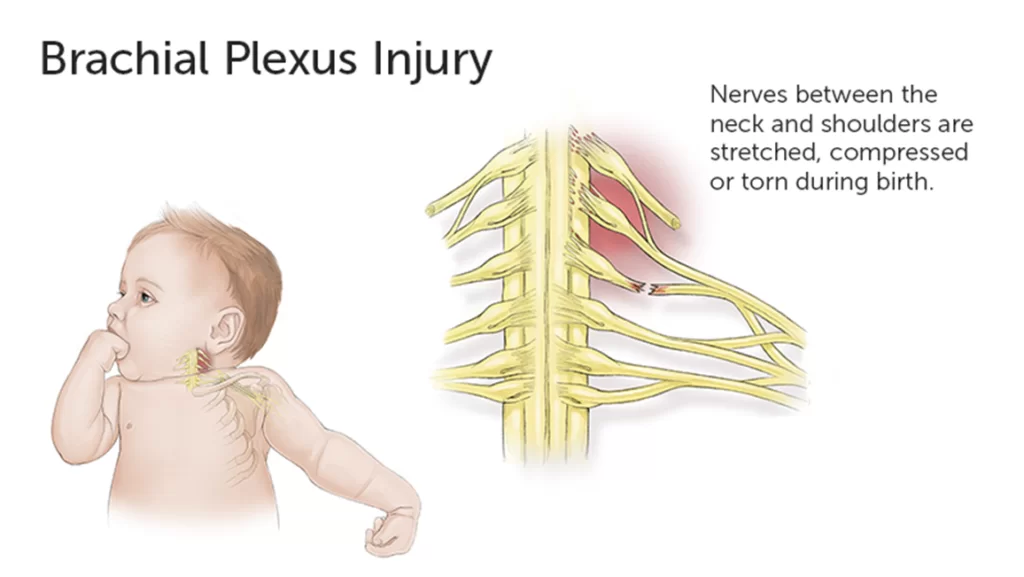
Brachial Plexus injury
Table of Contents
What is Brachial Plexus injury?
The brachial plexus initiate from the cervical vertebrae and passes to the neck to the axilla and supplies the upper limb. It is formed from the 5th to 8th cervical nerves of the ventral rami and the 1st thoracic nerve of the ventral ramus of the ascending part. Branches from the 2nd thoracic ventral ramus and 4th cervical may contribute.
Compression of the brachial plexus’s posterior, medial, and lateral cord can occur between the clavicle and first rib and below the pectoralis minor muscle.
A traumatic brachial plexus injury involves sudden injury to these nerves and may cause loss of sensation, muscle weakness, or loss of movement in the arm, hand, and shoulder. Injury to this nerve trunk often occurs when the arm is forcefully pulled or stretched. Mild brachial plexus injuries may not heal however more severe injuries require surgeries to regain function of the hand and arm.
Anatomy of Brachial Plexus:
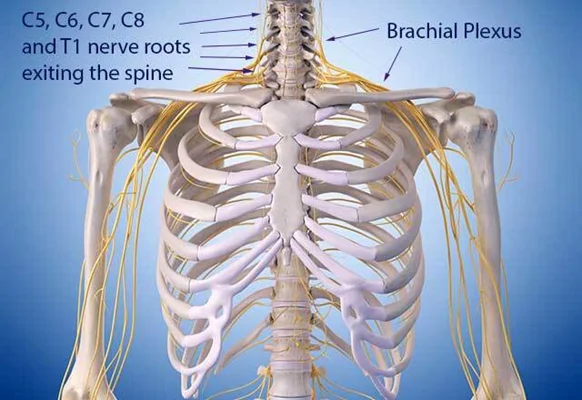
This nerve trunk is composed of the first thoracic nerve (T1) and four cervical nerve routes ( c5 to c8). These nerve roots combine with the three trunks. C8 to T1 to the lower trunk, C7 continues to the middle trunk, and C5 to C6 to the upper trunk.
What are the Causes of Brachial plexus injury?
The main causes of two-wheeler accidents. A common etiology is listed below.
Vehicular accident (majority two wheelers) accounts for >90% of cases
An industrial area is like —a weight falling from the height on the shoulder.
