Lateral Rectus Muscle
Table of Contents
Introduction:
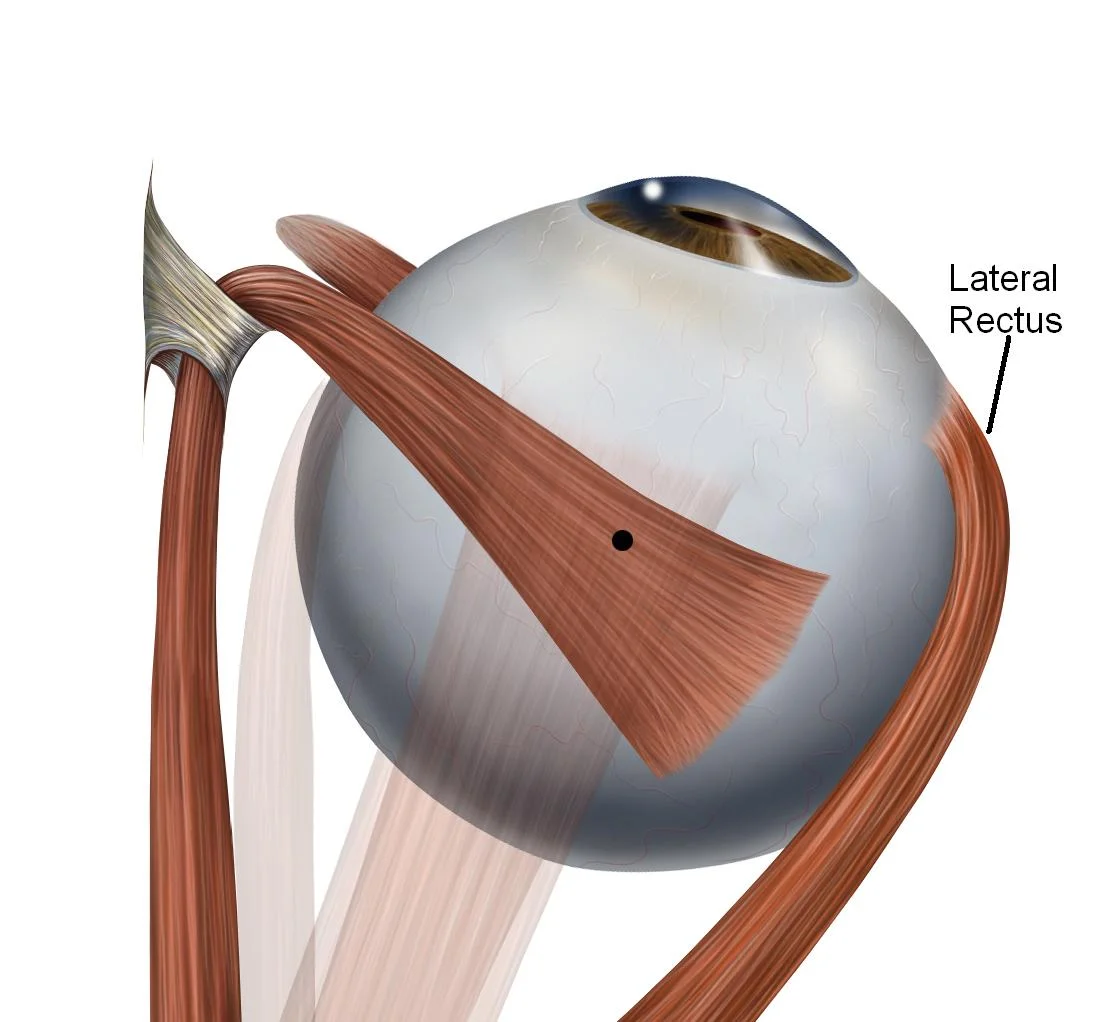
- The lateral rectus muscle is a muscle on the lateral side of the eyeball in the orbit.
- It is one of six extraocular muscles that control the movements of the eye.
- The lateral rectus muscle is responsible for the lateral movement of the eyeball, specifically abduction. Abduction describes the movement of the eye away from the midline (i.a. nose), allowing the eyeball to move horizontally in the lateral direction, bringing the pupil away from the midline of the body.
