Parkinson’s disease
Table of Contents
What is Parkinson’s disease?
Parkinson’s disease is a progressive nervous system condition that affects the movement of the body. It is a brain disorder that causes uncontrollable or unintended movements, such as stiffness, shaking, and difficulty with coordination and balance. Symptoms initiate gradually, sometimes starting with a hardly noticeable tremor in just one hand. Tremors are common, but the disorder also commonly causes slowing of movement or stiffness. It can also cause a wide range of other effects on a patient’s senses, mental health, thinking ability, and more.
In the early phase of Parkinson’s disease, the patient’s face may show no or little expression. A patient’s arms may not swing while they walk. The patient’s speech may become slurred or soft. Parkinson’s disease symptoms worsen as their condition progresses over time. As the condition progresses, patients may have difficulty talking and walking. They may also have behavioral and mental changes, depression, sleep problems, memory difficulties, and fatigue.
Although Parkinson’s disease can not be cured, medicines might significantly improve their symptoms. Occasionally, doctors may suggest surgery to regulate certain regions of patients’ brains and improve their symptoms.
While virtually any person could be at risk for developing Parkinson’s disease, few research studies suggest this disease affects more men than women, in comparison. It is not clear why, but studies are underway to understand factors that may raise a person’s risk. One main risk is age: Although most patients with Parkinson’s first develop the disease after age 60, about 5% to 12% feel onset before the age of 50. Early-onset forms of Parkinson’s are frequent, but not forever, inherited, and few forms have been linked to specific gene mutations.
The condition is named after English doctor James Parkinson, who published the first in-depth description in an essay on the Shaking Palsy, in 1817. Public awareness campaigns include World Parkinson’s Day on the birthday of James Parkinson, on 11th April, and the use of a red tulip as the symbol of the disease.
What are the symptoms of Parkinson’s disease?
Parkinson’s disease symptoms and signs can be different for individuals. Early signs may go unnoticed and are mild. Symptoms often start on one side of the patient’s body and usually remain worse on that side, even after symptoms begin to affect the bilateral side.
The mainly known symptoms of Parkinson’s disease involve loss of muscle control. But, experts now know that muscle control-related issues are not the single possible symptoms of Parkinson’s disease.
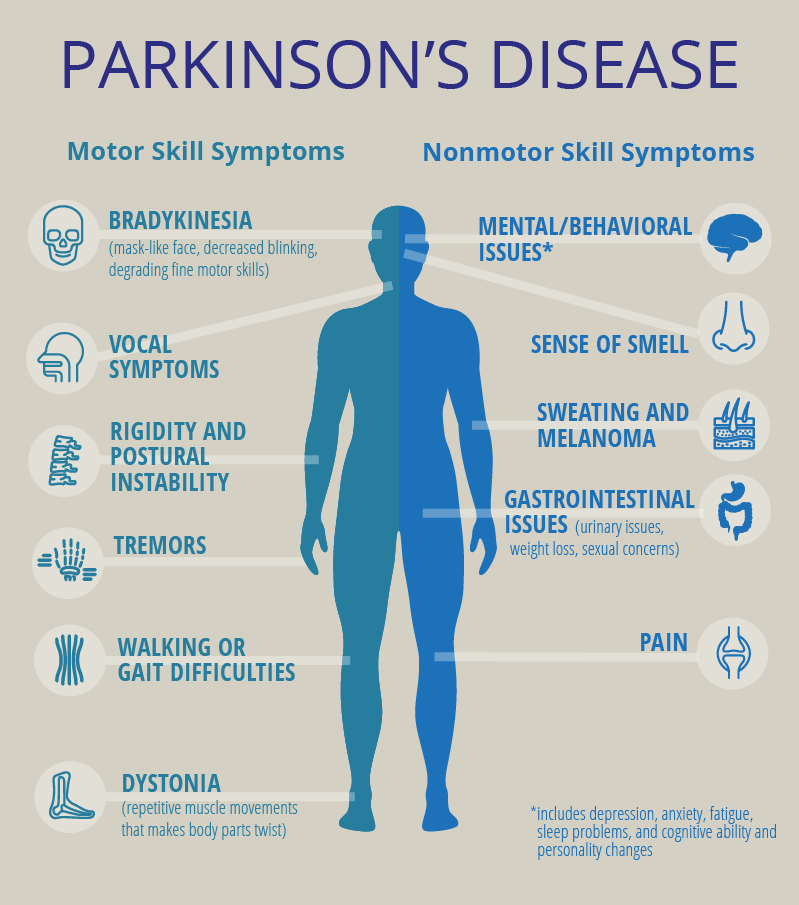
Motor-related symptoms
Motor symptoms, which means movement-related symptoms of Parkinson’s disease include:
Tremor
Tremor or shaking generally starts in a limb often the patient’s fingers or hand. A patient may rub their thumb and forefinger forth and back, known as a pill-rolling tremor. The patient’s hand may tremble when it is at rest. This is a rhythmic shaking of muscles even when the patient is not using them and happens in approximately 80% of Parkinson’s disease cases. Resting tremors are unique from essential tremors, which do not usually happen when muscles are at rest.
