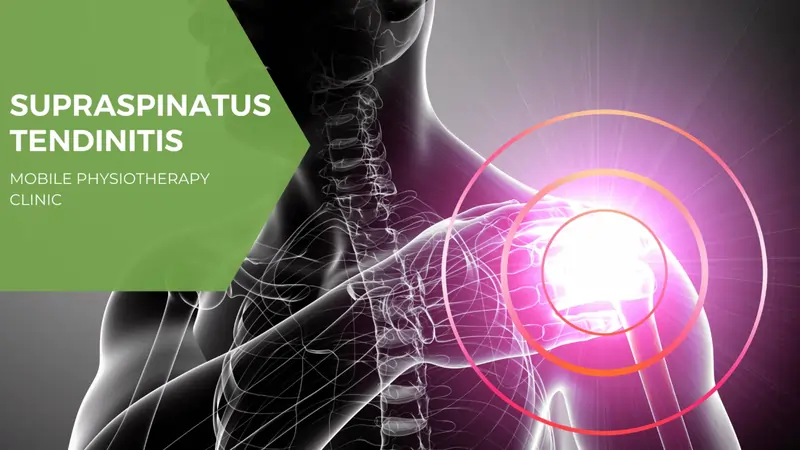
All You Need to Know About Supraspinatus Tendinitis
The supraspinatus tendon is a part of the rotator cuff muscles and is present in the subacromial space. The Supraspinatus is one of the four rotator cuff muscles. The condition of Supraspinatus tendinitis becomes more frequent after middle age. It is a very common cause of shoulder pain. Supraspinatus tendon overuse is considered one of the key factors of the condition.
Supraspinatus tendinitis is a result of degeneration of the Supraspinatus tendon in the rotator cuff. Degeneration can be caused due to repetitive stresses and overloading/overusing during sports or other activities. Diabetic patients are most likely to develop the condition.
The Supraspinatus tendon commonly affects the acromion as it passes between the acromion and the humeral head. Friction between the acromion and the tendon is reduced due to the subacromial bursa.
Table of Contents
What is Supraspinatus Tendinitis?
The supraspinatus muscle is located in the supraspinatus fossa, which is located at the lateral angle of the scapula. The supraspinatus muscle is further connected with the supraspinatus tendon which is a thick fibrous band of tissue, which in turn connects the supraspinatus muscles to the shoulder joint.
The function of the supraspinatus is to let the arm move upwards. When there is damage or injury to the supraspinatus tendon, it is referred to as supraspinatus tendinitis.
On average, Supraspinatus tendinitis develops in a person after their 50’s due to the normal process of aging. Due to aging, muscles start becoming weaker and then all of the tendons of the rotator cuff become weak.
The supraspinatus tendinitis is very common in diabetic patients, athletes who are involved in throwing and overhead motions. Badminton or tennis players are more likely to develop the condition as their sports require them to raise
the arms frequently and repetitively above shoulder level.
Symptoms of Supraspinatus Tendinitis
The most prominent symptom of Supraspinatus tendinitis is progressing pain. The pain may reach the lateral upper arm or may be felt in the top and front of your shoulder. Typically, it becomes worse with overhead activity. During the initial days of the condition, the pain is felt during activities only but after that may occur during rest.
If you are experiencing the following symptoms then you may have Supraspinatus Tendinitis:
- Tenderness over the affected arm.
- Swelling around the affected tendon.
- Shoulder’s limited mobility.
- Burning sensation in the shoulder.
- Ache in the shoulder that increases on elevation, overhead activity.
- Pain that is felt after reaching
- Difficulty in sleeping at night, mostly when lying on the affected shoulder.
- Feeling pain after any specific activity, that is done repeatedly.
- Difficulties with normal movements, such as brushing hair, putting on a shirt or jacket, or reaching the arm above shoulder height.
- Weakness while bending forward.
- Weakness during overhead activities
- Previous shoulder injuries
- Limited range of motions in the shoulder
- Previous shoulder trauma
- You cannot rotate your arm
- Posterior Tightness
- Decreased strength
- Pain when trying to reach behind the back
- Stiffness
- Triggered pain while lowering or raising your arm
- Inflammation
- The shoulder may be warm at all times
Patients with Supraspinatus tendinitis complain about decreased functional activity. You may hear a clicking sound because of the supraspinatus tendon slipping in and out of its normal position.
Its symptoms do not go past the elbow.
Causes of Supraspinatus Tendinitis
Overuse is the principal cause of Supraspinatus tendinitis. The condition can be developed by lifting something too heavy, falling on your arm, or dislocation of your shoulder.
Diabetic patients are prone to develop the condition. People from the age 50 to 59 are most likely to develop the condition.
Furthermore, Supraspinatus tendinitis can be caused due to primary and secondary impingement. Primary impingement is a result of increased subacromial loading whereas Secondary impingement is a result of rotator cuff overload and muscle imbalance.