Heavy fall with stretching of the neck
Assault with a sharp object
Bullet injury—is rare in India
some injuries damage the posterior triangle of the neck.
The pathophysiology of the common cause is abnormal neck shoulder angle while the vehicle is falling down on the person. if the upper plexus is affected including C7, C6, and C5 roots with the shoulder in adducted position and the lower plexus is damaged because the shoulder is in abducted position i.e. C8-T1 roots. The high velocity of the vehicle damaged all nerve roots. It is resulting in a flail upper limb.
Types of brachial plexus injury:
Brachial plexus injuries depend upon the severity, amount of force placed on the plexus, and type of injury. Some patients can injure the brachial plexus in different nerve roots.
An avulsion: It is the most common and severe brachial plexus injury. The small chunk of the nerve root can be detached from the spinal cord. These types of injuries can not repair by surgeries. This term is called an avulsion.
Stretch [neuropraxia]: when the nerves are stretched to the point of injury. This term is known as neuropraxia. It is healing requires simple. The non-surgical method is useful to become a normal function.
Rupture: A nerve can be damaged partially or fully because more forcefully stretching occurs. Rupture is treated by surgery.
Upper-Trunk Palsy Injury:
Upper-trunk palsy occurs when the neck and angle between shoulders forcefully widen. such as when a fall forces the head should be opposite side and the shoulder should be down.
A patient has weakness in the arm and is unable to bend the arm at the elbow and also has unable to use the shoulder to raise the arm away from the body because the patient suffers from upper trunk palsies. In the shoulder, thumb, and outside of the arm may be loss of sensation.
An upper trunk palsy may weakness in the deltoid muscle and rotator cuff, and upper arm muscle.
Erb’s Paralysis:
Site of injury
The Erb’s point: The region of the upper trunk meets, Six nerves meet here. Erb’s palsy causes due to injury of the upper trunk.
Causes:
The head is away from the shoulder. some injuries have given below.
- Birth injury
- Fall on shoulder
- During anesthesia
Nerve roots involved:
- mainly C5
- mainly C5, partially C6
Muscles paralyzed:
Mainly: biceps, deltoid, brachialis, and brachioradialis.
Partillly: supraspinatus, infraspinatus, and supinator
Deformity:
Arm: Medially rotated, adducted, and hang by the side.
Forearm: Extended and pronated
Synonym : “Porter’s tip hand” – “Policeman’s tip hand”.
Disability:
Shoulder in abduction position and lateral rotation.
Flexion and supination of the forearm.
Biceps and supinator jerks are lost.
Sensory loss over the lower part of the deltoid.
Lower-Trunk Palsy Injury:
Lower-trunk palsy occurs when the angle between the chest wall and arm forcibly widens. This may injure the lower trunks and the lower nerves.
Patients with a lower-trunk palsy will typically maintain elbow and shoulder length, but also lose the function of the hand. After a long time, the fingers may develop a claw position band the patient will not be able to perform fine motor tasks. Patients also typically have hand numbness in at least the small finger and ring finger.
Klumpke’s Paralysis:
Site of injury:
klumpke’s paralysis causes due to lower trunk injury.
Causes:
May be caused due to the abduction of the arm, some time in birth injury, or clutching a tree branch with the hand during a fall from a height.
Nerve roots involved:
Mainly T1, Partially C8
Muscles paralyzed:
Intrinsic muscles of the hand (T1)
fingers and wrist flexors.
Deformity:
Claw hand (position of the hand) due to the unopposed action of the extensors and long flexors of fingers. In a claw hand, there is flexion at the IP joints and hyperextension of MCP joints.
Disability:
Claw hand
Cutaneous anesthesia and analgesia in a narrow zone along with the hand and ulnar border of the forearm.
Horner’s syndrome: miosis, ptosis, loss of ciliospinal and anhidrosis, enophthalmos reflex- may be associated. This is because of injury to the neck that leaves the spinal cord through nerve T1 and sympathetic fibers to the head.
Vasomotor changes: The arteriole dilatation occurs due to loss of skin areas. it is also a loss of sympathetic activity and drier due to the absence of sweating.
Injury to the lateral cord:
Cause:
The humerus is dislocated and associated with other joints.
