Osteoporosis
Table of Contents
INTRODUCTION:
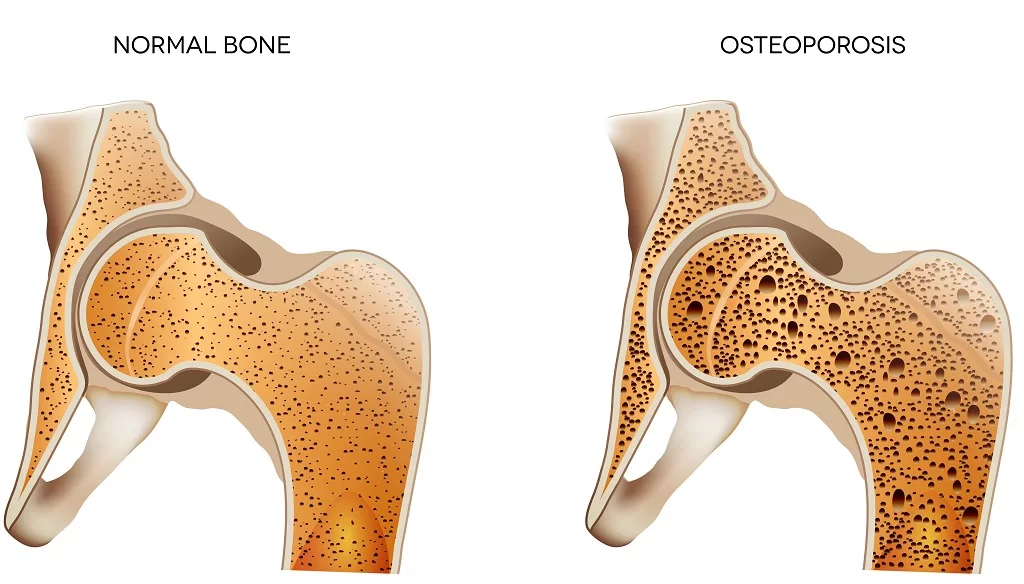
“Osteoporosis is a disease of bones in which a decrease in bone density (mass and quality).”Osteoporosis” literally means “porous bones.
Bone is a living tissue that is constantly being broken down and replaced. Osteoporosis occurs when the creation of new bone doesn’t keep up with the removal of old bone.
People with osteoporosis have bones that are weak and break easily.
The bones become weaker, increasing the risk of fractures, especially in the hip, spinal vertebrae, and wrist.
Osteoporosis is called a “silent” disease. You may have bone loss for many years without any symptoms until you break a bone.
A broken bone can cause severe pain and disability. It can make it harder to do daily tasks on your own, such as walking.
Bone density peaks when a person is in their late 20s. After the age of around 35 years, the bone starts to become weaker. As we age, bone breaks down faster than it builds. If this happens excessively, osteoporosis results.
TYPES
There are two types of osteoporosis:
primary and secondary.
Primary osteoporosis is not related to other diseases or conditions and is the more common of the two. It is most common in post-menopause women or older men, but can occur at any age. In cases of primary osteoporosis, either the condition is caused by age-related bone loss (sometimes called senile osteoporosis) or the cause is unknown (idiopathic osteoporosis).
In cases of secondary osteoporosis, the loss of bone mass is caused by certain lifestyle behaviors, diseases, or medications. The most common causes of secondary osteoporosis in men include exposure to glucocorticoid medications, hypogonadism (low levels of testosterone), alcohol abuse, smoking, gastrointestinal disease, hypercalciuria, and immobilization.
RISK FACTORS/CAUSES
FEMALES:
Osteoporosis is more common in women than in men—about 80% of cases affect women.
OLDER AGE:
As we age, our bones naturally lose some density and become weaker. That doesn’t mean that every older person gets osteoporosis, but it does mean your chances of developing the disease increase with age.
FAMILY HISTORY:
Studies show that if either of your parents had osteoporosis, then you are more likely to get it, too.
HISTORY OF BROKEN BONES:
Even if you’ve only had one broken bone, it will increase your risk of developing osteoporosis.
SMALL & THIN FRAME:
People with lighter, thinner bones are more prone to osteoporosis. However, having a larger frame is not a defense against the disease.
WHITE OR OF ASIAN OR LATINE HERITAGE:
Osteoporosis affects all races and ethnicities, but if you are white or of Asian or Latino descent, you have a higher risk.
MENOPAUSE:
Menopause is marked by a steep drop in estrogen, which is a female sex hormone that protects bones. When estrogen levels decrease, bones may lose density and become prone to fractures.
LOW VITAMIN D AND LOW CALCIUM DIET:
It’s important to eat a diet rich in calcium and vitamin D because these nutrients work together to promote healthy bone growth and maintenance. Calcium promotes healthy bones, and vitamin D helps your body effectively absorb calcium.
SEDENTARY LIFESTYLE:
Due to inactivity bones become weak. Exercise helps ward off osteoporosis by strengthening your bones, just as it strengthens your muscles. Strong bones are less likely to fracture.
SMOKING:
If you smoke, your risk for osteoporosis increases for a number of reasons. First, the chemicals found in cigarettes interfere with the normal functioning of your bone cells. Also, smoking may inhibit proper calcium absorption. And finally, smoking prevents estrogen in women from protecting their bones as it should.
ALCOHOL:
Heavy alcohol consumption inhibits normal bone formation by impacting your body’s calcium supply. If you consume alcohol, do so in moderation (less than 2 drinks a day).
MEDICATIONS:
Certain medications, particularly steroids, can weaken your bones. In most cases, you have to use these medications for a long time and in very high doses for them to become a threat to your bones. That’s not to say that these medications are bad for you—they may be essential to treat your respective condition. Don’t stop any treatment or alter the dosage without first consulting your doctor.
SIGN AND SYMPTOMS:
