Use of TENS Machine In Physiotherapy : Uses, Indication, Precautions | Transcutaneous Electrical Nerve Stimulation
Table of Contents
What is Transcutaneous Electrical Nerve Stimulation(TENS)?

Transcutaneous Electrical Nerve Stimulation is a treatment for pain that can be used for acute pain (e.g., during labor or after surgery) or for chronic pain (e.g., low back pain). It is a form of electrical energy sent in various wave forms to the nerves.
When it is delivered through electrodes or patches placed on the skin, it is called transcutaneous (meaning through the skin) electrical nerve stimulation or TENS for short.
~TENS is a noninvasive way to override or block signals from the nerves to the spinal cord and brain. Pain messages may be altered enough to provide temporary or even long-lasting pain relief. In addition to controlling pain, this type of electrical stimulation can also improve local circulation and reduce or eliminate muscle spasm.
~Transcutaneous electrical nerve stimulation (TENS or TNS) is the use of electric current produced by a device to stimulate the nerves for therapeutic purposes. TENS, by definition, covers the complete range of transcutaneously applied currents used for nerve excitation although the term is often used with a more restrictive intent, namely to describe the kind of pulses produced by portable stimulators used to treat pain. The unit is usually connected to the skin using two or more electrodes.
~A typical battery-operated TENS unit is able to modulate pulse width, frequency and intensity. Generally TENS is applied at high frequency (>50 Hz) with an intensity below motor contraction (sensory intensity) or low frequency (<10 Hz) with an intensity that produces motor contraction. While the use of TENS has proved effective in clinical studies, there is controversy over which conditions the device should be used to treat.
How does a TENS machine work ?
~TENS machines produce an electrical impulse that can be adjusted for pulse, frequency, and intensity. The exact mechanism by which it works to reduce or even eliminate pain is still unknown. There are several possible ways TENS works. For example, TENS may inhibit (block) pain pathways or increasethe secretion of the pain-reducing substances (e.g., endorphins, serotonin) in the central nervous system.
~TENS is a noninvasive way to treat pain. Pain messages may be altered enough to provide temporary or even long-lasting pain relief. Besides controlling pain, this type of electrical stimulation can also improve local circulation and reduce or eliminate muscle spasm.
What is a TENS Machine?
~TENS is an abbreviation of Transcutaneous Electrical Nerve Stimulation.
~Transcutaneous means “across the skin”. In simple terms, a tens machine stimulates your nerves via an electrical current through your skin.
~A TENS machine is an electronic medical device. A TENS machine may assist you in modest short- term pain relief.
~The use of a TENS machine should be as one part of a pain management program under the guidance of your doctor or healthcare practitioner. Your health practitioner should always be consulted before using a TENS machine.
TENS unit:-

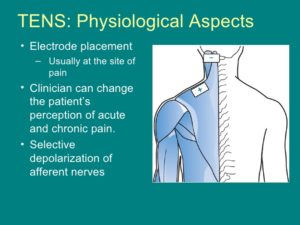
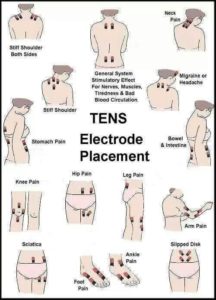
~You will be shown how to use your TENS device by your physiotherapist at Advantage Physiotherapy. Round or square rubber electrodes are applied to the skin over or around the painful area. The electrodes are self-adhesive with a protective layer of gel built in to prevent skin irritation or burning. Usually four electrodes (two pairs) are used to get maximum benefit from this treatment although two electrodes can also be used and in many cases provide sufficient relief.
~The unit is battery-operated with controls you manipulate yourself to alter the strength of the electrical signal. The unit can be slipped into a pocket or clipped to your belt.
~The electrodes will be placed on your body at positions selected by your physiotherapist. The electrode placement is determined based on the location of the involved nerves and/or the location of your pain. Most often the electrodes are placed either directly over the painful area or on either side of the pain.
~Once the electrodes are in place, the intensity of the unit is turned up until you feel a buzzing, tingling, or thumping sensation that is strong but comfortable.
~If placing the electrodes directly over or surrounding the painful area doesn’t work, more relief may be gained by putting the electrodes over the area where the spinal nerve root that supplies the painful area exits the vertebra. Your physiotherapist will guide you through the trial-and-error process for finding the best electrode placement for you and will make any changes needed in the program to suit your comfort level and your needs.
