Use Of Ultrasound in Physiotherapy: Indication, Contraindication, Precaution
Table of Contents
What is Ultrasound Therapy in physiotherapy?
Ultrasound therapy is a non-invasive treatment that uses sound waves to heal soft tissues and reduce pain.
Therapeutic ultrasound is a modality that has been used by physiotherapists. Ultrasound is applied using the head of an ultrasound probe that is placed in direct contact with your skin via a transmission coupling gel.
It is mainly used for its non-thermal effect where high-frequency sound waves cause vibrations and movement of cellular fluids. benefits of ultrasound therapy include improving the healing rate of certain soft tissues. Ultrasound (US) is a form of MECHANICAL energy, not electrical energy. Mechanical vibration at increasing frequencies is known as sound energy.
The normal human sound range is from 16Hz to something approaching 15-20,000 Hz (in children and young adults). Beyond this upper limit, the mechanical vibration is known as ULTRASOUND. The frequencies used in therapy are typically between 1.0 and 3.0 MHz (1MHz = 1 million cycles persecond). Ultrasonic therapy is treatment given using ultrasound wave emitted through ultrasonic machine.
Ultrasound wave, when given in a controlled condition has found to produce physiological effects in our body which cures many ailments. Ultrasound is actually a sound wave whose frequency is higher than the frequency of audible sound wave. It means that there is certain range of sound wave frequency which human ear can hear. When the frequency exceed this audible range than we call it as ultrasound wave.
Use of Ultrasound Therapy:
~ increases healing rates
~ tissue relaxation
~ tissue heating
~ increases local blood flow
~ scar tissue breakdown.
Effect of Ultrasound therapy:
The effect of ultrasound via an increase in local blood flow can be used to help reduce local swelling and chronic inflammation, and promote bone fracture healing. Ultrasound can also be used to achieve phonophoresis. This is a non-invasive way of administering medications to tissues below the skin; perfect for patients who are uncomfortable with injections. Stimulate the production of collagen (the main protein in tendons and ligaments) during tissue healing.
Which Conditions are treated with US? (indications)
Following are the list of conditions in which Ultrasound therapy treatment are indicated.
~ inflammation(Bursitis or tendonitis)
~ chronic pain
~ Muscle Strain and tears
~ ligament and tendon injuries
~ non-acute joint swelling and muscle spasm.
~ Tightness or contractures (to improve range of motion)
~ Frozen shoulder
~ Wound healing
Which body parts we can use for ultra-sonic therapy?
~ Muscle pain.
~ Trigger points.
~ Soften the surgical scar.
~ Softening the tendon after tendon transplant.
~ Plantar fascitis.
~ Carpal tunnel syndrome.
What is the condition where you need to avoid it?
Following the list of conditions in which Ultrasound therapy are contraindicated means you should avoid use of Ultrasound therapy.
~ Tumor.
~ Pregnancy.
~ Over the metal implants.
~ Knee replacement.
~ Hip replacement.
~ Pacemaker.
~ Eyes.
~ Directly on open wounds or active infections
~ Over metastatic lesions
~ On patients with impaired sensation
~ Directly on metal implants
~ Near a pacemaker or any other device that generates a magnetic field
~ During pregnancy (except in the instance of diagnostic sonography)
~ Additionally, ultrasound should not be applied over: ~ The eye ~ The gonads ~ Active epiphysis in children.
Precautions:
~Always use the lowest intensity which produces a therapeutic response
~The head of the applicators should be moving throughout the treatment
.~The ultrasound beam (treatment head) should be perpendicular to the treatment area for best results.
~All parameters (intensity, duration, and mode) need to be considered carefully for desired therapeutic effects. Consider using the lowest intensity to produce a therapeutic response.
How Does an Ultrasound Work?
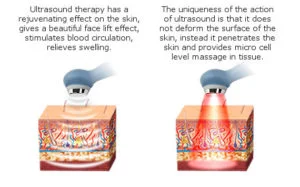
~The ultrasound waves are generated by a piezoelectric effect caused by the vibration of crystals within the head of the probe. The ultrasound waves that pass through the skin cause a vibration of the local soft tissues. This vibration or cavitation can cause a deep heating locally though usually no sensation of heat will be felt by the patient. In situations where a heating effect is not desirable, such as a fresh injury with acute inflammation, the ultrasound can be pulsed rather than continuously transmitted.
Therapeutic effect of Us:
~The therapeutic effects of US are generally divided into: THERMAL & NON-THERMAL.