Osteoporosis can be present without any symptoms for decades because osteoporosis doesn’t cause symptoms until bone breaks (fractures). Moreover, some osteoporotic fractures may escape detection for years when they do not cause symptoms. Therefore, patients may not be aware of their osteoporosis until they suffer a painful fracture. The symptom associated with osteoporotic fractures usually is pain; the location of the pain depends on the location of the fracture. The symptoms of osteoporosis in men are similar to the symptoms of osteoporosis in women.
HEIGHT LOSS:
Under normal circumstances, height loss is a part of growth. As a person ages, the discs in the spinal cord shink and contract, and this causes loss of height. But a person inflicted with this disease might experience height loss suddenly.
Episodic, acute low thoracic/high lumbar pain
FRACTURES:
Fractures are the most dangerous aspect of this disease. It can cause debilitating, acute and chronic pain. It might be hard to link fractures to this disease as these are asymptomatic. In some cases, the fractures of the long bones acutely impair mobility and might necessitate surgery.
wrist fractures:
A broken wrist is the first symptom that suggests the presence of osteoporosis. Women are prone to wrist fractures after menopause. Usually, people shoot their arms to the front as a reflex action to stop their fall. Healthy bones should be able to resist a simple fall but a fracture is an indication of osteoporosis.
spinal fractures:
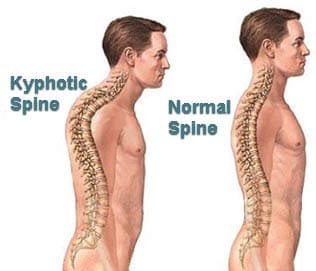
Fractures of the spine (vertebra) can cause severe “band-like” pain that radiates from the back to the sides of the body. Over the years, repeated spinal fractures can lead to chronic lower back pain as well as loss of height and/or curving of the spine due to collapse of the vertebrae. The collapse gives individuals a hunched-back appearance of the upper back, often called a “dowager hump” because it is commonly seen in elderly women.
Dowager’s hump:
Spinal compression fractures may result in loss of height with a stooped posture called a dowager’s hump.
Stress fractures:
A fracture that occurs during the course of normal activity is called a minimal trauma, or stress fracture. For example, some patients with osteoporosis develop stress fractures of the feet while walking or stepping off a curb.
Hip fractures:
Hip fractures typically occur as a result of a fall. With osteoporosis, hip fractures can occur as a result of trivial slip-and-fall accidents. Hip fractures also may heal slowly or poorly after surgical repair because of poor healing of the bone.
RARE SYMPTOMS:
There are a few other signs that you may be experiencing a loss of bone density.
Loss of Grip Strength:
There’s increasing evidence that a loss of grip strength is a good predictor of osteoporosis. This could be attributed to other issues, like osteoarthritis for example, but should be brought to your doctor’s attention nonetheless.
Loss of Fitness:
there is an overall decrease in the strength of the body. a person becomes easily fatigued.
Periodental disease:
Some research suggests an association between periodontal disease (receding gums, tooth loss, etc.) and osteoporosis. Other studies have found, though, that the association isn’t significant. Certain osteoporosis treatments can adversely affect oral health, so it’s important to discuss this potential side effect with your doctor.
DIAGNOSIS:
To diagnose osteoporosis and assess your risk of fracture and determine your need for treatment, your doctor will most likely order a bone density scan.
Bone Density Test (DEXA SCAN: Dual-energy X-ray absorptiometry):
The most common test used is a bone density test, which is the only test that can detect osteoporosis before a fracture occurs. There are two types of bone density tests: Central DXA and Screening Tests. Central DXA uses a dual-energy absorptiometry machine to test the bone density of the hip and spine. If testing can’t be done to the hip and spine then it is recommended to test the radius of the forearm. Central DXA is the preferred method because it measures bone density at the hip and spine where bone loss occurs most rapidly.
Screening Tests, also called peripheral tests, measure bone density in the lower arm, wrist, finger, or heel. These are useful when Central DXA testing is not possible. Screening tests cannot accurately diagnose osteoporosis or measure how well medication is working.
Bone density test results are reported using T-scores. T-scores are relative to how much higher or lower your bone density is compared to that of a healthy 30-year-old adult.

