needling is a tool used by clinicians and physiotherapists to treat trigger points or to enhance the way muscles respond to past sports injuries. These are simple instruments that have been shown in the literature to improve neurological pathology or the muscular function of the gastrocnemius muscle in athletes.
FAQ
It begins above the knee joint at the base of the femur (thigh bone), and it inserts into the rear of the heel through the Achilles tendon. There are two ‘heads’ to the gastrocnemius muscles. The posterior aspect of the medial femoral condyle is the source of the medial (inside) head.
A general anesthetic is often used for the gastrocnemius/soleus aponeurotic lengthening (also known as Strayer’s, Baker’s, or Vulpius release). A portion of the muscle or gristle is sliced on the back of the calf and left to grow. This surgery has several versions.
The Greek terms γαστήρ (gaster), which means stomach or belly, and κvήμη (kneme), which means leg, are the source of its name. Together, the two words refer to the “belly of the leg,” or the majority of the calf.
The huge muscle on the posterior calf of the leg is referred to as the gastrocnemius, or leg tricep. It makes up the majority of the calf muscle and is the most superficial muscle in the leg. The Greek words “gaster,” which means stomach or belly, and “kneme,” which means leg, are the source of its name.
The medial and lateral sural arteries, as well as branches of the popliteal artery, supply the medial and lateral heads of the gastrocnemius muscle (gastroc). Furthermore, anastomotic veins pass within the muscle material between bellies.
An acute injury known as a medial gastrocnemius strain results from suddenly overextending the biggest muscle in the calf. Tiny rips in the muscle fibers are the source of the discomfort. Some patients experience no pain at the scene, but they do hear a “pop” when the damage happens.

11 Comments