(1) In thermal mode, US will be most effective in heating the dense collagenous tissues and will require a relatively high intensity, preferably in continuous mode to achieve this effect. Many papers have concentrated on the thermal effectiveness of ultrasound, and much as it can be used effectively in this way when an appropriate dose is selected (continuous mode >0.5 W cm-2), the focus of this paper will be on the non-thermal effects.
~It is too simplistic to assume that with a particular treatment application, there will either be thermal or non-thermal effects. It is almost inevitable that both will occur, but it is furthermore reasonable to argue that the dominant effect will be influenced by treatment parameters, especially the mode of application i.e. pulsed or continuous
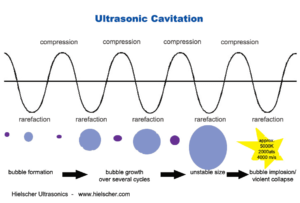
(2) The non-thermal effects of US are now attributed primarily to a combination of CAVITATION and ACOUSTIC STREAMING. There appears to be little by way of convincing evidence to support the notion of MICROMASSAGE though it does sound rather appealing.
*CAVITATION in its simplest sense relates to the formation of gas filled voids within the tissues & body fluids. There are 2 types of cavitation – STABLE & UNSTABLE which have very different effects.
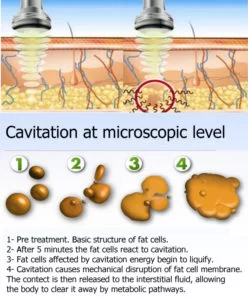
(1)STABLE CAVITATION: does seem to occur at therapeutic doses of US. This is the formation & growth of gas bubbles by accumulation of dissolved gas in the medium. They take apx. 1000 cycles to reach their maximum size. The `cavity’ acts to enhance the acoustic streaming phenomena (see below) & as such would appear to be beneficial.
(2)UNSTABLE (TRANSIENT) CAVITATION: the formation of bubbles at the low-pressure part of the US cycle. These bubbles then collapse very quickly releasing a large amount of energy which is detrimental to tissue viability. There is no evidence at present to suggest that this phenomenon occurs at therapeutic levels if a good technique is used. There are applications of US that deliberately employ the unstable cavitation effect (High Intensity Focussed Ultrasound or HIFU) but it is beyond the remit of this summary.
*ACOUSTIC STREAMING is described as a small-scale eddying of fluids near a vibrating structure such as cell membranes & the surface of a stable cavitation gas bubble (Dyson & Suckling 1978). This phenomenon is known to affect diffusion rates & membrane permeability. Sodium ion permeability is altered resulting in changes in the cell membrane potential. Calcium ion transport is modified which in turn leads to an alteration in the enzyme control mechanisms of various metabolic processes, especially concerning protein synthesis & cellular secretions.
Ultrasound waves:
~FREQUENCY – the number of times a particle experiences a complete compression/rarefaction cycle in 1 second. Typically 1 or 3 MHz (though there are devices that operate in the kHz range – see comments on Low Frequency / Longwave Ultrasound at the end of this paper).
~WAVELENGTH – the distance between two equivalent points on the waveform in the particular medium. In an ‘average tissue’ the wavelength @ 1MHz would be 1.5mm and @ 3 MHz would be 0.5 mm.
~VELOCITY – the velocity at which the wave (disturbance) travels through the medium. In a saline solution, the velocity of US is approximately 1500 m sec-1 compared with approximately 350 m sec-1 in air (sound waves can travel more rapidly in a more dense medium). The velocity of US in most tissues is thought to be similar to that in saline.
~These three factors are related, but are not constant for all types of tissue. Average figures are most commonly used to represent the passage of US in the tissues. Typical US frequencies from therapeutic equipment are 1 and 3 MHz though some machines produce additional frequencies (e.g. 0.75 and 1.5 MHz) and the ‘Longwave’ ultrasound devices operate at several 10’s of kHz (typically 40-50,000Hz – a much lower frequency than ‘traditional US’ but still beyond human hearing range.
~The mathematical representation of the relationship is V = F.l where V = velocity, F = frequency and l is the wavelength.
