Cauda Equina Syndrome(CES)
Table of Contents
What is Cauda equina syndrome (CES)?
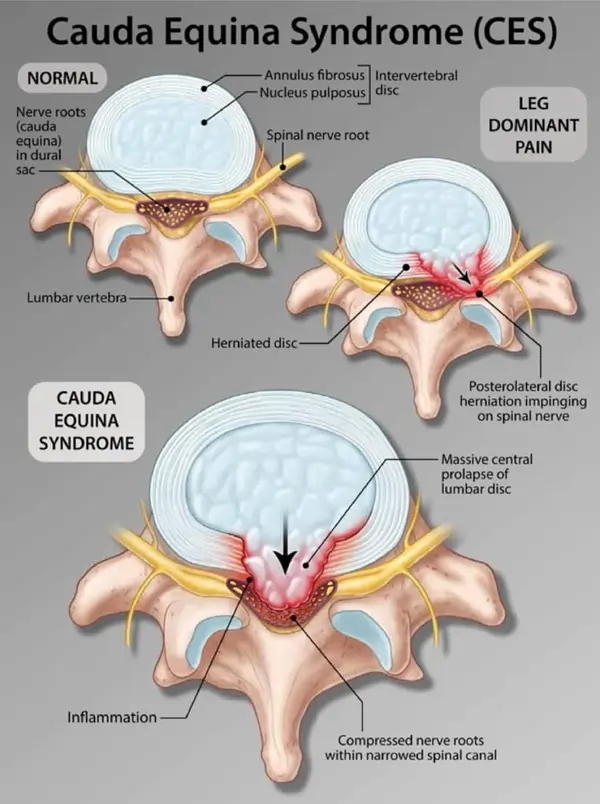
Cauda equina syndrome(CES) is an uncommon compression of the nerves at the end of the spinal cord within the spinal canal.
Cauda equina syndrome can be caused by any condition that results in direct irritation or pinching of the nerves which are located at the lower end of the spinal cord in lumbosacral spine.
These nerves provide motor and sensory function to the legs, feet, and pelvic organs.
It is a medical emergency and a rare yet serious condition. When these nerves are compressed, their function may be disrupted, with potentially serious repercussions. The symptoms of cauda equina syndrome might include lifelong paralysis of one or both leg muscles as well as bladder and bowel dysfunction (loss of bladder/bowel control).
The Latin term that means “horse’s tail” is the source of the cauda equina’s name. The nerve root sac like a horse’s tail in appearance.
Anatomy
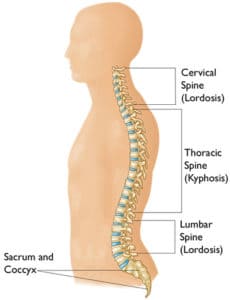
On average, the spinal cord tapers and stops between the first and second lumbar vertebrae. Its tapering end continues as the filum terminale, and the conus medullaris is the most distal bulbous portion of the spinal cord. The cauda equina (Latin for horse’s tail) is a group of nerve roots that are located distal to the end of the spinal cord. They like horsetails.
Causes of Cauda equina syndrome(CES)
Lumbar Herniated Disc:
Excessive pressure on the lower spine can cause a lumbar disc to herniate in a single injury, or it can happen when an existing weak disc is stressed and ruptures. The majority of lumbar disc herniations happen at the L4-L5 or L5-S1 vertebral levels.
Inflammatory conditions:
Inflammatory tissues or bony overgrowth pressing on lumbar nerve roots can cause cauda equina syndrome. For instance, ankylosing spondylitis is an inflammatory disease that could lead to cauda equina syndrome.
Lumbar spinal stenosis:
Cauda equina may develop if the spinal canal is compressed by lumbar stenosis.
Infections:
Infections of the spinal canal (osteomyelitis), such as a spinal epidural abscess, which in turn may potentially press into the spinal canal, producing neurological symptoms.
Tumors/neoplasms:
It may put pressure on the spinal canal. Tumors may originate in the spine, but it is more common for cancer from another part of the body to spread toward the spine (malignancy).
Trauma:
Injury to the lumbar spine, such as a car accident, fall, or a penetrative injury such as a gunshot or knife wound, can damage the cauda equina and produce neurological symptoms.
Postoperative complications:
Issues following lumbar surgery. After surgery to repair a lumbar herniated disc, just a few percent of patients develop cauda equina syndrome.
