Herniated Disc (Slipped Disc)
Table of Contents
What is a Herniated Disc?
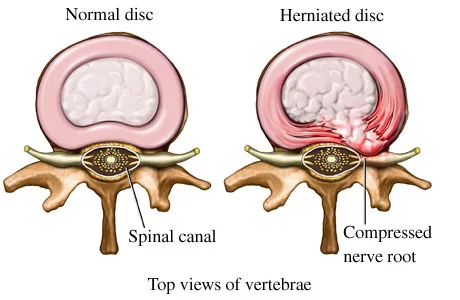
A herniated disc occurs when the soft, gel-like center of a spinal disc pushes through a crack in its outer layer. This can irritate nearby nerves, causing pain, numbness, or weakness, often in the lower back or neck.
- It is among the most prevalent conditions that cause individuals to experience leg and/or low back pain.
- A herniated disc happens when the disc’s jelly-like core squeezes out when the fibrous outer layer bursts or tears.
- A herniated disc occurs when the annulus fibrosis or nucleus pulposus moves outside of the intervertebral disc space. Failure in the innermost annulus rings initiates this herniation process, which then spreads outward radially.
Fully extending the spine repeatedly or for an extended length of time seems to be linked to disc annulus injury. During disc compression, the annulus swells outward and the nucleus loses its hydrostatic pressure.
ANATOMY OF IV DISC AND VERTEBRAE
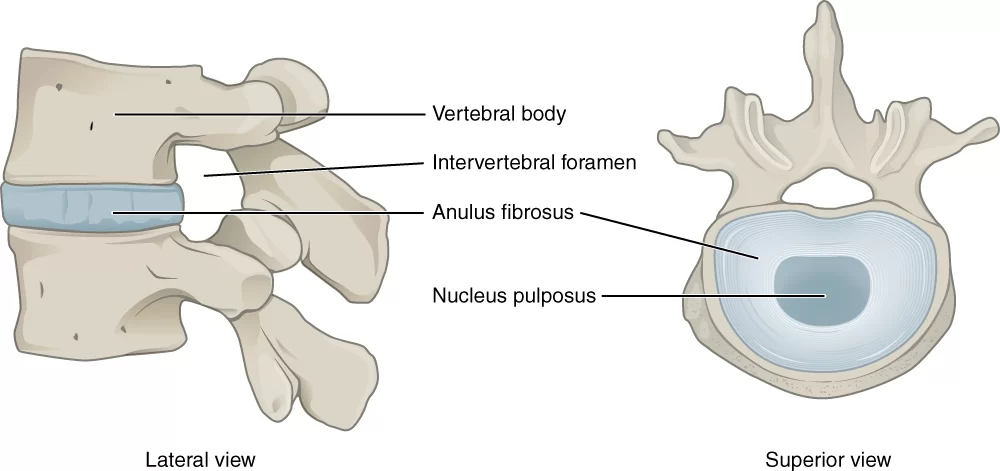
Support and protection are provided by your vertebral column, often known as your backbone. There are 33 vertebrae (bones) in it.
Between each vertebra are discs that serve as shock absorbers or pads. The annulus fibrosus, which resembles a tire, and the nucleus pulposus, which resembles gel, make up each disc.
The spinal cord and spinal nerves are protected in the spinal canal, a protective tube made possible by the vertebrae and discs working together. These nerves escape to different places of the body after running down the middle of the vertebrae.
There are also blood vessels, ligaments, tendons, and muscles in your back. Muscles are tissue fibers that provide the force needed to move. Tendons connect muscles to bones and discs, and ligaments are the strong, elastic bands of fibrous tissue that hold the bones together. Blood vessels supply nutrition. Together, these components enable you to navigate.
The lumbar area, or low back, is where a herniated disc most frequently happens. This is due to the fact that the majority of the body weight is supported by the lumbar spine. A nerve may occasionally be compressed by the herniation, resulting in discomfort that radiates or extends to other areas of the body.
The quantity of pieces that penetrate the annulus fibrosus and whether it compresses a nerve are two factors that frequently affect how painful a disc rupture is.
FUNCTION OF INTERVERTEBRAL DISC:
There are three main purposes for the discs in the spine:
- They are positioned between each bony vertebra in the spine and serve as a shock absorber.