~Ultrasound Beam, Near Field, Far Field and Beam Non Uniformity
~The US beam is not uniform and changes in its nature with distance from the transducer. The US beam nearest the treatment head is called the NEAR field, the INTERFERENCE field or the Frenzel zone. The behaviour of the US in this field is far from regular, with areas of significant interference. The US energy in parts of this field can be many times greater than the output set on the machine (possibly as much as 12 to 15 times greater). The size (length) of the near field can be calculated using r2/l where r= the radius of the transducer crystal and l = the US wavelength according to the frequency being used (0.5mm for 3MHz and 1.5mm for 1.0 MHz).
~The result of the combined effects of stable cavitation and acoustic streaming is that the cell membrane becomes ‘excited’ (up-regulates), thus increasing the activity levels of the whole cell. The US energy acts as a trigger for this process, but it is the increased cellular activity which is in effect responsible for the therapeutic benefits of the modality.
Ultrasound frequency:
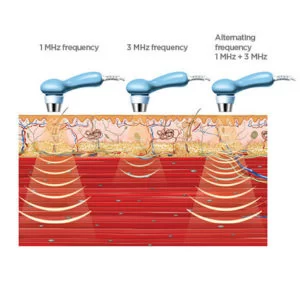
~There is two different form of ultrasound frequency used for therapy purpose. One is 1 MHz frequency and another is 3 MHz. This two different frequency is generated by two different ultrasound head. depending on the site of body illness the types of frequency is selected.
~1 MHz is used to treat deeper tissues and 3 MHz is used to treat superficial tissues.
How ultrasound is generated?
A typical ultrasound machine consists of a machine with all its control switches. It is connected to a transducer head through a thick wire. From the machine we can control the intensity and frequency of ultrasound generated. It is adjusted according to the need of patient. But, it is the transducer head that comes in direct contact with the patient body.
This transducer head produces the wave. The transducer head consists of a special material which has piezoelectric properties. It means when a high frequency electric current passes through this material it compresses and expands with the wave of alternating current. When this material expands, it pushes the substance in front of it which produces compression phase. when it contracts it rarefies the substance in front of it which in turns produces rarefaction phase. So, there is continuous production of wave with alternate compression and rarefaction phase. The following animation makes this point clearer.
Sound waves are LONGITUDINAL waves consisting of areas of COMPRESSION and RAREFACTION. Particles of a material, when exposed to a sound wave will oscillate about a fixed point rather than move with the wave itself. As the energy within the sound wave is passed to the material, it will cause oscillation of the particles of that material. Clearly any increase in the molecular vibration in the tissue can result in heat generation, and ultrasound can be used to produce thermal changes in the tissues.
Ultrasound Transmission through the Tissues:
All materials (tissues) will present an impedance to the passage of sound waves. The specific impedance of a tissue will be determined by its density and elasticity. In order for the maximal transmission of energy from one medium to another, the impedance of the two media needs to be as similar as possible.
Clearly in the case of US passing from the generator to the tissues and then through the different tissue types, this can not actually be achieved. The greater the difference in impedance at a boundary, the greater the reflection that will occur, and therefore, the smaller the amount of energy that will be transferred. The difference in impedance is greatest for the steel/air interface which is the first one that the US has to overcome in order to reach the tissues.
To minimize this difference, a suitable coupling medium has to be utilized. If even a small air gap exists between the transducer and the skin the proportion of US that will be reflected approaches 99.998% which means that there will be no effective transmission.
~The absorption of US energy follows an exponential pattern – i.e. more energy is absorbed in the superficial tissues than in the deep tissues. In order for energy to have an effect it must be absorbed, and at some point this must be considered in relation to the US dosages applied to achieve certain effects Because the absorption (penetration) is exponential, there is (in theory) no point at which all the energy has been absorbed, but there is certainly a point at which the US energy levels are not sufficient to produce a therapeutic effect.
As the US beam penetrates further into the tissues, a greater proportion of the energy will have been absorbed and therefore there is less energy available to achieve therapeutic effects. The half value depth is often quoted in relation to US and it represents the depth in the tissues at which half the surface energy is available. These will be different for each tissue and also for different US frequencies. The table below gives some indication of typical (or average) half value depths for therapeutic ultrasound.
1 MHz 3 MHz
Muscle 9.0 mm 3.0 mm
Fat 50.0 mm 16.5 mm
Tendon 6.2 mm 2.0 mm
~As it is difficult, if not impossible to know the thickness of each of these layers in an individual patient, average half value depths are employed for each frequency:
3 MHz 2.0 cm
1 MHz 4.0 cm
~These values (after Low & Reed) are not universally accepted (see Ward 1986) and some research (as yet unpublished)suggests that in the clinical environment they may be significantly lower.