- The lateral rectus muscle is one of the 4 straight muscles of the orbit responsible for the movement of the eye in the cardinal directions.
- These muscles, along with the superior and inferior oblique muscles, belong to the extraocular muscles of the eye.
- The lateral rectus muscle arises from the common tendinous ring and runs anteriorly across the lateral part of the orbit to insert at the lateral side of the eyeball. Like other straight muscles, the lateral rectus is named by its position within the orbit relative to the eyeball.
Origin:
- The lateral rectus originates at the lateral part of the annulus of Zinn, also known as the annular tendon or common tendinous ring, and inserts into the temporal side of the eyeball.
Insertion:
- The muscle inserts at the lateral side of the eyeball after crossing the tendon of the inferior oblique muscle.
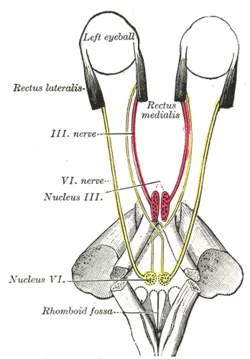
Nerve supply:
- The lateral rectus muscle is supplied by branches of the abducens nerve (CN VI).
Actions:
- abducts the eyeball (makes it move outwards).
Blood Supply:
- The lateral rectus muscle is supplied by the ophthalmic artery.
The blood flow to the extraocular muscles varies. Like all other extraocular muscles, the lateral rectus gets one or two branches of the inferior muscular artery as well as the lacrimal artery. The ocular artery, which is a branch of the internal carotid artery, gives rise to the lacrimal artery.
The inferior and superior orbital veins, which are situated medially and laterally to the superior and inferior rectus muscles, receive the veins that bear the same names as their corresponding arteries. The cavernous sinus empties into the inferior and superior petrosal sinuses before emptying into the internal jugular vein. These two veins empty into the cavernous sinus (sometimes directly, and other times the inferior orbital vein empties into the superior orbital vein and subsequently to the cavernous sinus).
Relations:
- The lateral rectus muscle extends along the lateral wall of the orbit. It arises from the lateral part of the common tendinous ring near the attachments of the medial, lateral, and superior recti muscles.
- This tendinous ring encircles the margins of the optic canal and part of the superior orbital fissure, hence the attached muscles form a cone that envelops the structures entering the orbit.
- These structures include the optic sheath containing the optic nerve (CN II) and ophthalmic artery, the superior and inferior divisions of the oculomotor nerve (CN III), the nasociliary nerve (CN V₁), and the abducens nerve (CN VI).
- After arising from the common tendinous ring, the lateral rectus lies lateral to the ciliary ganglion near the apex of the orbit.
- The lateral rectus muscle then runs along the lateral wall of the orbit towards the eyeball, passing medially to the lacrimal gland. In addition, the lacrimal artery runs along the superior border of the lateral rectus muscle to supply the lacrimal gland.
Extraocular Muscles
Unlike other skeletal muscles in the human body, the rectus and extraocular muscles are made up of a specific mix of fiber types that allow them to move quickly (saccadic motions) and withstand exhaustion. Additionally, compared to other muscle insertions, the rectus muscle insertions are far more accurate.
Each muscle begins at the annulus of Zinn, extends anteriorly, and inserts on the globe at a precise distance from the limbus. The lateral rectus muscle, for instance, inserts into the limbus approximately 6.9 mm.
The superior and inferior rectus muscles combine to produce the vertical rectus muscles, whereas the lateral rectus forms the horizontal rectus muscle alongside the medial rectus.
Embryology
Like all other extraocular muscles, the lateral rectus muscles are derived from mesoderm. Remember that neural crest cells are the source of all connective tissue. The literature contains case studies where the development of the lateral rectus or other extraocular muscles is compromised.
Variations
Strabismus, or misalignment, is known to be caused by the abnormal origin of the lateral rectus muscle. Furthermore, there are case reports describing the absence of the lateral rectus muscle.
Examination
People may gaze to the right with their right eye and to the left with their left eye because the lateral rectus muscle abducts the eye. When testing all nine extraocular muscles at once, clinicians typically have the patient gaze in each direction while tracking the doctor’s finger or pen as it makes an “H” shape in the air with their eyes.