- They serve as strong ligaments that keep the spine’s vertebrae joined.
- The spine can move somewhat thanks to these cartilaginous joints.
STAGES OF DISC HERNIATION:
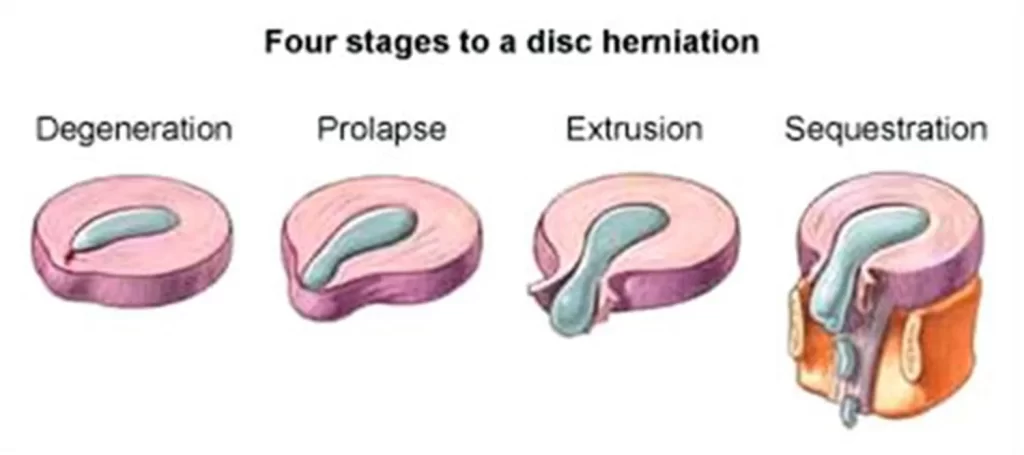
Clinical Anatomy and Management of Back Pain describes four different kinds of herniated discs. These include:
- Degeneration
Expansion of the disc margin past the neighboring vertebral end-plate borders
- Prolapse or protrusion
The nucleus pulposus presses against the annulus fibrosus, but the posterior longitudinal ligament is unaffected.
- Extrusion
The posterior longitudinal ligament is unaffected even if the nuclear material passes through the annular fibers.
4. Sequestration
The posterior longitudinal ligament gets injured as the nuclear material passes through the annular fibers. The nucleus pulposus has extended out into the epidural space in part.
What are the Causes of a Herniated Disc?
Although they can happen at any age, males between the ages of 20 and 50 are more likely to have herniated disks.
Among the factors that increase the probability are:
WEIGHT:
The lower back is further strained by being overweight.
GENETICS:
A herniated disk may be inherited.
OCCUPATION:
Herniated disks are more common in those who work in physically demanding occupations or engage in activities that require pushing, pulling, or twisting. They can be caused by any repetitive activity that puts tension on the spine.
INCORRECT LIFTING METHODS:
When lifting big objects, one should always exert force from the legs rather than the back. A herniated disk may result from improper technique.
Frequently driving:
Long periods of sitting combined with the car’s movements and vibrations might harm the disks and spinal structure.
SEDENTARY LIFESTYLE:
A herniated disk can result from inactivity.
SMOKING
This could cause the tissue to break down and cut off the oxygen supply to the disks.
Which Symptoms are seen in the Herniated Disc?
