Psoriasis
Table of Contents
What is Psoriasis?
Psoriasis is a chronic autoimmune condition that causes the rapid buildup of skin cells. This buildup of cells causes scaling on the skin’s surface.
Inflammation and redness around the scales is fairly common. Typical psoriatic scales are whitish-silver and develop in thick, red patches. Sometimes, these patches will crack and bleed.
Psoriasis is the result of a sped-up skin production process. Typically, skin cells grow deep in the skin and slowly rise to the surface. Eventually, they fall off. The typical life cycle of a skin cell is one month.
In people with psoriasis, this production process may occur in just a few days. Because of this, skin cells don’t have time to fall off. This rapid overproduction leads to the buildup of skin cells.
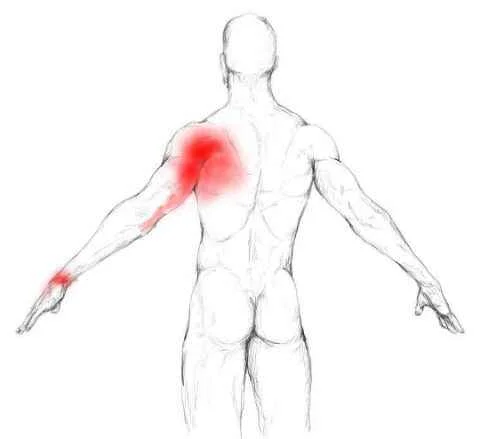
Scales typically develop on joints, such elbows and knees. They may develop anywhere on the body, including the:
- hands
- feet
- neck
- scalp
- face
~Less common types of psoriasis affect the nails, the mouth, and the area around genitals.
~According to the American Academy of Dermatology (AAD), around 7.5 million Americans have psoriasis. It’s commonly associated with several other conditions, including:-
-type 2 diabetes
-inflammatory bowel disease
-heart disease
-psoriatic arthritis
There are several types of psoriasis. These include:
- Plaque psoriasis. The most common form, plaque psoriasis causes dry, raised, red skin lesions (plaques) covered with silvery scales. The plaques might be itchy or painful and there may be few or many. They can occur anywhere on your body, including your genitals and the soft tissue inside your mouth.
- Nail psoriasis. Psoriasis can affect fingernails and toenails, causing pitting, abnormal nail growth and discoloration. Psoriatic nails might loosen and separate from the nail bed (onycholysis). Severe cases may cause the nail to crumble.
- Guttate psoriasis. This type primarily affects young adults and children. It’s usually triggered by a bacterial infection such as strep throat. It’s marked by small, water-drop-shaped, scaling lesions on your trunk, arms, legs and scalp. The lesions are covered by a fine scale and aren’t as thick as typical plaques are. You may have a single outbreak that goes away on its own, or you may have repeated episodes.
- Inverse psoriasis. This mainly affects the skin in the armpits, in the groin, under the breasts and around the genitals. Inverse psoriasis causes smooth patches of red, inflamed skin that worsen with friction and sweating. Fungal infections may trigger this type of psoriasis.
- Pustular psoriasis. This uncommon form of psoriasis can occur in widespread patches (generalized pustular psoriasis) or in smaller areas on your hands, feet or fingertips. It generally develops quickly, with pus-filled blisters appearing just hours after your skin becomes red and tender. The blisters may come and go frequently. Generalized pustular psoriasis can also cause fever, chills, severe itching and diarrhea.
- Erythrodermic psoriasis. The least common type of psoriasis, erythrodermic psoriasis can cover your entire body with a red, peeling rash that can itch or burn intensely.
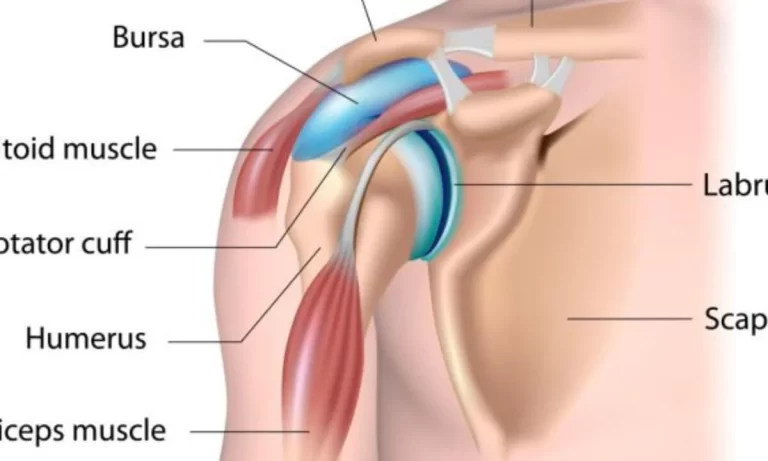
- ~Psoriatic arthritis. In addition to inflamed, scaly skin, psoriatic arthritis causes swollen, painful joints that are typical of arthritis. Sometimes the joint symptoms are the first or only manifestation of psoriasis or at times only nail changes are seen. Symptoms range from mild to severe, and psoriatic arthritis can affect any joint. Although the disease usually isn’t as crippling as other forms of arthritis, it can cause stiffness and progressive joint damage that in the most serious cases may lead to permanent deformity.