~Another way to use TENS is over spots in the muscles called trigger points (TrPs). Trigger points are areas of hyperirritability in the muscles that can cause chronic pain. Your physiotherapist will identify any TrPs present during their physical examination.
~Significant pain relief may be achieved with as little as 20-30 minutes of TENS use. Some patients find relief of symptoms for 1-2 hours even after the unit is removed. How long you use it will depend on the cause of your symptoms (i.e. post-operative pain vs chronic low back pain), the pain intensity, and the chronicity of your pain.
~For certain conditions like chronic pain or for women in labour, TENS can be used for several hours at a time. The unit should not be used however, for extremely long periods of time (e.g., 24 hours) or during extended sleep time (use during naps is permitted but TENS should not be used while sleeping at night or while sleeping for more than a couple of hours).
~If you experience increased pain be sure to let your physiotherapist know. In some cases electrodes placed below the level of a peripheral nerve impairment might actually block the input from the TENS unit and cause increased pain. Placement over an area of scar tissue from surgery can cause increased skin resistance anddecreased transmission of the electrical impulses.
~Fortunately there are no significant adverse effects from the use of TENS.
How does a TENS Machine provide Short-term Pain Relief?
Pain is thought to be controlled by TENS in one of two ways:
(1)Sensory Level Stimulation – The Gate Control theory of pain means that the electrical input of the TENS machine interferes with the transmission of pain signals, by blocking the neural “gate” through which the pain travels.
(2)Motor Level Stimulation – The goal of motor level stimulation is to cause the release of the body’s own opiate- like substances to achieve pain relief.
TENS Machine uses :

~pain relief
~increased circulation and healing
~improved sleep patterns
~decreased use of pain relievers or other analgesic drugs
~increased motion and function
~TENS can be used for relief of pain associated with a wide variety of painful conditions. Back pain caused by spine degeneration, disc problems, or failed back surgery is commonly relieved by the use of TENS. Nerve pain (neuropathy) from conditions such as chronic regional pain syndrome (CRPS) or diabetes may also be managed with TENS.
~TENS has been used for people suffering from cancer-related pain, phantom-limb pain (a chronic pain syndrome following limb amputation), and migraine or chronic tension-type headaches.
~TENS can also be used for muscle soreness from overuse, inflammatory conditions, and both rheumatoid and osteo-arthritis. Athletes with painful acute soft tissue injuries (e.g., sprains and strains) may benefit from TENS treatment.
~Sometimes TENS is used after surgery for incision or post-operative pain (e.g., joint replacement, cardiac procedures, various abdominal surgeries, or cesarean sections). Studies show that TENS can significantly reduce the use of analgesics (pain relievers, including narcotic drugs) after surgery.
~TENS is usually used along with other forms of treatment and pain control such as analgesics,relaxation therapy, biofeedback, visualization or guided imagery, physiotherapy, exercise, massage therapy, nerve block injections, and/or spinal manipulation.
Contraindications:-
~Patients who do not comprehend the physiotherapist’s instructions or who are unable to co-operate
~It has been widely cited that application of the electrodes over the trunk, abdomen or pelvis during pregnancy is contraindicated BUT a recent review suggests that although not an ideal (first line) treatment option, application of TENS around the trunk during pregnancy can be safely applied, and no detrimental effects have been reported in the literature
~TENS during labour for pain relief is both safe and effective
~Patients with a Pacemaker should not be routinely treated with TENS though under carefully controlled conditions it can be safely applied. It is suggested that routine application of TENS for a patient with a pacemaker or any other implanted electronic device should be considered a contraindication.
~Patients who have an allergic response to the electrodes, gel or tape
~Electrode placement over dermatological lesions e.g. dermatitis, eczema
~Application over the anterior aspect of the neck or carotid sinus
Precautions :
~If there is abnormal skin sensation, the electrodes should preferably be positioned elsewhere to ensure
effective stimulation
~Electrodes should not be placed over the eyes
~Patients who have epilepsy should be treated at the discretion of the therapist in consultation with the
appropriate medical practitioner as there have been anecdotal reports of adverse outcomes, most especially (but not exclusively) associated with treatments to the neck and upper thoracic areas
~Avoid active epiphyseal regions in children (though there is no direct evidence of adverse effect)
~The use of abdominal electrodes during labour may interfere with foetal monitoring equipment and is therefore best avoided.