Although they can also happen in the cervical spine, the majority of herniated disks occur in the lumbar spine, which is the lower back. The following are the most typical indications of a herniated disk:
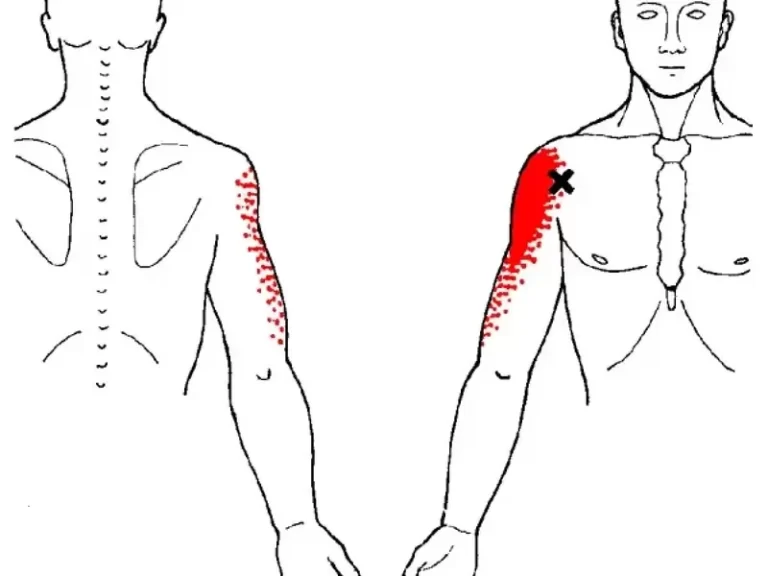
LEG OR ARM PAIN:
Your buttocks, thighs, and calves will usually be the areas that hurt the most if your ruptured disk is in your lower back. A portion of the foot may also be affected. The shoulder and arm usually experience the most severe pain if your ruptured disk is in your neck. When you cough, sneeze, or move your spine in specific ways, the pain may radiate into your arm or leg.
NUMBNESS OR TINGLING:
Numbness or tingling in the body part that the damaged nerves serve is a common symptom of a herniated disk.
Weakness
Nerves that are impaired often cause their muscles to weaken. This could make it harder for you to lift or hold something, or it could make you stumble.
General symptoms of lumbar herniated disc pain include the following:
LEG PAIN:
Usually, the leg pain is more severe than the low back pain. Sciatica or radiculopathy is the term used to describe pain that travels along the big sciatic nerve’s route at the back of the leg.
NERVE PAIN:
The leg’s nerve pain, which can be described as burning, intense, electric, radiating, or piercing, is typically the most obvious sign.
SYMPTOMS’ VARIABLE LOCATION:
Symptoms usually affect only one side of the body and might occur in the lower back, buttocks, front or back of the thigh, calf, foot, and/or toes, depending on factors such as the degree of herniation and the location of the disc’s herniation.
MENTAL SYMPTOMS:
Leg, foot, and/or toe numbness, a pins-and-needles sensation, weakness, and/or tingling may be felt.
Foot Drop:
One of the neurological symptoms caused by the herniation is foot drop, which is the inability to raise the foot when walking or standing on the ball of the foot.
LOW BACK PAIN:
There may be lower back pain, but it’s not always there. Low back pain can be characterized as throbbing or dull, and it may be accompanied by stiffness. Lower back muscle spasms caused by a herniated disc may be slightly relieved by resting flat on the back with a pillow under the knees, sitting in a supported chair, taking ice or heat, or taking a day or two of relative rest.
Pain that gets worse when you move:
Prolonged sitting or standing, as well as even a short walk, might cause pain. The pain may also be worsened by a sneeze, laugh, or other sudden movement.
HUNCHING FORWARD CAUSED PAIN TO GROW:
Many people discover that their leg pain significantly worsens when they slouch or hunch forward on a chair or bend forward at the waist.
IMMEDIATE ONSET:
Even though there might not have been a specific action or incident that caused the pain, lumbar herniated disc pain typically develops swiftly.
If the herniation is significant, the symptoms of a lumbar herniated disc are typically more severe. If no nerve is impacted by the disc herniation, the pain may be less severe and restricted to the lower back.
Sometimes the first sign of a herniated disc is low back or leg pain that lasts a few days before going away.
How to Diagnose the Herniated Disc?
PHYSICAL EXAMINATION:
These tests may include:
- Muscle strength tests:
In order to look for indications of a pinched nerve, your doctor will test the strength of particular muscles in your legs or feet. - Sensory testing:
This test measures your sensitivity to hot and cold, light touch, and pinpricks. - Deep tendon reflexes (knee and ankle jerk):
A reflex hammer will be used by your physician to tap your knees and ankles. You may have little to no reaction in your ankle (Achilles tendon) or knee (patellar tendon) if your lower back nerve roots are compressed. - Lying straight-leg test:
You will stretch both legs out while lying on your back. The affected leg will be raised toward your head by your physician. When the leg is raised up, pain travels down the back of the leg, below the knee, indicating a positive test result for a herniated disc. - Sitting straight-leg test:
You will sit on the exam table with both knees bent at a 90-degree angle, hanging over the side. One leg will be gradually extended by your physician until the knee is straight. The test is conducted on your other leg after your limb has been released. When the leg is elevated, pain travels down the back of the leg, below the knee, indicating a positive test result for herniated discs. - Femoral stretch test:
On the test table, you will lie with your legs outstretched, face down. Your physician will bend your knee after raising one leg toward the ceiling. One of the nerve roots high in the lumbar area (lower back) is probably inflamed if this test results in discomfort that radiates toward the front of the leg. - Valsalva maneuver:
As with a bowel movement, you will cough or press down. A Valsalva maneuver could worsen pain or other disc-related symptoms if you have a herniated disc.