Causes of Psoriasis:
~The cause of psoriasis isn’t fully understood, but it’s thought to be related to an immune system problem with T cells and other white blood cells, called neutrophils, in your body.
~T cells normally travel through the body to defend against foreign substances, such as viruses or bacteria.
~But if you have psoriasis, the T cells attack healthy skin cells by mistake, as if to heal a wound or to fight an infection.
~Overactive T cells also trigger increased production of healthy skin cells, more T cells and other white blood cells, especially neutrophils. These travel into the skin causing redness and sometimes pus in pustular lesions. Dilated blood vessels in psoriasis-affected areas create warmth and redness in the skin lesions.
~The process becomes an ongoing cycle in which new skin cells move to the outermost layer of skin too quickly — in days rather than weeks. Skin cells build up in thick, scaly patches on the skin’s surface, continuing until treatment stops the cycle.
~Just what causes T cells to malfunction in people with psoriasis isn’t entirely clear. Researchers believe both genetics and environmental factors play a role.
Psoriasis triggers:
~Psoriasis typically starts or worsens because of a trigger that you may be able to identify and avoid. Factors that may trigger psoriasis include:
- Infections, such as strep throat or skin infections
- Injury to the skin, such as a cut or scrape, a bug bite, or a severe sunburn
- Stress
- Smoking
- Heavy alcohol consumption
- Vitamin D deficiency
- Certain medications — including lithium, which is prescribed for bipolar disorder, high blood pressure medications such as beta blockers, antimalarial drugs, and iodides.
Risk factors:
Anyone can develop psoriasis, but these factors can increase your risk of developing the disease:
- Family history. This is one of the most significant risk factors. Having one parent with psoriasis increases your risk of getting the disease, and having two parents with psoriasis increases your risk even more.
- Viral and bacterial infections. People with HIV are more likely to develop psoriasis than people with healthy immune systems are. Children and young adults with recurring infections, particularly strep throat, also may be at increased risk.
- Stress. Because stress can impact your immune system, high stress levels may increase your risk of psoriasis.
- Obesity. Excess weight increases the risk of psoriasis. Lesions (plaques) associated with all types of psoriasis often develop in skin creases and folds.
- Smoking. Smoking tobacco not only increases your risk of psoriasis but also may increase the severity of the disease. Smoking may also play a role in the initial development of the disease.
Complications:
If you have psoriasis, you’re at greater risk of developing certain diseases. These include:
- Psoriatic arthritis. This complication of psoriasis can cause joint damage and a loss of function in some joints, which can be debilitating.
- Eye conditions. Certain eye disorders — such as conjunctivitis, blepharitis and uveitis — are more common in people with psoriasis.
- Obesity. People with psoriasis, especially those with more severe disease, are more likely to be obese. It’s not clear how these diseases are linked, however. The inflammation linked to obesity may play a role in the development of psoriasis. Or it may be that people with psoriasis are more likely to gain weight, possibly because they’re less active because of their psoriasis.
- Type 2 diabetes. The risk of type 2 diabetes rises in people with psoriasis. The more severe the psoriasis, the greater the likelihood of type 2 diabetes.
- High blood pressure. The odds of having high blood pressure are higher for people with psoriasis.
- Cardiovascular disease. For people with psoriasis, the risk of cardiovascular disease is twice as high as it is for those without the disease. Psoriasis and some treatments also increase the risk of irregular heartbeat, stroke, high cholesterol and atherosclerosis.
- Metabolic syndrome. This cluster of conditions — including high blood pressure, elevated insulin levels and abnormal cholesterol levels — increases your risk of heart disease.
- Other autoimmune diseases. Celiac disease, sclerosis and the inflammatory bowel disease called Crohn’s disease are more likely to strike people with psoriasis.
- Parkinson’s disease. This chronic neurological condition is more likely to occur in people with psoriasis.
- Kidney disease. Moderate to severe psoriasis has been linked to a higher risk of kidney disease.
- Emotional problems. Psoriasis can also affect your quality of life. Psoriasis is associated with low self-esteem and depression. You may also withdraw socially.
