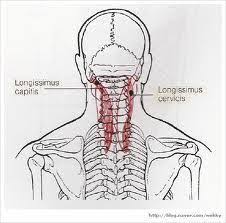
Longissimus capitis muscle:
Longissimus capitis muscle: the muscle lateral to the semispinalis muscles. It is the longest subdivision of the erector spinae muscles that extends forward into the transverse processes of the posterior cervical vertebrae. origin: The transverse processes are bony projections that stick out diagonally from the back of the vertebrae, while the articular processes are bony…