There are some intrinsic and extrinsic factors involved in supraspinatus tendinitis which are:
Intrinsic Factors:
- Acromial morphology (hooked acromion, presence of an os acromiale or osteophyte, calcific deposits in the subacromial space, all of which predispose to primary impingement)
- Coracoacromial ligament hypertrophy
- Acromioclavicular arthrosis (inferior osteophytes)
- Coracoid impingement
- Subacromial bursal thickening and fibrosis
- Prominent humeral greater tuberosity
- Impaired cuff vascularity
- Aging
- Primary tendinopathy
- Intratendinous
- Articular side partial-thickness tears
- Calcific tendinopathy
Extrinsic Factors:
Primary impingement-
- Increased subacromial loading
- Trauma (direct macro trauma or repetitive microtrauma)
- Overhead activity (athletic and nonathletic)
Secondary impingement-
- Rotator cuff overload/soft tissue imbalance
- Eccentric muscle overload
- Glenohumeral laxity/instability
- The long head of the biceps tendon laxity/weakness
- Glenoid labral lesions
- Muscle imbalance
- Scapular dyskinesia
- Posterior capsular tightness
- Trapezius paralysis
Diagnosis
Imaging can be useful.
Shoulder X-rays can reveal calcifications in the rotator cuff and in the bursa. If you are experiencing the symptoms for a long time then there may be degenerative changes, such as cystic/sclerotic changes at the greater tuberosity and decreased humeral head-acromion distance, secondary to upward migration of the humeral head.
In the case of acute calcific tendinitis, calcifications may be irregular, fluffy, and ill-defined. Dynamic ultrasound can reveal thickening of the subacromial bursa and impingement during the abduction. Magnetic resonance imaging (MRI) is preferred over computed tomography (CT) since it produces more detailed soft-tissue images.
Supraspinatus Tendinitis Examination
There are different examinations that can reveal if you have Supraspinatus tendinitis or not.
It is seen that in the case of calcification, due to trauma, pain emerges after some time.
The physical examination consists of searching if there are any external wounds or bruises on the affected shoulder and taking the patient’s temperature to check if the person has a fever.
Further, your doctor will examine the area of the tendinous insertion of the supraspinatus muscle to check tenderness and pain.
Both passive and active tests will be performed.
Clinical examinations can exclude other causes of shoulder pain.
The shoulders are checked for symmetry, swelling, and muscle atrophy. Your doctor may check for tenderness below the acromion and over the greater tuberosity. Internal rotation of the shoulder can make it easier to examine supraspinatus insertion on the greater tuberosity.
The most important clinical tests are:
Painful arc test– This test can be conducted while sitting or standing. Your doctor will ask you to slowly lift your arm to the side. You have to stop when it hurts. In the case of Supraspinatus tendinitis, you will feel pain at 70 or 110 degrees.
Continue lifting your arm to the side, the pain might go away.
Usually, patients experience pain in the second part of the arc rather than the first part of the arc.
Neer’s Sign test- While putting, one hand on the scapula to stabilize it, your doctor will forward flex your arm. He will ask you to internally rotate your affected arm.
The test is considered positive if any pain is recognized by a patient.
Hawkins/ Kennedy test- Your doctor will forward flex your affected arm to 90 degrees, and then will bend the elbow. After that, he will try to forcibly internally rotate your arm.
The test is considered positive if the patient feels any pain.
Empty Can sign test– You will have to lift your arm to the side and stop at 90 degrees. Your doctor will then rotate your arm in a way that visualizes liquid pouring out of the can.
If you have Supraspinatus tendinitis, you will resist this motion.
Drop arm sign test– Your doctor will passively lift your affected arm to the side and then release his support, and then He will ask you to drop your arm slowly. If you cannot control the downwards movement, it can indicate supraspinatus tendinitis.
Treatment of Supraspinatus Tendinitis
The treatment for supraspinatus tendinitis depends upon the criticality of the condition. This treatment may involve physiotherapy, nonsteroidal anti-inflammatory drugs (NSAIDs), ice treatments, and resting. Corticoid injections can also be used with physical therapy.
Surgery can be a solution if there is no improvement after 3-6 months of conservative treatment.
NSAIDs: NSAIDs are the first choice in case of mild to moderate symptoms. A short-term use (7-14 days) of NSAIDs is very useful in relieving the pain associated with supraspinatus tendinitis. Also, there is little evidence that supports a long-term course of NSAIDs.
But for moderate to severe symptoms, subacromial corticosteroid injection may be required.
Electrotherapy modalities: These should be considered in order to avoid worse conditions. Modalities such as SWD, IFT, TENS, ultrasound, and cryotherapy can provide temporary relief in case of the acute phase.
Strengthening exercises: Exercises such as isometric exercises can be very beneficial. Strengthening exercises can work out the shoulder girdle musculatures. Proper home exercise programs can be taught too. Anyone can perform some light strengthening exercises for improvement.
Try to practice those strengthening exercises that work on the external rotators, internal rotators, biceps, deltoid, and scapular stabilizers.
If these muscles are Strengthened, they will keep the shoulder joint more stable and prevent further injuries.
There are three phases of progressive exercise treatment: Immobilization, passive/assisted range of motion, and progressive resistance exercises of the Supraspinatus Muscle. You should avoid repetitive movements that induce pain.
Massage Therapy: Once pain is reduced, massage therapy can be taken to restore the range of motion.
Wear a sling/tape: You can wear a sling or tape so that your shoulder remains unmoved.
Cryotherapy: It is the therapy of using extreme cold to freeze the abnormal tissues and remove them.
Active-assisted mobilisations: The mobilisations can be done by the patient himself/herself by using an exercise bar. You can also use a rope and pulley so that the unaffected arm is able to pull the affected one into anteversion.
Surgery: Surgery is considered the last option. Surgery is done only when there is a loss of function, failure to respond to conservative therapy for 3 months, or evidence of an acute tear in a younger patient.
Sometimes, the pain that was ignored before causes some serious consequences later. Such conditions can make your life miserable. So, it is advisable to take action during the initial days of the condition.