Nerve involved:
The lateral root of median, musculocutaneous.
Muscles paralyzed:
Biceps
Coracobrachialis
The median nerve supplies all the muscles of the forearm, except the hand.
Deformity and disability:
Midprone forearm
Loss of flexion of the forearm
Loss of flexion of the wrist
radial side of forearm loss of sensation.
trophic changes and vasomotor changes.
Injury to the medial cord:
Cause:
dislocation of the humerus at the subcoracoid region.
Nerves involved:
Ulnar, Medial root of median
Muscles paralyzed:
ulnar nerve supplied all the muscles.
The median nerve supplied five muscles of the hand.
Deformity and disability:
Claw hand
loss of sensation on the ulnar side of the hand and forearm.
trophic changes and vasomotor changes as a bone.
Pan-Plexus Palsy Injury:
It occurs if the force of the injury is high. In pan-plexus palsy, all levels of the trunk and nerves are damaged. It results in complete paralysis of the hand and arm, which is known as the flailing limb.
Brachial plexus injury in newborns:
The region of the brachial plexus is a group of nerves around the shoulder. the nerves are damaged due to loss of movement and weakness of the arm. This is called neonatal brachial plexus palsy (NBPP).
Causes
The nerves of the brachial plexus can be affected by difficulty in delivery or compression inside the mother’s womb.
Injury may be caused by:
The baby’s neck and head pull toward the side as the shoulders pass through the birth canal.
During feet first delivery stretching of the infant’s shoulders.
During a breech delivery pressure on the baby’s raised arms.
There are various types of NBPP. This depends on the amount of paralysis of the arm.
Brachial plexus palsy mostly affects the upper arm. This is known as Duchenne-Erb or Erb-Duchenne paralysis.
Klumpke paralysis affects the lower arm and hand. This is less common.
The risk factor of NBPP:
- Breech delivery
- Maternal obesity
- larger-than-average newborn.
Shoulder dystocia: Difficulty delivering the baby’s shoulder after the head has already come out
NBPP is less common than in the past. Cesarean delivery is used because some major problems occur. A C-section is the risk of injury. Although C-sections also carry other risks.
NBPP may be considered with a condition known as pseudo paralysis. This is seen when the infant has a fracture and is no nerve damage, moving the arm because of pain.
What are the symptoms of a brachial plexus injury?
Symptoms depend on brachial plexus length and injury.
There are common symptoms of brachial plexus palsy:
- Sensory loss at the hand or arm
- pain in hand and arm
- unable to control the finger, wrist, and arm.
How is a Brachial plexus injury diagnosed?
Doctor Examination:
Patients with brachial plexus injuries must be examined and treated within an appropriate time, typically within 6 to 7 months after injury. The nerve input without longer muscle, the less likely it is that the muscle will function normally in the future.
The exact time for treatment depends on its location and type of injury.
Physical Examination:
If your doctor diagnosed a brachial plexus injury, they will also check if the other injury may cause it. They will take an assessment of all nerve groups controlled by the brachial plexus to identify the severity and specific location of the nerve injury.
The pattern of the nerves that arise from the brachial plexus control various muscles of the hand and arm and will assist your doctor in finding out sites of nerve injury. Your doctor will examine the brachial plexus which the nerve group supplied.
In addition, some patients show specific signs that help determine the location of the nerve injury:
Drooping of the eyelid, narrowing of the eye pupils and Horner’s syndrome is signs that the injury is nearer to the spinal cord.
A shooting-like pain in the nerve when the doctor checks along the affected nerves suggests an injury occurs in the spinal cord. The physical therapist will also assess your stability and range of motion of the shoulder and elbow.
Imaging Tests:
X-rays. this shows a clear picture of the injured part, like bone. X-rays of the arm, chest, neck, and shoulder are taken to check for associated fractures. Chest X-rays are used for injuries to the lungs and fractures of the ribs. If you are not taking a full, deep breath during the chest X-ray, the physical therapist may consider pulmonary function testing (PFT) with the guidance of a pulmonologist to find the damage to the nerves that control deep breathing.
Nerve conduction studies (NCV):
Nerve conduction studies measure the signals that go into the nerves of the hand and arm.