Iatrogenic:
Cauda equina syndrome can result from improperly positioned screws in the spine that compress and damage nerves.
Cauda equina syndrome has been associated with prolonged spinal anesthesia.
Patients undergoing anticoagulant therapy, which thins the blood, may develop spontaneous spinal epidural hematomas as a result of lumbar puncture (spinal tap). Cauda equina syndrome may result from this blood clot compressing the nerves.
Risk Factors
Those with a herniated disk, such as elderly people or sportsmen participating in high-impact sports, are at the highest risk of developing CES.
The following are additional risk factors for a ruptured disk:
- being obese or overweight:
- working at a job that involves a lot of sideways bending, twisting, pushing, and heavy lifting:
- possessing a herniated disk hereditary tendency.
Symptoms:
The degree of nerve compression affects how severe the symptoms of cauda equina syndrome are. The symptoms of cauda equina syndrome (CES) can appear gradually in some patients and suddenly in others.
LOWER BACK PAIN:
There are two types of low back pain: radicular and local.
Local pain is generally a deep, dull, steady, aching pain and may be felt across the lower back and/or pelvis, resulting from soft tissue and vertebral body irritation.
Compression of the nerve roots usually causes leg pain, also known as radiating pain, which is a sharp, stabbing ache. Radicular pain radiates along the dermatomal distribution, which is the precise location that the compressed nerve controls.
NEUROLOGICAL SYMPTOMS:
One or both sides of the body may have motor weakness, tingling, or numbness in the legs and/or feet. It may be challenging to stand or walk if you have numbness or weakness in your lower body.
Saddle anesthesia, or altered feeling in the “saddle region.” The part of the body that would come into touch with a saddle while seated on a horse is known as the saddle region. This area consists of the upper inner thighs, the buttocks and genitalia, and the groin. Cauda equina syndrome can cause neurological symptoms such as weakness, tingling, and/or numbness in all or sections of this area.
Leg or lower extremity pain that is sharp or stabbing.
Sciatic nerve pain, which can be felt on both sides of the body and manifests as a severe, burning sensation down the backs of the thighs and possibly into the lower legs and foot, might result from compression of the cauda equina.
BLADDER DISTURBANCES (URINARY MANIFESTATIONS):
- Inability to urinate (urinary retention).
- Difficulty initiating urination (urinary hesitancy)
- Decreased sensation when urinating (decreased urethral sensation)
- Inability to stop or control urination (incontinence)
BOWEL DISTURBANCES:
- Incontinence is the inability to stop or feel a bowel movement.
- Constipation
- Loss of anal tone and sensation
LOSS OF REFLEXES:
A person’s knee and ankle reflexes might be diminished, along with anal and bulbocavernosus abilities.
SEXUAL DYSFUNCTION:
The affected person may experience impotence or loss of ability to ejaculate or orgasm.
Diagnosis
A medical history, in which you respond to inquiries regarding your well-being, symptoms, and activities.
A physical examination to evaluate your motion, stability, alignment, strength, reflexes, and senses. Blood testing might also be required.
The following tests may help diagnose CES:
Magnetic resonance imaging (MRI):
A diagnostic test that uses computer technology and magnetic fields to create three-dimensional representations of body structures. Images of the spinal cord, nerve roots, and surrounding areas are generated using MRI.
Myleogram:
An X-ray of the spinal canal taken after a contrast substance has been injected into the surrounding cerebrospinal fluid spaces is called a myelogram. It may reveal spinal cord or spinal nerve displacement caused by malignancies, bone spurs, herniated discs, etc.
A computed tomography (CT) scan
Nerve conduction velocity (NCV) and electromyography (EMG) tests are two specialized neurologic nerve examinations of the lower limbs that might reveal the consequences of nerve irritation in the lower back.
PHYSICAL EXAMINATION:
Assessment of a patient suspected of having cauda equina syndrome aims at eliciting the following four cardinal features of the syndrome:
• Lower back pain with unilateral or bilateral sciatica
• Lower limb motor weakness
• Sensory abnormalities, particularly in the saddle area
• Visceral involvement, typically the urinary bladder.
(i) Lower back pain and sciatica:
STRAIGHT LEG RAISING TEST:
Lie the patient on their back, ensuring that the knees are fully extended and the leg is relaxed.
Explain that you plan to raise your leg gently and that you will stop when it causes pain.
Watching the patient’s face, cup your hand under the heel and raise the leg slowly,
stop at the onset of the pain, and notice the degree of elevation.