IMAGING TEST:
X-rays:
Although they cannot identify herniated disks, plain X-rays can be used to rule out other possible causes of back pain, such as a tumor, infection, problems with spinal alignment, or a broken bone.
Computerized tomography (CT scan):
A CT scanner creates cross-sectional images of your spinal column and surrounding structures by combining a number of X-rays taken from various angles.

Magnetic resonance imaging (MRI):
The inside structures of your body are imaged using radio waves and a powerful magnetic field. This test can be performed to determine which nerves are impacted and to validate the location of the herniated disk.
Myelogram:
After injecting an indicator into the spinal fluid, X-rays are obtained. Multiple herniated disks or other problems may cause pressure on your spinal cord or nerves, as indicated by this test.
PREVENTION MEASURES:
Although a herniated disc cannot always be avoided, there are precautions you may take to lower your risk:
- Make sure to use safe lifting methods. Keep your waist straight. Use your powerful leg muscles to assist you in maintaining the weight while bending your knees and maintaining a straight back.
- Keep your weight in check. Carrying too much weight strains the lower back.
When standing, sitting, walking, and sleeping, maintain proper posture. Put your shoulders back, your abdomen in, and the small of your back flat, for instance, and stand up straight. Your feet should be flat on the floor or raised when you sit. Sleep on your side rather than your stomach, and choose a firm mattress. - When sitting for extended periods of time, stretch frequently.
- Avoid wearing shoes with high heels.
- Maintain strong back, leg, and stomach muscles by engaging in regular physical activity. Do aerobic exercises on a regular basis. In a regular exercise regimen, try to strike a balance between strength and flexibility.
- Stop smoking.
- Consume balanced, healthful meals.
Treatment of Herniated Disc
MEDICAL TREATMENT:
Over-the-counter (OTC) medications: For mild to moderate pain, ibuprofen or naproxen-based medications may be helpful.
Nerve pain medications:
Gabapentin, pregabalin, duloxetine, and amitriptyline are among the medications used for relieving nerve pain.
Narcotics:
A doctor may prescribe codeine, oxycodone, and acetaminophen, or another narcotic, if over-the-counter drugs are ineffective at relieving pain. Constipation, sedation, nausea, and confusion are some of the adverse effects.
Cortisone injections:
To help lessen pain and inflammation, these can be injected straight into the herniation site.
Epidural injections:
Steroids, anesthetics, and anti-inflammatory drugs are injected by a physician into the epidural space, which surrounds the spinal cord. This may lessen pain and edema in the area of the spinal nerve roots.
Muscle relaxants:
Muscle spasms are lessened as a result. Sedation and dizziness are common adverse effects.
Surgical Treatment
Spinal surgery may be recommended for a patient if:
-Developing progressive neurological impairments, including leg weakness and/or numbness
- Loss of bowel and bladder functions
- Back and leg pain limit normal activity
- Standing and walking difficulties
- Medication and physiotherapy are ineffective
- Generally good state of health
Surgical Treatment
ARTIFICIAL DISC SURGERY
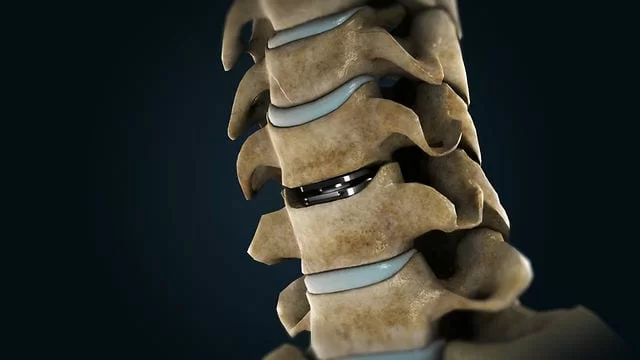
Surgically replacing a manufactured disc for a damaged or herniated lumbar disc.