Depth (cm) 3 MHz 1 MHz
2 50%
4 25% 50%
6
8 25
~To achieve a particular US intensity at depth, account must be taken of the proportion of energy which has been absorbed by the tissues in the more superficial layers. The table gives an approximate reduction in energy levels with typical tissues at two commonly used frequencies, and more detailed information is found in the dose calculation material.
~As the penetration (or transmission) of US is not the same in each tissue type, it is clear that some tissues are capable of greater absorption of US than others. Generally, the tissues with the higher protein content will absorb US to a greater extent, thus tissues with high water content and low protein content absorb little of the US energy (e.g. blood and fat) whilst those with a lower water content and a higher protein content will absorb US far more efficiently. Tissues can be ranked according to their relative tissue absorption and this is critical in terms of clinical decision making.
Best absorption in tendon,ligament,fascia,joint capsule and scar tissue:
~Although cartilage and bone are at the upper end of this scale, the problems associated with wave reflection mean that the majority of US energy striking the surface of either of these tissues is likely to be reflected. The best absorbing tissues in terms of clinical practice are those with high collagen content – LIGAMENT, TENDON, FASCIA, JOINT CAPSULE, SCAR TISSUE. The application of therapeutic US to tissues with a low energy absorption capacity is less likely to be effective than the application of the energy into a more highly absorbing material.
~The physiological effects of ultrasound are almost identical to those of Pulsed Shortwave and LASER therapy – the key difference however, is that ultrasound energy is preferentially absorbed in different tissue to the other modalities – as summarised in the adjacent diagram.
Pulsed ultrasound:
~Low-intensity pulsed ultrasound (LIPUS) is a medical technology, generally using 1.5 MHz frequency pulses, with a pulse width of 200 µs, repeated at 1 kHz, at a spatial average and temporal average intensity of 30 mW/cm2. As of 2009 research for the use of LIPUS to treat soft tissue injuries were in the early stages. Until recently, the pulse duration (the time during which the machine is on) was almost exclusively 2ms (2 thousandths of a second) with a variable off period.
Some machines now offer a variable on time though whether this is of clinical significance has yet to be determined. Typical pulse ratios are 1:1 and 1:4 though others are available (see dose calculations). In 1:1 mode, the machine offers an output for 2ms followed by 2ms rest. In 1:4 mode, the 2ms output is followed by an 8ms rest period.
~Low intensity pulsed ultrasound has been proposed as a therapy to support bone healing after fractures, osteotomies, or delayed healing. The effects of pulsed US are well documented and this type of output is preferable especially in the treatment of the more acute lesions. Some machines offer pulse parameters that do not appear to be supported from the literature (e.g. 1:9; 1:20). Some manufacturers describe their pulsing in terms of a percentage rather than a ratio (1:1 = 50% 1:4 = 20% etc). The proportion of time that the machine is ON compared with OFF is a relevant factor in dosage calculations and further details are included in the dose calculation support material.
Pulse Frequency:
~A point of confusion amongst many therapists is the ‘frequency’ facility offered on some ultrasound machines. The pulse ratio (duty cycle) is at say 1:4 (20%), but there is an option to alter the pulse frequency (i.e. how many ultrasound pulses are delivered per second). This is achieved by adjusting the DURATION of the pulses. Typically, these are at 2ms, thus on a 1:4 ratio, the machine is ON for 2ms and then OFF for 8ms. It takes 10ms to complete one ‘cycle’ (ON : OFF), and thus 100 such cycles are completed in a second, so the machine claims to deliver ultrasound at 100Hz. If the pulse duration is increased from 2ms to say 4ms, then on a 1:4 ratio, the machine will be ON for 4ms followed by 16ms OFF, thus taking 20ms to complete a cycle and hence only 50 such cycles being delivered per second and the setting on the machine will be for ultrasound pulsing at 50Hz. There is no evidence that I can find to suggest that one mode of operation has any clinical advantage over another. The 2ms pulse time is ‘normal’ and is encountered on most machines (which effectively means that 100 pulses of ultrasound energy will be delivered per second.