~One of the most common forms of electrical stimulation used for pain management is transcutaneous electrical nerve stimulation (TENS) therapy, which provides short-term pain relief. Electrical nerve stimulation and electrothermal therapy are used to relieve pain associated with various conditions, including back pain. Intradiscal electrothermal therapy (IDET) is a treatment option for people with low back pain resulting from intervertebral disc problems.
TENS Modes:-
(1)Traditional TENS (Hi TENS, Normal TENS)
(2)Acupuncture TENS (Lo TENS, AcuTENS)
(3)Brief Intense TENS
(4)Burst Mode TENS
(5)Modulation Mode TENS
TENS—MECHANISM OF ACTION:-
*The Pain gate-control theory:-
(1)High frequency or conventional TENS (90-130Hz) :
High frequency (HF) or conventional TENS (90-130Hz), causes the pain gate to close by stimulating the small A-beta sensory nerve fibers. Conventional TENS also acts by reducing the release of excitatory neurotransmitters such as aspartate and glutamate, increasing the release of inhibitory neurotransmitters such as gamma-aminobutyric acid (GABA) and serotonin.
(2)“Low frequency” or “acupuncture” TENS (2-5Hz) :
LF TENS is also known as acupuncture TENS has a low pulse rate. It acts by stimulating the A-delta nerve fibers to produce endorphins which in turn relieve pain.
(3)Burst TENS :
Burst TENS stimulates both the A-beta and A-delta nerve types at the same time. In “burst” mode, conventional (HF) TENS is regularly interrupted by 2-3 “bursts” of lower frequency TENS. Different programs can be used interchangeably according to the preference of the patient.
(4)Low frequency TENS vs. high frequency TENS :
~Kocygit et al. in 2012 published a randomized controlled trial which compared 20 patients with subacromial impingement with patients being randomized into low TENS and Sham groups. Both the groups were given painful stimuli before and after TENS treatment. They found on functional magnetic resonance imaging (MRI) that in the LF TENS group, there was a statistically significant decrease in the perceived pain intensity and pain-specific activation of the contralateral primary sensory cortex, bilateral caudal anterior cingulate cortex, and of the ipsilateral supplementary motor area.
They also reported in their results a statistically significant correlation between the change of Visual Analog Scale (VAS) value and the change of activity in the contralateral thalamus, prefrontal cortex, and the ipsilateral posterior parietal cortex. It was reported that the sham TENS group had no significant change in VAS value and activity of regions of interest.
~The results of this study support the efficacy of LF TENS in acute pain management. Although the sample size is low,
~MRI is a reliable tool in measuring the pain perceived by the individual. Santos et al. in 2013 published a study done on rat paws wherein hyperalgesia and edema was induced by administering serotonin (5-HT). They applied LF and HF TENS on the right paw for 20 mins followed by serotonin induction. They used the Hargreaves method to measure nociception while the hydroplethysmometer was used to measure edema. Hargreaves method measures cutaneous hyperalgesia to thermal stimulation in animals. This study reported that neither HF nor LF TENS inhibited 5-HT- induced edema. However, LF TENS, but not HF TENS, completely reduced 5-HT-induced hyperalgesia. Pre-treatment of the paw with naltrexone, prior to application of TENS, showed a complete blockade of the analgesic effect induced by LF TENS.
~This study supports the participation of peripheral endogenous opioid receptors in LF TENS analgesia in addition to its central action.
~LF TENS takes a longer time to achieve analgesia. Since the analgesia produced by the application of LF TENS is due to the release of endogenous opioids it lasts for a longer time. HF TENS or conventional TENS has a quick onset of analgesia but loses its effect quite rapidly when turning off the stimulation. The post-treatment analgesic effects of TENS can thus last anywhere between 5 minutes to 18 hours. It has been reported that in some patients’ pain levels do not return to pre-stimulation levels even after 24 hours.
TENS-EVIDENCE FOR USE:-
(1)Postoperative/acute pain
Very few systematic reviews have examined the use of TENS for postoperative pain management. Out of 17 randomized controlled trials analyzed by Carroll et al. in a systematic review which included studies with pain outcomes, 15 concluded that TENS had no analgesic benefit in the acute postoperative period.[9] A systematic review conducted by Reeve et, included 20 studies of postoperative pain, and concluded that 12 of these had positive TENS outcomes.