The following procedures can be performed to determine bone injury or fractures due to osteoporosis:
Bone x-ray:
Bone x-ray produces images of bones within the body, including the hand, wrist, arm, elbow, shoulder, foot, ankle, leg (shin), knee, thigh, hip, pelvis, or spine. It aids in the diagnosis of fractured bones, which are sometimes a result of osteoporosis.
CT scan of the spine:
CT scanning of the spine is performed to assess for alignment and fractures. It can be used to subjectively measure bone density and determine whether vertebral fractures are likely to occur. This technique is called quantitative CT (QCT).
MRI of the spine:
Magnetic resonance imaging of the spine is performed to evaluate vertebral fractures for evidence of underlying disease, such as cancer, and to assess the newness of the fracture.
Laboratory Tests:
Some of these tests can help to identify if you have any other medical conditions that could contribute to osteoporosis, which would be called secondary osteoporosis.
Blood Calcium levels
24-hour urine calcium measurement
Thyroid function tests
Parathyroid hormone levels
Testosterone levels in men
25-hydroxyvitamin D test to determine whether the body has enough vitamin D
TREATMENT
1-DIET(CALCIUM AND VITAMIN D)
Food sources of calcium include nonfat milk, low-fat yogurt, plant-based milk, or orange juices that are fortified with calcium, broccoli, cauliflower, salmon, tofu, and leafy green vegetables.
Get 1,000 milligrams of calcium each day if you’re aged 19-50. You need 1,200 milligrams per day if you’re a woman age 51 or older, or a man age 71 and older.
It’s best to get your calcium from foods. If you want to take supplements, talk to your doctor first.
You can get vitamin D from fortified foods and also from sunshine. But it gets harder to make vitamin D as you get older and during winter. Supplements help.
2-MEDICATIONS:
Your doctor may prescribe medications to treat osteoporosis, too.
Some of these drugs target the breakdown of bones. They slow down bone loss. Your doctor may call these meds bisphosphonates. They include:
Alendronate (Binosto, Fosamax)
Ibandronate (Boniva)
Risedronate (Actonel, Atelvia),
Zoledronic acid (Reclast, Zometa),
here’s also a biologic drug — denosumab (Prolia, Xgeva) — for osteoporosis. It turns off the process that makes the body break down bones.
3-PHYSIOTHERAPY TREATMENT:
AIMS:
1- EDUCATION TO PATIENT ABOUT THE CONDITION
2- PAIN RELIEF AND RELAXATION TRAINING
3- STRENGTHENING EXERCISES
5- POSTURAL CORRECTION
6- BALANCING EXERCISES
7- ADVISES
PLANS:
1-EDUCATION:
first of all, educate the patient about a condition what is it, and how it can be prevented. then explain to the patient the role of physiotherapy and physical activity in osteoporosis.
2-PAIN RELIEF:
Heat and Ice:
Heat in the form of warm showers or hot packs can relieve chronic pain or stiff muscles.
Cold packs or ice packs provide pain relief by numbing the pain-sensing nerves in the affected area. Cold also helps reduce swelling and inflammation.
Depending on which feels better, apply heat or cold for 15 to 20 minutes at a time to the area where you feel the pain. To protect your skin, place a towel between your skin and the source of the cold or heat.
Transcutaneous Electrical Nerve Stimulation (TENS):
TENS units are small devices that send electrical impulses to certain parts of the body to block pain signals. Two electrodes are placed on the body where you are experiencing pain. The electrical current that is produced is very mild, but it can prevent pain messages from being transmitted to the brain. Pain relief can last for several hours. Some people may use a small, portable TENS unit that hooks onto a belt for more continuous relief.
MASSAGE THERAPY:
Massage therapy can be light, slow, circular motion with the fingertips or a deep, kneading motion that moves from the center of the body outward toward the fingers or toes. Massage relieves pain, relaxes stiff muscles, and smoothes out muscle knots by increasing the blood supply to the affected area and warming it. The person doing the massage uses oil or powder so that her or his hands slide smoothly over the skin.
Massage can also include gentle pressure over the affected areas or hard pressure over trigger points in muscle knots.
Note: Deep muscle massage should not be done near the spine if you have spinal osteoporosis. Light, circular massage with fingers or the palm of the hand is best in this case.
Braces and Supports
Spinal supports or braces reduce pain and inflammation by restricting movement. Following a vertebral fracture, a back brace or support will relieve pain and allow you to resume normal activities while the fracture heals. However, continuous use of a back support can weaken back muscles. For this reason, exercises to strengthen the muscles in the back should be started as soon as possible.
Relaxation Training
Relaxation involves concentration and slow, deep breathing to release tension from muscles and relieve pain. Learning to relax takes practice, but relaxation training can focus attention away from pain and release tension from all muscles. Relaxation tapes are widely available to help you learn these skills.
Exercises for Osteoporosis Video
3-STRENGTHENING EXERCISE:
A: AEROBIC EXERCISE:
Brisk walking
Climbing stairs
Dancing
Hiking
Jogging
Jumping rope
Step aerobics
Tennis or other racquet sports
Swimming or water aerobics
Cycling
B: STRENGTH TRAINING:
Weightlifting: dumbbells, barbells, machines, bodyweight exercises
Elastic exercise bands
Free weights
Weight machines
Add strength-training exercises to your workouts 2 to 3 days per week
C: WEIGHT-BEARING EXERCISES:
JOG IN PLACE:

Considering the needs of an aging body, if low-impact movement serves you better, just march with high knees in place for 1 minute.
PUNCHING:

Punching is a great way to warm up the upper body and get the blood pumping all over. Perform for 1 minute.
A) Stand with feet slightly wider than shoulder-distance apart and bend knees slightly. Tighten the core to keep your center still.
B) Punch out one arm at a time at a steady pace.
BASIC SQUAT:
Finish your warm up with the basic squat. Try to get your glutes to drop as low as possible to keep your hip flexors mobile and prevent you from taking on the old-age “shuffle” when you walk.

Bend your knees and extend your buttocks backward as if you are going to sit back into a chair. Make sure that you keep your knees on your toes and your weight in your heels. Rise back up.
SHOULDER OVERHEAD PRESS:
Press dumbbells slowly up until arms are straight. Slowly return to the starting position with control. Repeat for the desired number of reps.
Make it Harder: To work harder and improve balance, stand on one foot while performing half, then the other foot.
Start with feet hip distance apart. Bring elbows out to the side, creating a goal post position with arms, dumbbells are at the side of the head, and abdominals are tight.
Perform 8-12 Repetitions. Rest for 1 minute.
BIRD DOG:
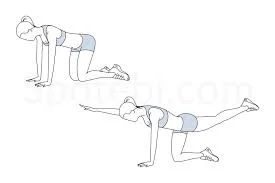
Kneel on the mat on all fours. Reach one arm long, draw in the abdominals, and extend the opposite leg long behind you.
Repeat on the other side.
Perform 8-10 per side. Move slow and steady, holding the arm and leg out momentarily before switching. Rest 1 minute
BRIDGING:
Lie on your back with bent knees hip distance apart and feet flat on the mat stacked under the knees.
Engage the core and squeeze your glutes as you lift your hips to a bridge. Hold, squeezing tight, and return to the mat with control.
Perform 8-12 Repetitions. Rest for 1 Minute.
4- POSTURAL CORRECTION:
FOR STOOP POSTURE: in the case of spinal osteoporosis posture becomes stoop is a rounded and protracted shoulder with a forward head.
so we can give neck extensor isometrics
pectoral stretch (butterfly)
5- BALANCING EXERCISE:
A-HEEL RAISE:–
stand with the support of the chair(behind the chair) slowly raise your heel and maintain your balance on your toes.
do for 1 min then increase.
In progression, do it without the support of a chair.

B-TOE RAISE:
stand with the support of a chair (behind the chair) slowly raise your toes and maintain your balance on your heels.
do it for 1 min then increase.
In progression, do it without the support of a chair.
C-ONE LEG STAND:

stand with the support of a chair lift one leg and maintain balance on another leg.
do it for 1 min then increase.
In progression, do it without the support of a chair.
D-WOBBLE BOARD EXERCISE:
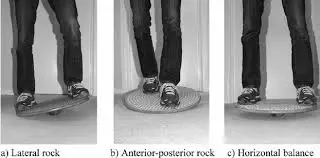
stand on a wobble board with support on both sides and then rock laterally and then anterior-posteriorly.
In both directions, do it for 1-1 min.
In progression, do it without support.
6- ADVISES:
- Take a proper diet that is a vitamin D and calcium-rich diet.
- prevent frequent falls to prevent fractures.
- Do exercise regularly to maintain physical fitness.
- stop smoking, tobacco chewing, alcohol, etc.
- Avoid sudden forces on bones because it leads to fractures.




12 Comments