INFLAMMATION:
~During the inflammatory phase, US has a stimulating effect on the mast cells, platelets, white cells with phagocytic roles and the macrophages For example, the application of ultrasound induces the degranulation of mast cells, causing the release of arachidonic acid which itself is a precursor for the synthesis of prostaglandins and leukotreine – which act as inflammatory mediators. By increasing the activity of these cells, the overall influence of therapeutic US is certainly pro-inflammatory rather than anti-inflammatory. The benefit of this mode of action is not to ‘increase’ the inflammatory response as such (though if applied with too greater intensity at this stage, it is a possible outcome , but rather to act as an ‘inflammatory optimiser’ The inflammatory response is essential to the effective repair of tissue, and the more efficiently the process can complete, the more effectively the tissue can progress to the next phase (proliferation). Studies which have tried to demonstrate the anti-inflammatory effect of ultrasound have failed to do so (e.g.El Hag et al 1985 Hashish 1986, 1988), and have suggested that US is ineffective. It is effective at promoting the normality of the inflammatory events, and as such has a therapeutic value in promoting the overall repair events. A further benefit is that the inflammatory chemically mediated events are associated with stimulation of the next (proliferative) phase, and hence the promotion of the inflammatory phase also acts as a promoter of the proliferative phase.
PROLIFERATION:
~During the proliferative phase (scar production) US also has a stimulative effect (cellular up regulation), though the primary active targets are now the fibroblasts, endothelial cells and myofibroblasts. These are all cells that are normally active during scar production and US is therefore pro-proliferative in the same way that it is pro-inflammatory – it does not change the normal proliferative phase, but maximizes its efficiency – producing the required scar tissue in an optimal fashion.demonstrated that low dose pulsed ultrasound increases protein synthesis and several research groups have demonstrated enhanced fibroplasia and collagen synthesis. Recent work has identified the critical role of numerous growth factors in relation to tissue repair, and some accumulating evidence has identified that therapeutic US has a positive role to play in this context.
REMODELLING:
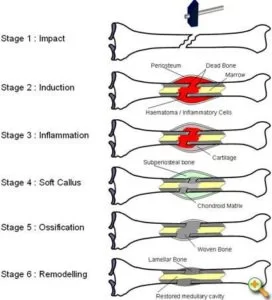
~During the remodelling phase of repair, the somewhat generic scar that is produced in the initial stages is refined such that it adopts functional characteristics of the tissue that it is repairing. A scar in ligament will not ‘become’ ligament, but will behave more like a ligamentous tissue. This is achieved by a number of processes, but mainly related to the orientation of the collagen fibres in the developing scar. and also to the change in collagen type, from predominantly Type III collagen to a more dominant Type I collagen. The remodelling process is certainly not a short duration phase – research has shown that it can last for a year or more – yet it is an essential component of quality repair. The application of therapeutic ultrasound can influence the remodelling of the scar tissue in that it appears to be capable of enhancing the appropriate orientation of the newly formed collagen fibres and also the collagen profile change from mainly Type III to a more dominant Type I construction, thus increasing tensile strength and enhancing scar mobility. Ultrasound applied to tissues enhances the functional capacity of the scar tissues.
The application of ultrasound during the inflammatory, proliferative and repair phases is not of value because it changes the normal sequence of events, but because it has the capacity to stimulate or enhance these normal events and thus increase the efficiency of the repair phases.
It would appear that if a tissue is repairing in a compromised or inhibited fashion, the application of therapeutic ultrasound at an appropriate dose will enhance this activity. If the tissue is healing ‘normally’, the application will, it would appear, speed the process and thus enable the tissue to reach its endpoint faster than would otherwise be the case. The effective application of ultrasound to achieve these aims is dose-dependent.
FAQs
The most common musculoskeletal diseases that have been traditionally treated with continuous therapeutic ultrasound therapy include osteoarthritis, soft tissue shoulder pathology, and myofascial pain.
If used for an extended period of time, the skin may become superficially burned. The ultrasound wand’s continuous motion can prevent this. Depending on the length of exposure, mechanical therapeutic ultrasounds may result in internal bleeding or scarring.
While some studies have found that it can reduce pain, others have found no significant difference in the efficacy of ultrasonography compared to other forms of therapy. In some circumstances, such as with extremely young children and cancer patients, ultrasound should not be used.
There are no restrictions on the frequency at which ultrasound therapy can be performed. During treatment, we typically utilize it for five minutes at a time.
Contrary to several other types of scans, like CT scans, ultrasonic scans don’t expose the patient to radiation. While both external and internal ultrasound scans are normally painless and have no negative side effects, you could feel some discomfort as the probe is placed against your skin or put into your body.







5 Comments