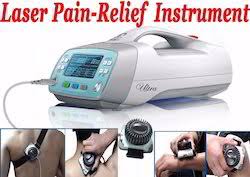
Use of LASER in Physiotherapy
*Introduction:-
Table of Contents
What is LASER therapy?
~Laser therapies are medical treatments that use focused light. Unlike most light sources, light from a laser (which stands for light amplification by stimulated emission of radiation) is tuned to specific wavelengths. This allows it to be focused into powerful beams. Laser light is so intense that it can be used to shape diamonds or cut steel.
~Laser Therapy treatment is a non-invasive therapy that makes use of intense beams of light of specific wavelengths to help reduce pain related to your injury. LASER stands for ‘Light Amplification by Stimulated Emission of Radiation.’
~When it comes to therapeutic use, lasers are often referred to as Cold Lasers, Low-Level Laser Therapy (LLLT) or High Power Laser Therapy (HPLT).The Low-Level Laser Therapy utilizes red (and close to red) infrared light on areas of injury or wounds in order to mend the soft tissue and also to give relief from acute and chronic pain.
~When the lights of specific wavelengths are targeted to a particular area of body, physiological changes take place in the cells. This process is known as photobiomodulation.
~In simple yet realistic terms, the laser can be considered to be a form of light amplifier – it provides enhancement of particular properties of light energy.
~Laser light will behave according to the basic laws of light, in that it travels in straight lines at a constant velocity in space. It can be transmitted, reflected, refracted and absorbed. It can be placed within the electromagnetic spectrum according to its wavelength/frequency which will vary according to the particular generator under consideration.
~There are several aspects of laser light which are deemed to be special and are often referred to in the literature. These include monochromacity, coherence and polarisation. There remains some doubt as to exactly how essential these particular aspects of laser light are in relation to the therapeutic application of this energy form.
~Monochromacity is probably the most important factor, as many of the therapeutic effects have been noted in various trials with light which is non-coherent. Additionally, it is thought that the polarisation is soon lost within the tissues & may therefore be less important than was thought at first.
Types of Laser:-
(1) Power Laser – It is used for the destructive or surgical purpose.
(2) Soft Laser – It has a very superficial effect and is used principally for treating the skin.
(3) Mid Laser – Its depth of penetration is sufficient to produce the biological effect on deeper tissue without damaging.
Physiological effect of LASER:-

~Wound healing
~Analgesic effect
~Anti-inflammatory
~Counterirritant
~Normalization of tissue
~Endorphin release
~Re-absorption of edema fluid.
~Penetration
~Absorption
~Dehydration
~Coagulation of proteins.
Indication of LASER:-
~Laser therapy indication Open lesions
~Incisions
~Decubitus ulcers
~Lacerations
~Diabetic ulcers
~Burns
~Chronic and acute pain especially those of musculoskeletal origin. e.g- osteoarthritis, sprains, tendinitis, ~contusions, lumbago, neuralgia, neuritis.
~Restricted joint ranges of motion.

Method of LASER:-
Contraindication of LASER:-
~Epileptic patient
~Cardiac patient
~Patient with a pacemaker
~Skin disease
~Pregnant women
~Growing cartilage in children.
~Directly eyes.
Parameters:-
~Most LLLT apparatus generates light in the Red Visible & Near Infra-red bands of the EM spectrum, with typical wavelengths of 600 -1000nm. The mean power of such devices is generally low (1-100mW), though the peak power may be much higher than this.
~The treatment device may be a single emitter or a cluster of several emitters, though it is common for most emitters in a cluster to be non laser type devices. The beam from single probes is usually narrow (Æ1mm-6 or 7mm) at the source. A cluster probe will usually incorporate both higher and lower power emitters of different wavelengths.
~The output may be continuous or pulsed, with narrow pulse widths (in the nano or micro second ranges) and a wide variety of pulse repetition rates from 2Hz up to several thousand Hz. It is difficult to identify the evidence for the use of pulsing from the research literature, though it would appear to be a general trend that the lower puling rates are more effective in the acute conditions whilst higher pulse rates work better in more chronic conditions.
~There is a growing body of support that suggests that the pulsing settings are of secondary importance in terms of clinical doses.
Dose Calculations:-
~Most research groups and many manufacturers, recommend that the dose delivered to a patient during a treatment session should be based on the ENERGY DENSITY rather than the power or other measure of dose. Energy Density is measured in units of Joules per square centimetre (J/cm2).
~One of the most significant inhibitors to the more widespread adoption of laser therapy in the clinical environment relates to the difficulty in getting these ‘effective’ laser doses to work on a particular machine. Few devices enable the practitioner to set the dose in J/cm2. Some will provide Joules, some Watts, some watts/cm-2 etc etc.
~It is currently argued that Joules (i.e. Energy) may in fact be the most critical parameter rather than Energy Density. The debate is not yet resolved, and the energy density will be used here, mainly because the published research almost exclusively cites it, and therefore, it may be of more use when it comes to trying to replicate an evidence based treatment dose.
~Some machines offer ‘on board’ calculations of this dose, whilst other machines require the operator to make some simple calculations based on several considerations:
~output power (Watts)
~irradiation area (cm2)
~time (seconds)
~If PULSED – pulse width, frequency and power settings
~ENERGY DENSITY (J/cm2) = Total amount of energy (J) / Irradiation area (cm2)
~TOTAL ENERGY (J) = Average Power (Watts) x Time (sec)
~AVERAGE POWER (Watts) = Peak power (W) x Frequency (Hz) x Pulse Duration (sec) (PULSED OUTPUT ONLY)
~There are various alternative methods for calculating these doses, but those cited above offer a reasonably simple
method should one be needed.
~Most authorities suggest that the ENERGY DENSITY per TREATMENT SESSION should generally fall in the range of 0.1 – 12.0 J/cm2 though there are some recommendations which go up to 30 J/cm2. It has been previously suggested that a maximal (single treatment) dose of 4 J/cm2 should not be exceeded. The evidence would not support that contention. Again as a generality, lower doses should be applied to the more acute lesions which would appear to be more energy sensitive.
Use of LASER:-
~Laser therapy may be used to:
~shrink or destroy tumors, polyps, or precancerous growths
~treat pain, including back nerve pain
Lasers can have a cauterizing, or sealing, effect and may be used to seal:
~nerve endings to reduce pain after surgery
~blood vessels to help prevent blood loss
~lymph vessels to reduce swelling and limit the spread of tumor cells
~Lasers may be useful in treating the very early stages of some cancers, including:
cervical cancer
penile cancer
vaginal cancer
vulvar cancer
non-small cell lung cancer
basal cell skin cancer
For cancer, laser therapy is usually used alongside other treatments, such as surgery, chemotherapy, or radiation.
Laser therapy is also used cosmetically to:
remove warts, moles, birthmarks, and sun spots
remove hair
lessen the appearance of wrinkles, blemishes, or scars
remove tattoos