Additional testing, such as the cover test, may be required in certain cases to detect extraocular muscle disease.
Clinical significance:
- Damage to the abducens nerve (CN VI) can result in paralysis of the lateral rectus muscle This condition is called abducens nerve palsy.
- This condition can occur from an expanding lesion such as a tumour or a cyst that compresses the abducens nerve itself or its nucleus.
- The main symptoms of abducens nerve palsy are reflected in the lateral rectus dysfunction, in which the eye is unable to move laterally.
- Since the abducens nerve only innervates the lateral rectus, other extraocular muscles will not be affected. Therefore, the muscle that is functionally antagonistic to the lateral rectus will overpower it and pull the eyeball on its side.
- This results in the eyes being fully adducted by the unopposed medial rectus muscle.
Etiology of Abducens nerve palsy
- The etiology of abducens nerve palsy requires knowledge of the nerve path.
- Neoplasm and trauma may affect the abducens nerve at any point along its path resulting in abducens nerve palsy.
- They are mainly affected by increased intracranial pressure and some symptoms like headache, nausea, vomiting, and papilledema may be noted.
- some other causes are noted like an aneurysm, carcinomatous meningitis, procedure-related injury (e.g., spinal anesthesia, post-lumbar puncture), inflammatory lesions (e.g., sarcoid, lupus), infection (e.g., Lyme disease, syphilis, tuberculosis, Cryptococcus).
Pathophysiology:
- The abducens nerve has the longest intracranial course of any cranial nerve and It is primarily responsible for ipsilateral eye abduction.
- Abducens nerve palsy results in an inability of the abducens nerve to transmit signals to the lateral rectus, resulting in an inability to abduct the eye and horizontal diplopia.
Treatment of Abducens nerve palsy
- The physiotherapy treatment of abducens nerve palsy includes eye muscle exercises, prism therapy, injection of botulinum toxin, and strabismus surgery.
Lateral rectus myositis
Lateral rectus myositis is an uncommon condition that often indicates a rare inflammatory illness, as documented in the literature. An unusual manifestation of a non-Hodgkin B cell mucosa-associated lymphoma (MALT) might be lateral rectus muscle myositis.
Surgical Considerations
Surgery may be required to repair strabismus in certain cases. This procedure corrects the eye’s malalignment, restoring the patient’s ability to utilize both eyes together and their binocular function. Additionally, surgery can enhance the eyes’ look.
Owing to its location, the nerve may occasionally sustain injury during surgery; this may occur if the surgeon moves the tools forward around 3 cm posterior to the lateral rectus muscle’s insertion.
During surgery, the blood supply may potentially sustain harm. Blood is also supplied to the nasal portion of the anterior region of the eye by the same blood arteries that supply the lateral rectus muscle. Therefore, during surgery, the surgeon has to be mindful of the lateral rectus muscle’s vascular supply.
FAQ
The nerve may function badly or not at all if there is damage to it somewhere along its course. Your eye bends inward toward your nose because it can no longer contract normally in the lateral rectus muscle. Sixth nerve palsy can occasionally occur in the absence of other symptoms. We refer to this as isolated sixth nerve palsy.
The oculomotor nerve, whose superior branch feeds the superior rectus and whose inferior branch serves the inferior and medial rectus, innervates the other muscles. The sixth cranial nerve – the abducens nerve supplies the lateral rectus.
Cranial nerve VI
The abducens nerve, cranial nerve VI, enters the muscle on the medial side and innervates the lateral rectus.
Lateral rectus exercises
Looking at the extremes in each direction—up, down, right, and finally left—is part of the cardinal point practice. Ten seconds should be spent fixing your gaze at each cardinal point. Do the workout five times in total.
Together with the medial rectus, an adductor, the lateral rectus is an abductor muscle that moves the eye laterally and side to side.
A lateral rectus palsy can result after head trauma, however, this is often caused by elevated intracranial pressure. Lateral rectus palsy can occasionally be caused by inflammation in the nerve’s surrounding tissue.
References
Cabrera, A. F. (2023, August 8). Anatomy, Head and Neck: Eye Lateral Rectus Muscle. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK539721/


3 Comments