Lower the leg a few degrees and dorsiflex the foot fully with your free hand.
At this point, ask the patient if the pain comes back and to point to where it is felt.
Only reproduction of their radicular pain in correct dermatomes should count as a positive straight leg raising test, particularly if it occurs at <60 degrees of hip flexion.
(ii) Lower limb motor weakness:
Asking patients to walk on tiptoes and then to walk on their heels is a commonly used screening test for obvious L5 and S1 weakness respectively.
A more sensitive examination of the L5 myotome involves the demonstration that the patient can both evert the foot and extend the big toe (not simultaneously) against resistance.
S1 can be tested by asking the patient to invert the foot or to curl the toes. Although radicular neuropathy results in lower motor nerve signs such as muscle wasting, fasciculations, reduced tone, and diminished reflexes, these are late signs.
(iii) Sensory abnormalities, particularly in the saddle area:
After asking the patient to close their eyes, ask them to describe whether the stimulus felt blunt or sharp each time the appropriate dermatomes are touched at random with a blunt end or a pin prick.
(iv) Visceral involvement:
To assess the external anal sphincter’s strength, which is lacking in up to 80% of cases, ask the patient to “bite down” on your finger after it has been inserted. Take note of any fecal loading, as this may be a sign of more severe neuropathy.
Treatment
NON SURGICAL TREATMENT:
Depending on the underlying etiology of cauda equina syndrome, some people may benefit from medical therapy options. Corticosteroids like methylprednisolone (Solu-Medrol, Depo-Medrol) and anti-inflammatory drugs like ibuprofen (Advil, Motrin).
People who have infection-induced cauda equina syndrome should be treated with the right antibiotics. It is important to treat patients with spinal tumors (neoplasms) with radiation and chemotherapy.
SURGICAL TREATMENT:
LAMINECTOMY:
The lamina of the affected vertebra is removed during this treatment. By increasing the space surrounding the nerves, a laminectomy reduces pressure on them and therefore the term “decompression surgery.”
To preserve the strength of the spine, it could occasionally be necessary to use metal hardware and a bone graft (spinal fusion) to connect that vertebra to neighboring vertebrae.
DISCETOMY:
In patients with cauda equina syndrome caused by a herniated disk, a discectomy is performed to remove the disk material crushing the nerves, and a laminectomy is performed to remove a part of the bone surrounding the nerves.
PHYSIOTHERAPY TREATMENT:
THERMOTHERAPY:
Heat therapy for the lower back increases circulation, which eases stress and muscular spasms while increasing range of motion.
CRYOTHERAPY:
Ice packs may reduce minor pain and minimize inflammation.
Applying heat before exercise might help relax the muscles, while applying ice after exercise can help reduce pain.
LUMBAR TRACTION:
Spinal traction relieves pain from narrowed nerves by expanding the back. The therapist has two options: mechanically (using specialized machines) or manually (using his or her own body).
ELECTRICAL STIMULATION:
Your muscles are stimulated with a low-frequency electrical current to lessen inflammation.
Ultrasound:
Because ultrasound sends sound waves deep into your muscle tissues, it may help lessen discomfort, stiffness, and muscular spasms. This improves circulation by producing a mild heat.
EXERCISES:
PELVIC TILT:
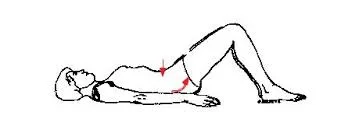
- Place your feet flat on the floor and lie on your back.
- Contract your abdominal muscles, press your belly button down toward the floor, and flatten your lower back as you release the breath.
- Hold for five seconds. Calm down.
- Hold for five seconds each time, repeating ten times.
LOWER TRUNK ROTATION:
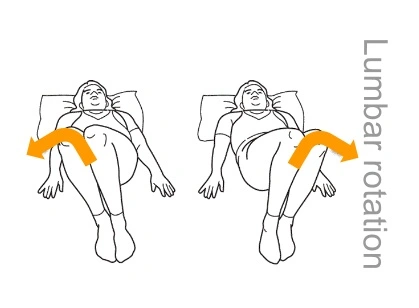
Lie on your back in the hook-lying position (knees bent and feet flat on the floor).
Rotate your knees to 1 side, holding them for 3 to 5 seconds.
While contracting your abdominal muscles, slowly rotate your knees to the other side and hold for 3 to 5 seconds.