DISCECTOMY:
An intervertebral disc may be removed surgically or partially.
LAMINECTOMY
Surgically removing the majority of a vertebra’s bone arch, or lamina.
LAMINOTOMY
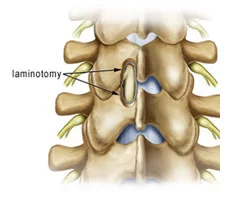
To release pressure on the nerve roots, a lamina is opened.
SPINAL FUSION
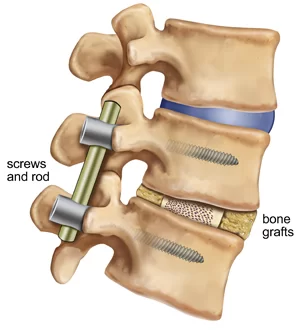
A process that creates a firm union between two or more vertebrae by grafting bone onto the spine; extra spinal support may be provided by the use of rods and screws.
- MASSAGE
There are over 100 different kinds of massage, but if you have a herniated disc, deep tissue massage is the best choice since it applies a lot of pressure to release deep muscular tension and spasms that form to limit muscle movement at the problem area.
2. HOT AND COLD THERAPY
To achieve the best outcomes, your physical therapist may switch between heat and cold therapies, each of which has advantages of its own.
To improve blood flow to the targeted area, your physical therapist could apply heat. Blood provides additional oxygen and nutrients, which aid in the healing process. Additionally, waste products from muscle spasms are removed by the blood.
Cryotherapy, another name for cold therapy, decreases circulation. This lessens pain, muscular spasms, and inflammation. To calm irritated tissues, your physical therapist may apply an ice pack, massage you with ice, or even use a spray called fluoromethane.
3. TRACTION
Reducing the effects of gravity on the spine is the aim of traction. The goal is to lessen the disc herniation by carefully separating the bones. The analogy is similar to how a flat tire “disappears” when the pressure is removed from it and a jack is placed underneath the vehicle. Both the cervical and lumbar spines can be used for it.
4. ULTRASOUND
In order to transfer heat deep into the tissues, ultrasound is utilized. Ultrasound is intended to improve mobility by boosting local blood circulation and metabolism, enhancing connective tissue flexibility, and speeding up tissue regeneration—all of which may lessen stiffness and pain.
5. TENS [TRANSCUTANEOUS ELECTRICAL NERVE STIMULATION]
An electrical current is used by a TENS unit to activate your muscles. Although it sounds intense, it isn’t actually painful. Key sites on the nervous system receive a little electrical current from electrodes that are attached to your skin. TENS lessens muscle spasms and is thought to cause endorphins, your body’s natural analgesics, to be released.
6. HYDROTHERAPY
Water is used in hydrotherapy. Hydrotherapy can be as simple as sitting in a warm shower or whirlpool bath as a passive treatment. Hydrotherapy relaxes muscles and relieves pain gradually.
7. EXERCISES
HANGING:

- Let your body “just hang” from a bar, the top of a door, or whatever else you can hang from.
- Do three sets while hanging for 30 seconds.
- Try some of the other exercises if this strategy makes you feel worse.
BACK EXTENSION IN STANDING:

- Start this workout by standing up straight and maintaining proper posture. Place both hands on either side of your lower back now.
- Now, extend your spine back and push your pelvis forward with your hands. Continue extending your neck until you are facing the ceiling.
- Do two to three sets, starting with ten repetitions. When you need a break from sitting at your desk, this is an ideal thing to do.
BIRD DOG:
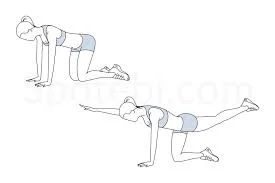
- Keep your hands under your shoulders and your knees under your hips to start on your hands and knees.
- Kick your right leg backward until it is in line with your chest while simultaneously raising your left arm and reaching it forward until it is in line with your torso.
- Hold this position for two to three seconds, then slowly go back to the beginning position.
- Repeat opposite.