Symptoms of Psoriasis:
~Psoriasis signs and symptoms are different for everyone. Common signs and symptoms include:
- Red patches of skin covered with thick, silvery scales
- Small scaling spots (commonly seen in children)
- Dry, cracked skin that may bleed
- Itching, burning or soreness
- Thickened, pitted or ridged nails
- Swollen and stiff joints
~Psoriasis patches can range from a few spots of dandruff-like scaling to major eruptions that cover large areas.
~Most types of psoriasis go through cycles, flaring for a few weeks or months, then subsiding for a time or even going into complete remission.
The most common triggers for psoriasis include:
~Stress:-Unusually high stress may trigger a flare-up. If you learn to reduce and manage your stress, you can reduce and possibly prevent flare-ups.
Alcohol
~Heavy alcohol use can trigger psoriasis flare-ups. If you excessively use alcohol, psoriasis outbreaks may be more frequent. Reducing alcohol consumption is smart for more than just your skin, too. Your doctor can help you form a plan to quit drinking if you need help.
Injury
~An accident, cut, or scrape may trigger a flare-up. Shots, vaccines, and sunburns can also trigger a new outbreak.
~Medications:-Some medications are considered psoriasis triggers. These medications include:
- lithium.
- antimalarial medications.
- high blood pressure medication
- Infection:-Psoriasis is caused, at least in part, by the immune system mistakenly attacking healthy skin cells. If you’re sick or battling an infection, your immune system will go into overdrive to fight the infection. This might start another psoriasis flare-up. Strep throat is a common trigger.
Treatment of Psoriasis:
Topical treatments:
Used alone, creams and ointments that you apply to your skin can effectively treat mild to moderate psoriasis. When the disease is more severe, creams are likely to be combined with oral medications or light therapy. Topical psoriasis treatments include:
- Topical corticosteroids. These drugs are the most frequently prescribed medications for treating mild to moderate psoriasis. They reduce inflammation and relieve itching and may be used with other treatments. Mild corticosteroid ointments are usually recommended for sensitive areas, such as your face or skin folds, and for treating widespread patches of damaged skin. Your doctor may prescribe stronger corticosteroid ointment for smaller, less sensitive or tougher-to-treat areas. Long-term use or overuse of strong corticosteroids can cause thinning of the skin. Topical corticosteroids may stop working over time. It’s usually best to use topical corticosteroids as a short-term treatment during flares.
- Vitamin D analogues. These synthetic forms of vitamin D slow skin cell growth. Calcipotriene (Dovonex) is a prescription cream or solution containing a vitamin D analogue that treats mild to moderate psoriasis along with other treatments. Calcipotriene might irritate your skin. Calcitriol (Vectical) is expensive but may be equally effective and possibly less irritating than calcipotriene.
- Anthralin. This medication helps slow skin cell growth. Anthralin (Dritho-Scalp) can also remove scales and make skin smoother. But anthralin can irritate skin, and it stains almost anything it touches. It’s usually applied for a short time and then washed off.
- Topical retinoids. These are vitamin A derivatives that may decrease inflammation. The most common side effect is skin irritation. These medications may also increase sensitivity to sunlight, so while using the medication apply sunscreen before going outdoors. The risk of birth defects is far lower for topical retinoids than for oral retinoids. But tazarotene (Tazorac, Avage) isn’t recommended when you’re pregnant or breast-feeding or if you intend to become pregnant.
- Calcineurin inhibitors. Calcineurin inhibitors — tacrolimus (Prograf) and pimecrolimus (Elidel) — reduce inflammation and plaque buildup. Calcineurin inhibitors are not recommended for long-term or continuous use because of a potential increased risk of skin cancer and lymphoma. They may be especially helpful in areas of thin skin, such as around the eyes, where steroid creams or retinoids are too irritating or may cause harmful effects.
- Salicylic acid. Available over-the-counter (nonprescription) and by prescription, salicylic acid promotes sloughing of dead skin cells and reduces scaling. Sometimes it’s combined with other medications, such as topical corticosteroids or coal tar, to increase its effectiveness. Salicylic acid is available in medicated shampoos and scalp solutions to treat scalp psoriasis.
- Coal tar. Derived from coal, coal tar reduces scaling, itching and inflammation. Coal tar can irritate the skin. It’s also messy, stains clothing and bedding, and has a strong odor. Coal tar is available in over-the-counter shampoos, creams and oils. It’s also available in higher concentrations by prescription. This treatment isn’t recommended for women who are pregnant or breast-feeding.
- Moisturizers. Moisturizing creams alone won’t heal psoriasis, but they can reduce itching, scaling and dryness. Moisturizers in an ointment base are usually more effective than are lighter creams and lotions. Apply immediately after a bath or shower to lock in moisture.