Computed tomographic (CT) scan: A CT scan is considered the most useable test for diagnosing spinal nerve injuries. . CT scan is typically performed at least 3 to 4 weeks after the injury to allow any potential blood clots around the nerve root to
dissolve. In some severe injuries, the patient needs MRI.
Electrodiagnostic studies(EMG): These tests measure muscle signals and nerve conduction. They are important to evaluate because they can confirm the diagnosis, characterize its severity, and assess the rate of nerve recovery, locate the nerve injury. An electrodiagnostic test is done after 3 to 4 weeks of injury. Electrodiagnostic studies are required after 2 to 3 months to check the repairing of the nerve injury.
Brachial Plexus Injury Treatment:
Brachial plexus injuries don’t always need treatment. Some people, adults with neuropraxia, or particularly babies with a brachial plexus birth injury recover without any treatment, though it can take as long as several weeks or months for the injury to heal.
Exercises can help heal and function and regain the range of motion. In severe injury, surgeries may require.
Nonsurgical Treatment for Brachial Plexus Injuries
Mild brachial plexus injuries require non-surgical treatment. The doctor suggests more following treatment.
Physiotherapists teach exercises that may help regain function in the arms and hands and improve range of motion and flexibility in stiff muscles and joints.
injections and corticosteroids to help manage pain during healing.
An orthosis is used in severe conditions like braces and an Aeroplan splint.
Medication: some medicine reduces the pain.
Occupational therapy: It works on practical skills like dressing and cooking in cases of severe muscle weakness, numbness and pain.
Surgical Treatment of Brachial Plexus Injuries
Brachial plexus injuries require surgeries, it is not healing own. Tissue of the nerve repair and heals slowly, so it can take few months to years to see the outcome of brachial plexus surgery.
Brachial plexus surgeries take 6 months to best recover. The following surgeries have given below.
Nerve repair: reconnecting a torn nerve.
Neurolysis: Improve the function of removing scar from the injured nerve to improve the function.
Nerve graft: It is a method used for connects the two nerves at their ends. It is important to heal the nerve.
Nerve transfer: The nerve grafting method is less important but sometimes it is healing the nerve and restores function.
Tendon and muscle transfers: To restore the function the tendon and muscle transfer method is required but it is less important.
Brachial Plexus Birth Injury Treatment:
In babies or infants, if no improvement is shown after three months of occupational therapy, consulting a pediatric neurosurgeon or neurologist can help determine if your child can require any other treatments or surgeries. Up to 10 out of 1 babies who have brachial plexus injury will require surgeries.
If the injury occurred during delivery or birth time, the best time for surgery is when your child is between 4 to 9 months, as you waiting so the babies or infants to go for surgeries.
Physiotherapy treatment
The main aim is to increase the range of motion, increase muscle strength, reduce pain, and denervate muscle.
The main aim is to increase the range of motion, increase muscle strength, reduce pain, and denervate muscle.
Pain control – acupuncture, TENS
Maintaining ROM – passive movements, exercise therapy, splinting, positioning
Strengthen weak muscles – biofeedback, exercise therapy
Managing chronic edema – compression garments, advice, massage therapy
Physiotherapy treatment in infants
Positioning and Handling:
The baby’s shoulder, elbow, and hand are in a supported and neutral position because the baby’s arm is very floppy. However, using a towel under the affected arm during sleep helps to keep the arm in a neutral position.
while skin care, dressing, and washing move baby’s arm.it helps in affected arms to undress last and dressed first. When washing and drying, particular care should be taken with the affected arm.
The therapist should be advised on which play is helpful in exercise. The exercise should depend on the baby’s development and the adaptations required.
These all the exercises help increase the range of motion and strength of the muscle.
They primarily ask the baby’s parents to assist the baby’s affected arm.
Support/Weight Bearing Exercises:
Place your baby on the floor on their front with their arms forward. In starting phase support the chest with help of put the rolled towel. Ask the baby to transfer the weight on the affected arm and then progress. this exercise by encouraging them to reach through the object with both hands.
Two Handed Exercises:
Place your hands on your child’s arms and encourage them to reach through the object with both arms. (assist the
affected arm as necessary). You can also do clapping to encourage the use of both hands. This exercise is done in a sitting position, the child is sitting alone, sitting on their back.