Physical Mechanisms :
~According to quantum mechanical theory, light energy is composed of photons or discrete packets of
electromagnetic energy. The energy of an individual photon depends only on the wavelength. Therefore, the energy of a “dose” of light depends only on the number of photons and on their wavelength or color (blue photons have more energy than green photons, that have more energy than red, that have more energy than NIR, etc).
~Photons that are delivered into living tissue can either be absorbed or scattered. Scattered photons will eventually be absorbed or will escape from the tissue in the form of diffuse reflection. The photons that are absorbed interact with an organic molecule or chromophore located within the tissue.

~Because these photons have wavelengths in the red or NIR regions of the spectrum, the chromophores that absorb these photons tend to have delocalized electrons in molecular orbitals that can be excited from the ground state to the first excited state by the quantum of energy delivered by the photon. ~
According to the first law of thermodynamics, the energy delivered to the tissue must be conserved, and three possible pathways exist to account for what happens to the delivered light energy when low level laser therapy is delivered into tissue.
~The commonest pathway that occurs when light is absorbed by living tissue is called internal conversion. This happens when the first excited singlet state of the chromophore undergoes a transition from a higher to a lower electronic state. It is sometimes called “radiationless de-excitation”, because no photons are emitted.
~It differs from intersystem crossing in that, while both are radiationless methods of de-excitation,
the molecular spin state for internal conversion remains the same, whereas it changes for intersystem crossing. The energy of the electronically excited state is given off to vibrational modes of the molecule, in other words, the excitation energy is transformed into heat.
~The second pathway that can occur is fluorescence. Fluorescence is a luminescence or re-emission of light, in which the molecular absorption of a photon triggers the emission of another photon with a longer wavelength.
~The energy difference between the absorbed and emitted photons ends up as molecular vibrations or heat. The wavelengths involved depend on the absorbance curve and Stokes shift of the particular fluorophore.
~The third pathway that can occur after the absorption of light by a tissue chromophore, represents a number of processes broadly grouped under an umbrella category of photochemistry. Because of the energy of the photons involved, covalent bonds cannot be broken. However, the energy is sufficient for the first excited singlet state to be formed, and this can undergo intersystem crossing to the long-lived triplet state of the chromophore.
~The long life of this species allows reactions to occur, such as energy transfer to ground state molecular
oxygen (a triplet) to form the reactive species, singlet oxygen. Alternatively the chromophore triplet state
may undergo electron transfer (probably reduction) to form the radical anion that can then transfer an electron to oxygen to form superoxide.
~Electron transfer reactions are highly important in the mitochondrial respiratory chain, where the principal chromophores involved in laser therapy are thought to be situated. A third photochemistry pathway that can occur after the absorption of a red or NIR photon is the dissociation of a non-covalently bound ligand from a binding site on a metal containing cofactor in an enzyme.
~The most likely candidate for this pathway is the binding of nitric oxide to the iron-containing and copper-containing redox centers in unit IV of the mitochondrial respiratory chain, known as cytochrome c oxidase (see below).
~It should be mentioned that there is another mechanism that has been proposed to account for low level laser effects on tissue. This explanation relies on the phenomenon of laser speckle, which is peculiar to laser light. The speckle effect is a result of the interference of many waves, having different phases, which add together to give a resultant wave whose amplitude, and therefore intensity, varies randomly. Each point on illuminated tissue acts as a source of secondary spherical waves.
~The light at any point in the scattered light field is made up of waves that have been scattered from each point on the illuminated surface.If the surface is rough enough to creat e path-length differences exceeding one wavelength, giving rise to phase changes greater than 2Pi.jpg, the amplitude (and hence the intensity) of the resultant light varies randomly.
~It is proposed that the variation in intensity between speckle spots that are about 1 micron apart can give rise to small but steep temperature gradie nts within subcellular organelles such as mitochondria without causing photochemistry. These temperature gradients re proposed to cause some unspecified changes in mitochondrial metabolism

