Piriformis Syndrome
Table of Contents
What is piriformis syndrome?
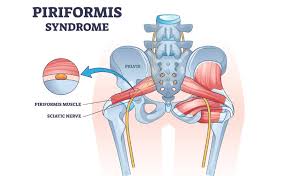
A neuromuscular disorder known as Piriformis Syndrome develops when the sciatic nerve is compressed by the piriformis muscle, which is situated deep within the buttock. Piriformis syndrome, sometimes confused with sciatica, is more frequent in those who sit for extended periods or do repeated lower-body motions. It is usually caused by muscular tension, overuse, or trauma.
Piriformis syndrome can be caused by a variety of reasons, but the clinical presentation is often constant. Furthermore, tingling symptoms throughout the sciatic nerve’s distribution and buttock numbness are prevalent.
Pathophysiology:
The piriformis muscle has a pyramidal structure and is flat and oblique. It begins in front of the sacrotuberous ligament, the superior border of the larger sciatic foramen, and the vertebrae (S2 to S4). After passing through the greater sciatic notch, the muscle attaches itself to the hip bone’s greater trochanter.
According to the ischial tuberosity’s anatomical placement, sciatic nerve entrapment happens either anterior to the piriformis muscle or posterior to the gemelli-obturator internus complex. Acute injuries that cause a quick and intense internal rotation of the hip or continuously bad posture can both put stress on the piriformis.
Causes of Piriformis Syndrome:
Overuse from sports like cycling, jogging, or extended sitting, especially on hard surfaces, is a common reason. Muscle damage or edema can also result from direct trauma to the buttocks, such as a fall or accident.
The risk of nerve compression may be elevated in certain people due to anatomical variances where the sciatic nerve runs through or around the piriformis muscle. This disorder may also occur as a result of poor posture, muscular imbalances, or inappropriate body mechanics when moving.
Symptoms of Piriformis Syndrome:
- The buttocks hurt deeply and painfully, generally on one side.
- Similar to sciatica, this pain travels down the back of the leg.
- Numbness or tingling in the leg or buttocks.
- Increased pain during extended periods of sitting or exercise.
- pain while getting up from a sitting posture or upward stairs.
- Hip range of motion reduction or lower back stiffness.
- Feelings of stiffness or tenderness in the buttocks.
Differential Diagnosis:
- Hamstring injury
- Lumbosacral disc injuries
- Lumbosacral discogenic pain syndrome
- Lumbosacral facet syndrome
- Lumbosacral radiculopathy
- Lumbosacral spine sprain
- Lumbosacral spondylolisthesis
- Lumbosacral spondylolysis
- Sacroiliac joint injury/dysfunction
- Inferior gluteal artery aneurysm or pseudoaneurysm
- Malignancy/tumors
- Arteriovenous malformations.
Diagnosis:
Piriformis syndrome can be difficult to diagnose since its symptoms frequently resemble sciatica or other lower back problems. A thorough medical history and physical examination, with an emphasis on symptoms, posture, and movement patterns, are usually the first steps taken by a healthcare professional.
To elicit symptoms and evaluate piriformis involvement, some tests, such as the FAIR test (Flexion, Adduction, and Internal Rotation), may be employed. While imaging tests like MRIs and CT scans can not directly prove piriformis syndrome, they are frequently used to rule out other illnesses like herniated discs. To find out if the piriformis muscle is the cause of the pain, diagnostic injections of anesthetic or anti-inflammatory drugs are occasionally used.
Treatment of Piriformis Syndrome:
Steroid injections around the piriformis muscle may help some people feel less pain and irritation. According to anecdotal evidence, botulinum toxin may be able to alleviate symptoms. Repeat injections are necessary, and the pain alleviation is only temporary.
Only individuals who have not responded to conservative treatment, such as physical activity, should be given this option. If there is any impingement, the operation may assist in decompressing the nerve; alternatively, the surgeon may remove scarring from the nerve or lyse any adhesions.
Exercise of Piriformis Syndrome:

The purpose of the piriformis stretch is to target and release stiffness and tension in the piriformis muscle, which is situated deep within the buttocks. If necessary, repeat on the opposite side after holding the posture for 20 to 30 seconds. This stretch can relieve piriformis syndrome-related leg and buttock pain by lowering pressure on the sciatic nerve.
Seated Spinal Twist:

Targeting the piriformis, spine, and surrounding muscles, the Seated Spinal Twist is a mild yet efficient stretch. Position your left elbow on the outside of your right knee and your right hand behind you for support. Looking over your shoulder, slowly rotate your torso to the right. This stretch lessens pain associated with the piriformis and increases spinal mobility.
Knee-to-Chest Stretch:

A straightforward yet powerful exercise for releasing gluteal and lower back stress, including piriformis muscle stiffness, is the Knee-to-Chest Stretch. Stretching involves lying on your back with your legs outstretched. Feel a little stretch in your buttocks and lower back as you hold the pose for 20 to 30 seconds. After that, switch sides and release. For a more thorough stretch, you can also bring both knees to your chest. This exercise relieves the piriformis syndrome-related lower body tension and pain.
Butterfly Stretch:

A sitting exercise called the Butterfly Stretch works the inner thighs, hips, and groin, which helps to relieve tension in the pelvic region and lessen the load on the piriformis muscle. Breathe deeply and maintain a straight spine. For 20 to 30 seconds, hold the posture. This stretch helps relieve piriformis-related pain and increases hip flexibility.
Hip Flexor Stretch:

By lengthening the muscles at the front of the hip, the Hip Flexor Stretch helps ease piriformis strain and pelvic instability. Keep your lower back from arching. Lean slightly to the left and raise your right arm above for more intensity. This stretch relieves the symptoms of piriformis syndrome by promoting the appropriate position and increasing hip mobility.
Walking (gentle, short distances):

For those with piriformis syndrome, walking is a low-impact aerobic exercise that can help increase blood flow, lessen muscular rigidity, and accelerate the healing process. Frequent, mild walking keeps the gluteal and hip muscles engaged without overtaxing the piriformis.
Additionally, it can relieve strain on the sciatic nerve and promote general movement. Wear supportive shoes and begin with short distances on level terrain. Increase the amount of time gradually as tolerated, with a daily goal of 15 to 30 minutes of walking. Walking regularly, along with strengthening and stretching activities, will greatly help manage piriformis pain.

Flatten your lower back against the floor to activate your core. Maintaining the opposite arm and leg in place, slowly drop your right arm and left leg toward the floor. Do 8–12 repetitions on each side. People with piriformis syndrome benefit from this regulated movement because it improves core stability, which supports good posture and alignment.
Bird Dog:
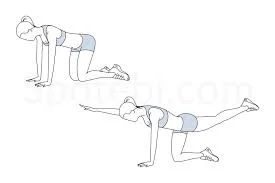
Maintaining your hips and shoulders level, slowly stretch your right arm forward and your left leg straight back while activating your core. After a few seconds of holding, flip sides and go back to the beginning position. Do ten to twelve reps on each side. Bird Dog may lessen piriformis syndrome symptoms by enhancing posture, spinal alignment, and coordination.
Wall Sit:

The Wall Sit is an isometric exercise that helps to stabilize the pelvis and ease strain on the piriformis muscle by strengthening the glutes, quadriceps, and hamstrings. Standing with your back flat against a wall and your feet shoulder-width apart, approximately two feet from the wall, is how you do a wall sit. As your strength increases, progressively extend the time you hold the posture for 20 to 30 seconds while keeping your back on the wall. This exercise helps relieve piriformis by improving hip alignment and increasing lower body stamina.
Prognosis:
Piriformis syndrome has a relatively good prognosis, particularly when diagnosed early and treated appropriately. Conservative therapies, including stretching, strengthening exercises, physical therapy, posture correction, and activity adjustment, result in considerable improvement for the majority of people.
Depending on how severe the symptoms are and how long they last, recovery might take a few weeks to several months. Although they are seldom necessary, more sophisticated treatments like injections or surgery may be needed in severe or persistent situations. Long-term results are usually favorable, and recurrence may frequently be prevented with regular care and preventative measures.
Complications of Piriformis Syndrome:
Piriformis syndrome can result in several consequences if it is not treated or is not adequately controlled. Chronic sciatic nerve compression is one of the most prevalent, and it can result in tingling, numbness, or chronic pain that travels down the leg.
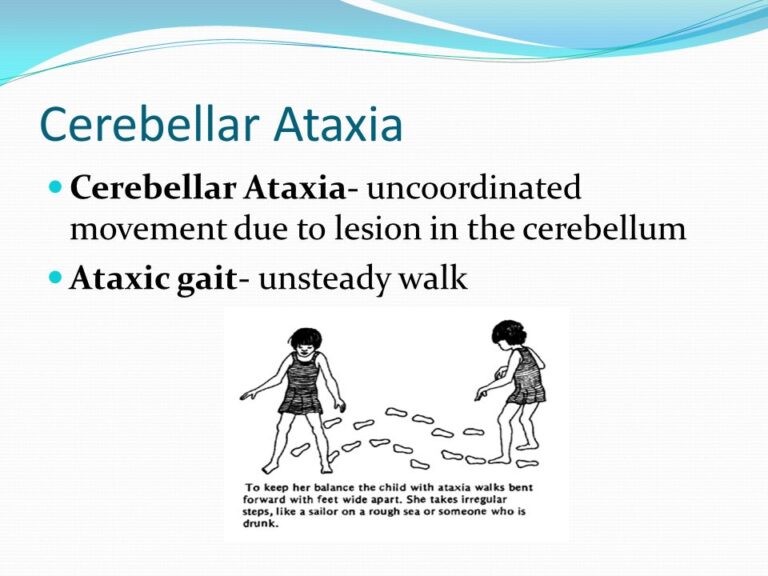
This may eventually cause the affected limb to become less mobile, have weaker muscles, and perform worse. The ongoing pain may also lead to aberrant gait and postural imbalances, which raises the risk of straining other body parts like the knees or lower back. Persistent pain can also cause mental health problems, including worry or depression, sleep problems, and decreased physical activity. To avoid these issues, early diagnosis and appropriate treatment are crucial.
Prevention of Piriformis Syndrome:
Piriformis syndrome may be avoided by preserving strength, flexibility, and good body mechanics. Frequent hip, gluteal, and hamstring stretches help maintain the piriformis muscle’s suppleness and lower the chance of stiffness.
In addition to supporting good posture, strengthening the hip stabilizers and core muscles eases the load on the pelvis and lower back. Using ergonomic seats or lumbar support, avoiding extended sitting, and maintaining proper posture both while standing and when sitting can all be beneficial.
Make sure you warm up and cool down properly before working out, and refrain from abruptly increasing the intensity of your workout. Additionally, the chance of getting piriformis syndrome can be considerably decreased by wearing supportive footwear and exercising with proper form.
Conclusion:
Even though it may resemble sciatica, it is frequently treatable with early detection and conservative measures such as activity moderation, posture correction, strengthening exercises, and focused stretching. Most people can recover completely and prevent recurrence with regular care and attention to preventative measures.
FAQs
The vitamin is abundant in nuts, seeds, plant oils like flaxseed oil, and fatty seafood like salmon and sardines. These foods are a vital component of your diet because they can help lessen the pain and inflammation linked to piriformis syndrome.
Physical therapy, exercise, and stretching are the cornerstones of treatment for piriformis syndrome, even if prescription treatments such as muscle relaxants, pain relievers, and anti-inflammatory drugs may be suggested. Gait modifications are one type of specific therapy. increased sacroiliac joint motion.
The majority of patients report sciatica-like pain down the back of the thigh, calf, and foot, along with severe buttock soreness. The following are typical signs of piriformis syndrome: The buttocks hurt dullly.
Avoid sitting as much as possible. Because of the structure of the hips, lower back, and other areas where the piriformis muscle is found, sitting can easily exacerbate piriformis syndrome. Therefore, it would be clear to avoid sitting at all or, at the very least, to only sit when necessary.
For example, piriformis sufferers have increased hip mobility and prolonged sitting pain. When lying down, sciatica patients often experience pain when they elevate their affected leg.
Using a mix of manual treatment, stretching, strengthening exercises, and posture correction, piriformis syndrome physiotherapy usually aims to reduce pain, increase flexibility, and restore functional mobility. The objective is to reduce muscular imbalances and sciatic nerve pain caused by the piriformis muscle’s compression or stimulation of the nerve.
Try applying pressure to each buttock muscle. In the center of the cheek, apply a little pressure. Another option is to attempt what is known as the “straight leg test.” Ask a friend or family member to assist you with this exam.
Try doing some stretching exercises.
Clasp your hands behind your thigh and cross your foot over the opposing knee. Hold your thigh for 30 seconds after pulling it toward you until you feel the strain. On the other side, repeat.
Walking can assist in increasing back mobility, releasing endorphins, and supporting your body’s natural healing processes, making it a crucial component of the recovery process for sciatic pain and piriformis syndrome pain.
Place the affected leg’s ankle close to your knee on the thigh on the other side. Gradually lift your knee out from your body with your hand until your hips start to extend. For 15 to 30 seconds, hold the stretch.
Entrapment of the sciatic nerve at the level of the ischial tuberosity results in piriformis syndrome. Piriformis syndrome can be caused by a variety of reasons, but the clinical manifestation is often the same.
References:
- Piriformis syndrome. (2025, June 2). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/23495-piriformis-syndrome
- Hicks, B. L., Lam, J. C., & Varacallo, M. A. (2023, August 4). Piriformis syndrome. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK448172/
- Patel, A., MD. (2023, February 22). What is Piriformis syndrome? Spine-health. https://www.spine-health.com/conditions/sciatica/what-piriformis-syndrome
- Piriformis syndrome: What is it? (2024, February 25). WebMD. https://www.webmd.com/pain-management/piriformis-syndrome-causes-symptoms-treatments
- Wikipedia contributors. (2025aj, June 12). Piriformis syndrome – Wikipedia. https://en.wikipedia.org/wiki/Piriformis_syndrome
- Piriformis syndrome: MedlinePlus Medical Encyclopedia. (n.d.). https://medlineplus.gov/ency/patientinstructions/000776.htm
- Healthdirect Australia. (n.d.). Piriformis syndrome. https://www.healthdirect.gov.au/piriformis-syndrome






3 Comments