- Perform two to three sets, switching sides for ten repetitions.
- To reduce neck strain, make sure your head, neck, and back are in a neutral position.
PRONE LYING ON FOREARM:

- Starting in the prone position, which involves resting on your stomach, gradually raise yourself up on your elbows while maintaining your hips in contact with the floor.
- Return to the prone position (lying face down) after holding the prop-up position for ten to fifteen seconds.
- Increase gradually until you can hold the final position for 30 seconds. Try to perform this stretch ten times.
- Start slowly and cautiously because you might not be able to handle this position at first.
PRONE LYING ON HAND

- You can progress to the more challenging variation of this stretch once you’ve perfected the half-cobra pose. Starting with your stomach in the prone position (facing down), gradually raise your hands while maintaining a relaxed lower back and pelvis in contact with the floor.
- For ten seconds, maintain the prop-up position. Try to perform this stretch ten times.
- If it feels comfortable, try holding this stance for 20 to 30 seconds at a time.
CAT AND CAMEL
- Get on your hands and knees to start this stretch. As you look towards the ceiling, let your stomach to “drop” towards the floor.
- After that, release your breath, slowly round your spine, press your hands into the floor, and bend your neck slightly so that you can see your feet.
- Do two to three sets of this stretch, aiming for ten repetitions.
PLANK

Start by resting your forearms against the mat while you are on your stomach.
- In order to rest on your forearms and toes, raise your body by using your core.
- For 20 to 30 seconds, maintain the plank position.
- Try to complete this workout five to ten times.
- When you’re ready, extend the duration you hold the plank by 10 seconds at a time to increase the intensity.
- Throughout the entire workout, make sure your back remains straight.
STATIC ABDOMINIS:
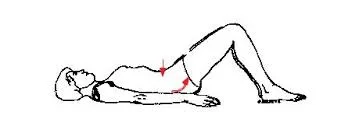
- Place your feet flat on the floor and lie on your back.
- Squeeze your abdominal muscles, flatten your lower back, and push your belly button toward the floor as you release the breath.
- Hold for five seconds. Calm down.
- Repeat ten times, each time holding for five seconds.
BRIDGING:
- With both knees at a 90-degree angle, lie on your back.
- Then, to get the shoulders, hips, and knees in a straight line, press your feet into the ground, tighten or squeeze your buttocks, and raise your hips off the ground.
- After holding for roughly five seconds, carefully return your hips to the floor and take a ten-second break.
- Do this ten times.
HAMSTRING STRETCH:

- To begin, flex your hip and knee to a 90-degree angle while resting flat on your back.
- With your opposing foot still firmly planted on the floor, steadily extend your bent knee toward the ceiling until you feel a stretch.
- Don’t move your spine; keep it straight.
- After 15 to 30 seconds of holding this stance, change your feet.
FAQs
Herniated disks are also known as ruptured or slipped discs. A herniated disk is more likely to produce pain than a bulging disk because it often protrudes more and is more prone to irritate nerve roots.
The good news is that discomfort caused by a herniated disc typically goes away on its own within six months, 90% of the time. Your doctor would probably advise you to start by taking an over-the-counter painkiller, Physical Therapy, and avoiding activities that make you feel pain or discomfort.
Rarely, a herniated disk might compress the cauda equina nerves as well as the entire spinal canal. In rare cases, immediate surgery may be necessary to prevent paralysis or lasting disability. Seek immediate medical help if you experience: worsening symptoms.
Depending on how far the nucleus has moved toward the outer annulus, there are four stages of a herniated disc.
Stage 1: Disc Compression
Stage 2: Bulging Disc
Stage 3: Disc Protrusion
Stage 4: Herniated Disc
Even if a slipped disc is the root of the issue, your body will likely be able to resolve it on its own in six weeks. The majority of treatments hardly ever slow down healing. Massages or hot packs may make you feel better.
A herniated disc is not always permanent, and many individuals experience symptom relief with conservative treatments like physical therapy, rest, and medication. However, rarely is surgery required.
A slipped disc may be the reason for a pinched nerve. Serious health problems, including impotence and problems getting pregnant, might result from a bulging or slipping L4-L5 disc. Infertility, loss of bowel or bladder control, paralysis of one or both legs, and even death can result from it.





53 Comments