~A Cochrane review published in 2009 excluded studies that allowed additional analgesics. The authors could extract data from only six of the 12 Randomized Controlled Trials RCT s that met their inclusion criteria. This review reported that only one out of five studies comparing TENS with placebo showed a statistically significant superior effect of active TENS. Owing to insufficient data this review could not come to a definitive conclusion about the effectiveness of TENS as a sole treatment for acute pain.[6]
(2)Chronic pain
~ Out of the 22 inactive control (placebo) studies they reviewed, 13 had a positive analgesic outcome and favored active TENS treatments. Whereas out of the 15 multiple-dose treatment comparison studies reviewed by them, only eight favored active TENS treatments.
(3)Neuropathic pain :
~Cruccu et al. in a systematic review recommended the use of standard high-frequency TENS when compared with placebo treatment for neuropathic pain. This review also suggested that TENS should be considered specifically to treat painful diabetic neuropathy. This review was endorsed by the European Federation of Neurological Societies guidelines for the treatment of neuropathic pain.
(4)Fibromyalgia :
~TENS as an adjuvant therapy is effective in relieving pain in fibromyalgia.
~Mechanisms of TENS reduction on analgesia
TENS activates a complex neuronal network to result in a reduction in pain. At frequencies and intensities used clinically, TENS activates large diameter afferent fibers .This afferent input is sent to the central nervous system to activate descending inhibitory systems to reduce hyperalgesia. Specifically, blockade of neuronal activity in the periaqueductal gray (PAG), rostral ventromedial medulla (RVM) and spinal cord inhibit the analgesic effects of TENS showing that TENS analgesia is maintained through these pathways .
In parallel, studies in people with fibromyalgia show that TENS can restore central pain modulation, a measure of central inhibition . Therefore, TENS reduces hyperalgesia through both peripheral and central mechanisms.
~Neurotransmitters & receptors that mediate TENS analgesia
HF TENS increases the concentration of ß-endorphins in the bloodstream and cerebrospinal fluid, and methionine -enkephalin in the cerebrospinal fluid, in human subjects [7,8]. The analgesia produced reduction in hyperalgesia by HF TENS is prevented by blockade of opioid receptors in the RVM or spinal cord, or synaptic transmission in the ventrolateral PAG [4–5,9]. This opioid-mediated analgesia produced by HF TENS has been confirmed in human subjects . Furthermore, the reduction in hyperalgesia produced by HF TENS is prevented by blockade of muscarinic receptors (M1 and M3) and GABAA receptors in the spinal cord . However, blockade of serotonin or noradrenergic receptors in the spinal cord has no effect on the reversal of hyperalgesia produced by HF TENS Thus, HF TENS produces analgesia by activating endogenous inhibitory mechanisms in the central nervous system involving opioid GABA, and muscarinic receptors.
~The reduction in hyperalgesia by LF TENS is prevented by blockade of µ opioid receptors in the spinal cord or the RVM or spinal cord, and by synaptic transmission in the ventrolateral PAG . Further, the reduction in hyperalgesia by LF TENS is prevented by blockade of GABAA, serotonin 5-HT2A and 5-HT3, and muscarinic M1 and M3 receptors in the spinal cord [11–13], and is associated with increased release of serotonin . This opioid mediated effect of LF TENS has been confirmed in human subjects . In addition, LF TENS does not produce analgesia in opioid tolerant people and animals but HF TENS does [16,17]. Thus, LF TENS uses classical descending inhibitory pathways involving the PAG-RVM pathway activating opioid, GABA, serotonin and muscarinic receptors to reduce dorsal horn neuron activity and the consequent pain.
~Reduction in central excitability
In animals without tissue injury, both LF and HF TENS reduce dorsal horn neuron activity . In animals with peripheral inflammation or neuropathic pain, enhanced activity of dorsal horn neurons (i.e., central
sensitization) to both noxious and innocuous stimuli is reduced by both HF and LF TENS. In parallel, there is a reduction in both primary and secondary hyperalgesia by both LF and HF TENS Furthermore, in people with fibromyalgia and osteoarthritis, there is a reduction in pressure pain thresholds not only at the site of stimulation, but also at sites outside the area of application, implicating a reduction in central excitability.
~HF TENS also reduces central neuron sensitization, and release of the excitatory neurotransmitters glutamate and substance P in the spinal cord dorsal horn in animals with inflammation .