Sensation Exercises:
To increase the sensation and awareness of the baby’s arm, like, massage and stroke their arm and rub the skin with various textures. For soft sensation use velvet and fleecy materials and for rough sensation use bath towels etc. Involve the child in some activities. e.g. encourage the child to face both palms each other and clapping.
Physiotherapy treatments in adults
Aims of treatment:
- Increase/maintain range of movement
- Mobilize tight scar tissue
- Improve strength of affected muscles
- If the splint is required to take care of the joint in a good position
- Discuss/help with pain control
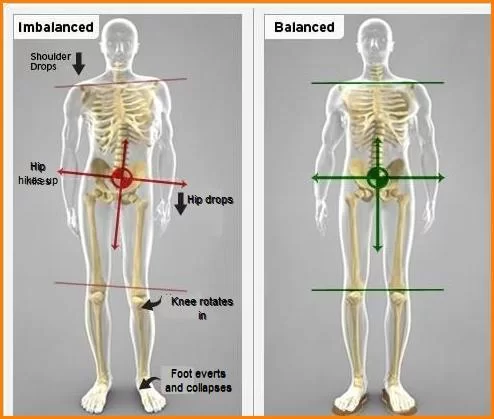
- Improve posture and balance
- Encourage return to work or sport.
Electrical Stimulation is used to maintain muscle property and also helps to strengthen muscles.
Physiotherapy Exercise Programme:
The following program of exercises is designed to help you be as independent as possible while doing the exercises.
The elbow and shoulder exercises usually start at 4 to 6 weeks, once the sling has been removed. The hand and wrist exercise is allowed while the sling is done. The duration of exercise is twice or three times per day with 10 repetitions.
Shoulder exercises
The patient is supine lying position, hold your affected arm by the wrist or hand and lift your arm above your head. This should be gradually improved when the patient is unable to take his arm above his head.
The patient required this type of exercise. The therapist assists the puts one hand across the top of the shoulder to stop moving. with the help of the other hands, they grasp around the elbow and fix the forearm between the body.
The therapist holds around your elbow to keep your arm close to your side. The therapist’s other hand holds around the wrist and in this position move your arm outside them.
After this exercise increases the repetition. Lift your affected arm up as far as you can and put the patient hand above his head. maintain this position, and stretch your elbow backward on the pillow side.
Elbow exercises
patient in a standing position, ask the patient to hold the affected hand with the help of the unaffected hand and stretch the elbow as far as possible.
Ask the patient the stretch the elbow as far as possible and get more stretching.
Wrist exercises
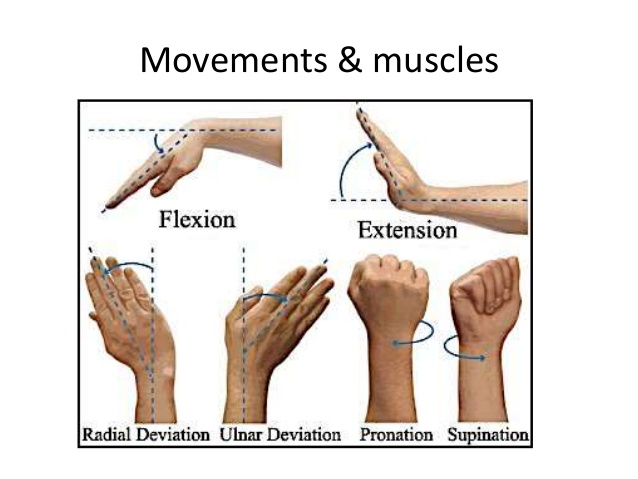
In a sitting position join both palms facing each other and push the wrist back of the affected hand with help of the unaffected hand.
Bend the wrist forward with the help of an unaffected hand.
Patient in sitting position, turn up the hand.
Hold your hand in the mid part of the palm and turn your palm down.
Hand exercises
Use your unaffected hand to help bend your fingers into your palm. Bend the fingers from the knuckles.
Patient in a sitting position, bend the fingers downward and upward. Also, stretch the fingers with the help of an unaffected hand( pad to pad or tip to tip ).
Thumb exercises
Ask the patient, to stretch the thumb. ( touch the fingers, like; opposition position)