Repeat up to 10 times on both sides.
BRIDGING:
- With your hands by your sides, knees bent, and feet flat on the floor beneath your knees, lie on your back.
- Make your buttocks and abdomen firmer.
- Raise your hips so that your knees and shoulders form a straight line.
- Pull your belly button back toward your spine by contracting your core.
- After 20 to 30 seconds of holding, go back to where you were before.
- Perform ten repetitions or more.
HAMSTRING STRETCH:
- Both legs should be level on the ground while you are flat on your back.
- Then, raise your right knee to your body and use your hands to support your right leg, or wrap a towel over your thigh and grip both ends firmly.
- Attempt to get your right leg perpendicular by lifting your right foot toward the ceiling. To bring your leg closer to your torso, you can pull on the towel gently.
- After 30 seconds of holding this position, switch to the other leg.
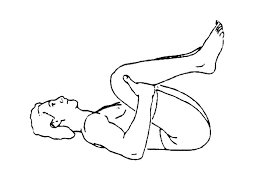
KNEE TO CHEST ( unilateral and bilateral ):

- Lie down on your back (Supine Position) with keep your feet flat.
- Using your hands to keep your leg in the stretched position, bring your right knee up to your chest. Hold for ten seconds.
- Repeat the exercise with your left knee after lowering your right leg. Hold for ten seconds.
- Do this three to five times for each leg.
- Stretch each leg separately, then hold both knees in the stretched position to complete the exercise.
- Hold for ten seconds.
- Then do it 3 or 5 times.
BILATERAL KNEE TO CHEST:
- Lie in prone position(face down)
Put your forearm at 90 angle with your arm and stretch your body up without lifting your elbow from the floor.
Hold this position for 10-15 seconds and then relax.
Repeat this 10 times.
PRONE SLR:
- On the floor, lie face down, or prone.
- Maintaining the engagement of your abdominal muscles, gently tighten your core muscles. While doing this, you should still be able to breathe.
- Slowly raise one leg backward while maintaining a straight knee and contracted abs. As your thigh rises off the ground, you should maintain a straight knee.
- After two seconds of holding your straight leg in the air, carefully bring it back to the floor.
- After ten to fifteen slow repetitions, go to the other leg and continue the exercise.
CAT AND CAMEL:
- Place your hands just under your shoulders and get on your hands and knees, keeping them hip-width apart.
- Your spine should be arched upward toward the sky as your abdominal muscles are tightened.
- Maintain the posture for ten seconds or more, then gradually ease your back.
- Bring your shoulders together, let your stomach drop to the floor, and then extend your back downward into a swayback position. Return to the starting position after ten seconds of holding.
- The sequence should be repeated at least three times.
Prognosis
Your nerve roots can be decompressed with surgery. It might avoid irreversible nerve damage if treated early. Unfortunately, once nerve damage occurs, it cannot be undone by surgeons. Following surgery, a medical professional will check in with you to discuss how the procedure went and to discuss the next stages in your treatment plan. In order to address any residual pain, incontinence, or muscle weakness, you will probably require long-term therapy regardless of your outcome.
Sexual dysfunction, lack of bladder or bowel control, and other cauda equina syndrome consequences are difficult to deal with. You might experience stress, sadness, or anxiety during this period. You can struggle at work, school, or in your friendships and interactions with loved ones. Your care team will collaborate closely with you to help you adjust and change your routine. In order to connect with people who have gone through similar things, you can even decide to see a mental health professional or join a support group.
Conclusion
Make an immediate appointment to visit the emergency department of the Hospital if you feel any of the symptoms of cauda equina syndrome. Even while it could be alarming, the sooner you receive treatment, the lower your risk of suffering irreversible injuries such as paralysis or incontinence.
After therapy, your body may take months or even years to heal. This indicates that you might have to physically empty your bowels and bladder. Your care team can help you modify your lifestyle to manage chronic symptoms, even if discussing urination and bowel movements with your provider may feel awkward.
With cauda equina syndrome, maintaining your mental health is equally as crucial as maintaining your physical health. During your recovery, you could find comfort in attending a support group or talking to a mental health professional.



![Downward Facing Dog Pose[Adho Mukha Svanasana]](https://mobilephysiotherapyclinic.net/wp-content/uploads/2023/12/Downward-Facing-Dog-PoseAdho-Mukha-Svanasana.webp)



9 Comments