Peripheral mechanisms of TENS :
~Both HF and LF TENS have effects at the site of stimulation. HF TENS reduces substance P, which is increased in dorsal root ganglia neurons in animals after tissue injury . Blockade of peripheral opioid receptor prevents the analgesia produced by LF, but not HF TENS . Thus, TENS may also alter excitability of peripheral nociceptors to reduce afferent input to the central nervous system.
~In a-2a adrenergic knockout mice, analgesia by LF and HF TENS does not occur . Blockade of peripheral, but not spinal or supraspinal, a-2 receptors prevents the analgesia produced by TENS suggesting a role for peripheral a-2a-adrenergic receptors in analgesia produced by TENS. Further, the reduction in cold allodynia by LF TENS is reduced by administration of systemic phentolamine to block a-adrenergic receptors.This adrenergic effect may alter the autonomic system. There are increases in blood flow with LF TENS at intensities that produce motor contractions; greater than 25% above motor threshold . Thus, some of the analgesic effects of TENS are mediated through peripheral adrenergic receptors.
~Factors that directly affect TENS efficacy
The factors affecting TENS efficacy include the population and the outcome assessed, timing of the outcome measures, negative interaction of opioid use and the parameters of the TENS dose. Three important factors for TENS efficacy are tolerance to repeated TENS, intensity of the stimulation and electrode placement. A recent article by Sluka et al. provides an extensive review of variables that can affect the clinical use of TENS.
~Tolerance to repeated TENS
Repeated application of either LF or HF TENS at the same frequency, intensity and pulse duration daily (i.e., same dose), produces analgesic tolerance in animals and humans. The analgesic tolerance by LF TENS results in cross-tolerance at µ-opioid receptors in the spinal cord, and the analgesic tolerance by HF TENS results in cross-tolerance at d-opioid receptors in the spinal cord in animals.
Prevention of analgesic tolerance occurs with pharmacological modulation of pathways involved in opioid tolerance. Specifically blockade of NMDA-glutamate receptors or CCK receptors in the spinal cord prevents analgesic tolerance to both LF and HF TENS Analgesic tolerance can also be prevented by modulating between LF and HF TENS within a treatment session, or by increasing intensity of TENS daily. Thus, animal studies suggest TENS tolerance can be delayed with pharmacological methods as well as with non-pharmacological modulation of TENS parameters.
~Intensity of TENS established as a critical factor in efficacy remains comfortable produces hypoalgesia in healthy subjects; lower intensities are ineffective. In addition to activation of greater numbers of sensory afferents, higher pulse amplitudes are proposed to activate deeper tissue afferents allowing for greater analgesia. High intensity TENS decreases post-operative opioid requirements and negative opioid-side effects. Even as researchers demonstrate the importance of intensity in TENS delivery, TENS systematic reviews continue to include studies with wide ranging intensity settings. In fact, as outlined below, application of TENS at inadequate intensities is one of the primary
factors attributed to conflicting reports of TENS efficacy. Therefore, clinicians should strive to apply TENS at the maximally tolerated intensity for each individual person.
~Electrode site placement :
~The intersection of acupuncture and TENS is receiving increasing attention in research. Numerous studies have examined both electro acupuncture and traditional TENS pad electrodes applied over acupuncture sites .Clinically, application of TENS at these acupoints reduces pain and may be more effective than when applied over non-acupoint sites when measuring pain and pain thresholds to heat and pressure in normal subjects , as well as in patient populations when compared with sham TENS. In post-operative hysterectomy subjects, TENS at acupoint sites reduced opioid intake, nausea and dizziness when compared with TENS at non-acupoint sites .
Evidence of TENS for pain management:-
~Acute non-postoperative pain :
A Cochrane review addressing acute pain (i.e., pain less than 12 weeks duration associated with procedures such as cervical laser, venipuncture, sigmoidoscopy screen, postpartum uterine contraction and rib fractures) in adults used a minimum stimulation intensity of ‘strong but comfortable’ as an inclusion factor. However, with 12 studies included ,the authors were unable to make any conclusions due to insufficient evidence .