Biochemical Mechanisms :
~There are perhaps three main areas of medicine and veterinary practice where LLT has a major role to play These are
(i) wound healing, tissue repair and prevention of tissue death;
(ii) relief of inflammation in chronic diseases and injuries with its associated pain and edema;
(iii) relief of neurogenic pain and some neurological problems. The proposed pathways to explain the mechanisms of LLLT should ideally be applicable to all these conditions.
What is LLLT?
~Low Level Laser Therapy (LLLT) sometimes known as Low Level Light Therapy or Photobiomodulation (PBM) is a low intensity light therapy. The effect is photochemical not thermal. The light triggers biochemical changes within cells and can be compared to the process of photosynthesis in plants, where the photons are absorbed by cellular photoreceptors and triggers chemical changes.
~Low Level Laser therapy (LLLT) is the application of light to a biologic system to promote tissue regeneration, reduce inflammation and relieve pain. Unlike other medical laser procedures, LLLT does not have an ablative or thermal mechanism, but rather a photochemical effect which means the light is absorbed and cause a chemical change 6. The reason why the technique is termed low level is that the optimum levels of energy density delivered are low and it is not comparable to other forms of laser therapy as practiced for ablation, cutting, and thermal tissue coagulation 7.
~The first law of photobiology explains that for a low power visible light to have any effect on a living biological system, the photons must be absorbed by electronic absorption bands belonging to some molecular photo-acceptors, which are called chromophores 8. The effective tissue penetration of light at 650 nm to 1200 nm is maximized.
~The absorption and scattering of light in tissue are both much higher in the blue region of the spectrum than the red, because the main tissue chromophores (hemoglobin and melanin) have high absorption bands at shorter wavelengths and tissue scattering of light is higher at shorter wavelengths. Water strongly absorbs infrared light at wavelengths greater than 1100 nm. Therefore, the use of LLLT in animals and patients almost exclusively utilizes red and near-infrared light (600-1100 nm) 9.
~According to Posten et al, properties of low level lasers are:
a) Power output of lasers being 0.001- 0.1 Watts.
b) Wave length in the range of 300-10,600 nm.
c) Pulse rate from 0, meaning continuous to 5000 Hertz (cycles per second).
d) Intensity of 0.01-10 W/cm2 and dose of 0.01 to 100 J/ cm2 5.
The Usage of LLLT:-
~The temporomandibular disorders (TMDs) have been identified as the most important cause of pain in the facial region. Low Level laser therapy (LLLT) has demonstrated to have analgesic, anti-inflammatory and biostimulating effects. The LLLT is a noninvasive, quick and safe, non-pharmaceutical intervention that may be beneficial for patients with TMDs 37.
~Another study proposed a novel combination of neural regeneration techniques for the repair of damaged peripheral nerves. A biodegradable nerve conduit containing genipin-cross-linked gelatin was annexed using beta-tricalcium phosphate (TCP) ceramic particles (genipin-gelatin-TCP, GGT) to bridge the transection of a 15mm sciatic nerve in rats. Electrophysiological measurements (peak amplitude and area) illustrated by compound muscle action potential (CMAP) curves demonstrated that laser stimulation significantly improved nerve function and reduced muscular atrophy.
~Histomorphometric assessments revealed that laser stimulation accelerated nerve regeneration over a larger area of neural tissue, resulting in axons of greater diameter and myelin sheaths of greater thickness than that observed in rats treated with nerve conduits alone 38.
*The use of low level laser:-
~to reduce pain, inflammation and edema, to promote wound, deeper tissues and nerves healing, and to prevent tissue damage has been known for almost forty years since the invention of lasers.
~This review will cover some of the proposed cellular mechanisms responsible for the effect of visible light on mammalian cells, including cytochrome c oxidase (with absorption peaks in the Near Infrared (NIR)). Mitochondria are thought to be a likely site for the initial effects of light, leading to increased ATP production, modulation of reactive oxygen species, and induction of transcription factors. These effects in turn lead to increased cell proliferation and migration (particularly by fibroblasts).
Dangers of LASER:-
Eye damage if the beam is applied directly to the eye.
There is no thermal effect in the skin.
Pregnant uterus- avoid.