Light therapy (phototherapy):
This treatment uses natural or artificial ultraviolet light. The simplest and easiest form of phototherapy involves exposing your skin to controlled amounts of natural sunlight.
Other forms of light therapy include the use of artificial ultraviolet A (UVA) or ultraviolet B (UVB) light, either alone or in combination with medications.
- Sunlight. Exposure to ultraviolet (UV) rays in sunlight or artificial light slows skin cell turnover and reduces scaling and inflammation. Brief, daily exposures to small amounts of sunlight may improve psoriasis, but intense sun exposure can worsen symptoms and cause skin damage. Before beginning a sunlight regimen, ask your doctor about the safest way to use natural sunlight for psoriasis treatment.
- UVB phototherapy. Controlled doses of UVB light from an artificial light source may improve mild to moderate psoriasis symptoms. UVB phototherapy, also called broadband UVB, can be used to treat single patches, widespread psoriasis and psoriasis that resists topical treatments. Short-term side effects may include redness, itching and dry skin. Using a moisturizer may help decrease these side effects.
- Narrow band UVB phototherapy. A newer type of psoriasis treatment, narrow band UVB phototherapy may be more effective than broadband UVB treatment. It’s usually administered two or three times a week until the skin improves, and then maintenance may require only weekly sessions. Narrow band UVB phototherapy may cause more-severe and longer lasting burns, however.
- Goeckerman therapy. Some doctors combine UVB treatment and coal tar treatment, which is known as Goeckerman treatment. The two therapies together are more effective than either alone because coal tar makes skin more receptive to UVB light.
- Psoralen plus ultraviolet A (PUVA). This form of photochemotherapy involves taking a light-sensitizing medication (psoralen) before exposure to UVA light. UVA light penetrates deeper into the skin than does UVB light, and psoralen makes the skin more responsive to UVA exposure. This more aggressive treatment consistently improves skin and is often used for more-severe cases of psoriasis. Short-term side effects include nausea, headache, burning and itching. Long-term side effects include dry and wrinkled skin, freckles, increased sun sensitivity, and increased risk of skin cancer, including melanoma.
- Excimer laser. This form of light therapy, used for mild to moderate psoriasis, treats only the involved skin without harming healthy skin. A controlled beam of UVB light is directed to the psoriasis plaques to control scaling and inflammation. Excimer laser therapy requires fewer sessions than does traditional phototherapy because more powerful UVB light is used. Side effects can include redness and blistering.
Oral or injected medications:
If you have severe psoriasis or it’s resistant to other types of treatment, your doctor may prescribe oral or injected drugs. This is known as systemic treatment. Because of severe side effects, some of these medications are used for only brief periods and may be alternated with other forms of treatment.
- Retinoids. Related to vitamin A, this group of drugs may help if you have severe psoriasis that doesn’t respond to other therapies. Side effects may include lip inflammation and hair loss. And because retinoids such as acitretin (Soriatane) can cause severe birth defects, women must avoid pregnancy for at least three years after taking the medication.
- Methotrexate. Taken orally, methotrexate (Rheumatrex) helps psoriasis by decreasing the production of skin cells and suppressing inflammation. It may also slow the progression of psoriatic arthritis in some people. Methotrexate is generally well-tolerated in low doses but may cause upset stomach, loss of appetite and fatigue. When used for long periods, it can cause a number of serious side effects, including severe liver damage and decreased production of red and white blood cells and platelets.
- Cyclosporine. Cyclosporine (Gengraf, Neoral) suppresses the immune system and is similar to methotrexate in effectiveness, but can only be taken short-term. Like other immunosuppressant drugs, cyclosporine increases your risk of infection and other health problems, including cancer. Cyclosporine also makes you more susceptible to kidney problems and high blood pressure — the risk increases with higher dosages and long-term therapy.
- Drugs that alter the immune system (biologics). Several of these drugs are approved for the treatment of moderate to severe psoriasis. They include etanercept (Enbrel), infliximab (Remicade), adalimumab (Humira), ustekinumab (Stelara), golimumab (Simponi), apremilast (Otezla), secukinumab (Cosentyx) and ixekizumab (Taltz). Most of these drugs are given by injection (apremilast is oral) and are usually used for people who have failed to respond to traditional therapy or who have associated psoriatic arthritis. Biologics must be used with caution because they have strong effects on the immune system and may permit life-threatening infections. In particular, people taking these treatments must be screened for tuberculosis.
- Other medications. Thioguanine (Tabloid) and hydroxyurea (Droxia, Hydrea) are medications that can be used when other drugs can’t be given.