~Four studies were included in a separate meta-analysis of RCTs where TENS was utilized in a pre-hospital setting for acute pain, (defined as moderate to severe) with TENS delivered by emergency service personnel. All studies found TENS lead to a clinically significant reduction in pain severity as compared with placebo TENS .This review only included studies where TENS was used short term in ambulance responses. These studies were excluded from the Cochrane review of TENS and acute pain due to low stimulation intensity. Thus, short-term use of TENS in ambulance responses the required intensity may be less than that required for chronic or other types of acute conditions. Recent randomized controlled trials for TENS show significant reductions in postpartum pain [90]) and pain during wound-care procedures . Interestingly, the mechanical triggers of wound-care procedures are similar to movement pain, supporting the effect of TENS for pain caused by mechanical stimulation, such as muscle movement, pressure, or force.
~Diabetic peripheral neuropathy (DPN) :
In people with painful DPN, TENS may also provide benefit. A meta-analysis including three RCTs (n = 78) reported reduction of pain that was significantly greater than placebo TENS following 4–6 weeks of treatment In addition, secondary outcomes of overall improvement in DPN symptoms (hyperalgesia, numbness, and quality of life) were significantly greater for active TENS groups when compared with placebo Therefore, there is support for the use of TENS in reducing
pain and improving quality of life in people with painful DPN.
~Fibromyalgia (FM) :
Recent evidence suggests that TENS can be effective for people with fibromyalgia. Although there have been several randomized controlled-trials , no systematic reviews have been published and the quality of these studies and the intervention have varied significantly. Two trials compared TENS to a placebo and used an adequate dose. Dailey et al. showed a one-time session of TENS (using a maximum tolerable intensity) significantly decreased movement pain and hyperalgesia. No changes were observed in resting pain Lauretti et al. showed TENS using a strong intensity (60 mA) at two sites and at one site produced a significant decrease in pain at rest compared with placebo when applied over a seven day period. Two additional studies show reductions in pain with strong but comfortable intensity HF TENS compared with warmth therapy and to a no TENS group. Thus, when used at a strong but comfortable sensation, TENS may be effective for both resting and movement
pain in people with fibromyalgia.
~Neuropathic pain :
TENS may offer relief to people with neuropathic pain and complex regional pain syndrome. A crossover design trial investigating neuropathic pain in people with spinal cord injury, found a favorable effect of both LF and HF TENS (LF TENS 38%; HF TENS 29%) on a global relief scale and 25% of subjects requested a unit for further treatment. However, this study did not compare against a placebo or control group, intensity was not reported, and there were a low number of study participants (n = 24).
A more recent study reports LF TENS provided significant reduction in pain when compared with placebo TENS in people with spinal cord injury. Here the parameters of 4 Hz and 200 µs were applied at sites below the level of injury at a set intensity of 50 mA Thus; LF TENS may be most effective for pain in people with spinal cord injury.
*TENS machine or EMS electrodes should NEVER be placed:
~Across your eyes (intraocular pressure) or brain.
~On the front of your neck due to the risk of acute hypotension (through a vasovagal reflex) or even a laryngospasm.
~Through the chest (using a front and rear of chest wall electrode positions). Either side of your spinal column is permitted.
~Across an artificial cardiac pacemaker (or another indwelling stimulator, implantable cardioverter- defibrillators (ICDs), including across its leads) due to a risk of interference and failure of the implanted device. Serious accidents have been recorded in cases when this principle was not observed.
~On open wounds or broken skin areas (although it can be placed around wounds.
~Over a malignant tumour (based on experiments where electricity promotes cell growth).
~Directly over the spinal column (although it can be placed either side of your spinal column).
~Over mucosal membranes or internally, except for specific applications of dental, vaginal, and anal stimulation that employ specialised TENS units.
~Head or neck of stroke or epilepsy patients.
~Pregnant uterus.
~On areas of numb skin/decreased sensation TENS should be used with caution because it’s likely less effective due to nerve damage. It may also cause skin irritation due to the inability to feel currents until they are too high.
~Areas of Infection. There’s an unknown level of risk when placing electrodes over an infection (possible spreading due to muscle contractions). Cross contamination with the electrodes themselves is of greater concern eg dermatological conditions.
Setting the Mode:-
~Three mode settings, Normal, Burst and Modulation.
~Constant Stimulation at the frequency and pulse width setting. Most commonly used or acute pain relief via a gating effect.
~Modulation. The frequency varies between different settings and uses a cyclical to help reduce nerve adaptation. This is useful for acute and chronic pain relief.
~Burst Mode is useful in chronic pain relief. The unit will send through a burst of pain relieving power.
~Setting the Pulse Rate (Frequency)Pulse Rate is the number of electrical pulses you will feel in one second. Frequency is measured in Hertz (Hz). Pain relief can occur at various frequencies. Acute pain is usually most effective between 80 and 120 Hz. Chronic pain can also benefit from lower settings 2 to 10Hz that stimulates an endorphin release. A setting between 35 and 50Hz is commonly used to stimulate muscles for strengthening or even relaxation.
*The following settings are recommended:-
- 80 to 120Hz-acute pain
- 35-50Hz-muscle stimulation
- 2 to 10Hz – chronic pain
*Setting the Pulse Width
These are the ON periods of the current. Generally speaking, pain relief will occur with low to mid time periods. Muscle stimulation requires a longer pulse width to successfully reproduce a muscle contraction.
You can alter the time that each pulse lingers before resetting. The time period is extremely small. It’s measured in microseconds uS (1000th’s of a second). While you may not notice the difference, your nerves can.
*The following setting is recommended:-
~175 to 200uS
You can strengthen the power of your machine by increasing the pulse width.
*What Time Duration Should You Use a TENS Machine?
The following settings are recommended:
Acute pain 20 to 60min up to four times daily
Chronic pain – 20 to 30min up to five times weekly
*How Often Should You Use Your TENS Machine?
You can safely use a TENS machine as often as you like. Usually for 30-60 minutes up to 4 times daily.
TENS can provide relief for up to four hours.
Application of electrodes:-
*Positioning
~The electrodes are self adhesive; discontinue treatment if the resident develops a skin irritation following treatment.
~The electrodes are normally positioned over the area of pain but other more advanced applications may often prove better. Please consult with physio for initial set up of electrode positioning.

*Examples
~Central neck pain
Position each set of electrodes on either side of the neck in the area of discomfort.
~Shoulder pain
Position each set of electrodes above and below the pain site
Position one electrode pad on the neck on the same side as the painful shoulder and the other paired electrode on the painful area; position the other electrode in a similar way
~Knee pain
Position electrodes around the knee joint above and below on each side
~Lower back pain and TENS
Position electrodes on either side of the back at the level of pain
If pain is out to one side position one of the paired electrodes over the site of pain next to the spineand the corresponding electrode close to the spine at the same level; position second electrode near same position.
*Safety:-
There are several anatomical locations where TENS electrodes are contraindicated:
~Over the eyes due to the risk of increasing intraocular pressure
~On the front of the neck due to the risk of an acute hypotension (through a vasovagal response) or
even a laryngospasm.
~Through the chest using an anterior and posterior electrode positions, or other transthoracic applications understood as “across a thoracic diameter”; this does not preclude coplanar applications
~Internally, except for specific applications of dental, vaginal, and anal stimulation that employ
specialized TENS units
~On broken skin areas or wounds, although it can be placed around wounds
~Over a tumor/malignancy (based on in vitro experiments where electricity promotes cell growth)
~TENS used across an artificial cardiac pacemaker (or other indwelling stimulator, including across its leads) may cause interference and failure of the implanted device.
~TENS, “are best avoided” in patients with pacemakers or implantable cardioverter-defibrillators (ICDs).
~The use of TENS is likely to be less effective on areas of numb skin/decreased sensation due to nerve damage. It may also cause skin irritation due to the inability to feel currents until they are too high.There’s an unknown level of risk when placing electrodes over an infection .
~TENS should also be used with caution in people with epilepsy or pregnant women; do not use over area of the uterus as the effects of electrical stimulation over the developing fetus are not known.
~On the front of your neck due to the risk of acute hypotension (through a vasovagal reflex) or even a laryngospasm
~Through the chest (using a front and rear of chest wall electrode positions). Either side of your spinal column is permitted.
~Over a malignant tumour (based on experiments where electricity promotes cell growth).
~Directly over the spinal column (although it can be placed either side of your spinal column).
~On areas of numb skin/decreased sensation TENS should be used with caution because it’s likely less effective due to nerve damage. It may also cause skin irritation due to the inability to feel currents until they are too high.
~Areas of Infection. There’s an unknown level of risk when placing electrodes over an infection (possible spreading due to muscle contractions). Cross contamination with the electrodes themselves is of greater concern. Patients who are non compliant or have dementia.
~TENS should also be used with caution in people with epilepsy or pregnant women; do not use over area of the uterus as the effects of electrical stimulation over the developing fetus are not known.
Other Electrotherapy related post :







7 Comments