Slowed movement (bradykinesia)
Parkinson’s disease diagnosis requires that patients have this type of symptom. Over time, Parkinson’s disease may slow the patient’s movement, be time-consuming, and make simple tasks difficult or hard. Patients’ steps may become shorter when they walk. It may be hard to get out of a chair or bed. A patient may drag their feet as they try to walk. Patients who have this, usually describe it as muscle weakness, but it happens because of muscle control problems, and there is no actual loss of strength.
Rigidity or stiffness
Rigid muscle or muscle stiffness may occur in any part of the patient’s body. The stiff muscles can be painful and limit the patient’s range of motion of joints.
Lead-pipe rigidity and cogwheel stiffness are the most general symptoms of Parkinson’s disease.
Lead-pipe rigidity is an unchanging, constant stiffness while moving a body part.
Cogwheel stiffness happens when patients combine lead-pipe rigidity and tremor. It gets its name because of the stop-and-go appearance of the movements like seen as the second hand on a mechanical clock), and the jerky movement.
Impaired posture and balance
Patients’ posture may become stooped, or they may have balance problems as a result of Parkinson’s disease. The stiffness and slowed movements of Parkinson’s disease cause a hunched over or stooped stance posture. This generally appears as the disease gets worse over time.
Unstable walking gait
Patients with Parkinson’s disease frequently develop a Parkinsonism gait that includes a tendency to lean forward; take quick, small steps; and reduce swinging their arms. While walking, turning may take several steps. Patients also may have trouble continuing or initiating movement.
Loss of automatic movements
Patients may have a decreased ability to perform unconscious movements, including smiling, blinking, or swinging their arms when they walk.
Additional motor symptoms can include:
Blinking is less frequent than usual. This is also a symptom of decreased control of facial muscles.
Cramped or small handwriting. This is known as micrographia, this happens due to muscle control problems. It may become hard to write, and the patient’s writing may appear small.
Drooling. This is another symptom that happens due to loss of facial muscle control.
Mask-like facial expression. It is known as hypomimia, which means facial expressions change a very small amount or not at all.
Trouble swallowing. It is known as dysphagia, which happens with reduced throat muscle control. This can lead to dehydration and malnutrition. It increases the risk of problems like choking or pneumonia.
Unusually soft speaking voice. It is called hypophonia, which happens because of reduced muscle control in the chest and throat. Patients may speak quickly, softly, slur, or hesitate before talking. The patient’s speech may be more mono-tonal not as general as individual.
Non-motor symptoms
Several symptoms are possible that are not connected to muscle control and movement. In past years, experts believed non-motor symptoms were risk factors for Parkinson’s disease while seen before motor symptoms. But, there is a growing amount of proof that these symptoms can appear in the earliest stages of the disease, which means these symptoms might be warning signs that initiate years or even decades before motor symptoms.
- Nerve pain. It can cause unpleasant sensations, such as coldness, burning, or numbness.
- Problems with urination. It is also known as urinary incontinence, which includes such as having to get up often during the night to pee or unintentionally peeing.
- Erectile dysfunction. It is an inability to sustain or obtain an erection in men
- Sexual dysfunction. Difficulty achieving an orgasm and becoming sexually aroused in women
- Dizziness, fainting, or blurred vision while moving from a lying or sitting position to a standing one, caused by a sudden drop in blood pressure
- Excessive sweating. It is known as hyperhidrosis
- Depression and other emotional changes.
- Loss of sense of smell. It is known as anosmia.
- Sleep problems (insomnia) such as rapid eye movement (REM), periodic limb movement disorder (PLMD), behavior disorder, and restless legs syndrome, can result in over sleepiness during the daytime.
- Trouble focusing and thinking (Parkinson’s-related dementia).
- Dementia. It is a group of symptoms, including personality changes, more severe memory problems, seeing things that are not there means visual hallucinations, and believing things that are not truly known as delusions.
- Urinary problems or constipation
- Skin problems
- mild cognitive impairment. It includes some memory problems and problems with activities that require organization and planning.
Stages of Parkinson’s Disease
Hoehn and Yahr rating scale
“Parkinson’s is a neurological condition caused by breaking down or degeneration of cells in the nervous system,” said Dr. Shprecher. This understanding of the condition relies on the Hoehn and Yahr rating scale to classify the severity of symptoms. Based on disease progression, the scale is classified into five stages. The five stages help doctors diagnose how far the disease has developed.
Stage One
This is the mildest form of Parkinson’s disease. At this stage, there may be symptoms, but they are not severe enough to interfere with the overall lifestyle and daily tasks. In fact, the symptoms are so minimal or less at this stage that they are frequently missed. But friends and family may notice changes in the patient’s walking, posture, or facial expressions.
A distinct symptom of stage 1 Parkinson’s disease is that tremors and other difficulties in movement are generally seen on one side of the body. Prescribed medicines can work effectively to reduce and minimize symptoms at this stage.
Stage Two
Stage 2 is described as a moderate form of Parkinson’s disease, and the symptoms are much more noticeable than those seen in stage 1. Tremors, stiffness, and trembling may be more noticeable, and changes in facial expressions can see.
While muscle stiffness increases task completion, stage 2 does not impair balance. Walking difficulties may develop or increase, and the person’s posture may initiate to change.
Patients at this stage feel symptoms on both sides of the body but one side may only be minimally affected and sometimes have speech difficulties.
The majority of patients with stage 2 Parkinson’s can still live alone, but they may find that some tasks are difficult and take a longer time to complete. The progression from stage one to stage two can take a few months or even years and there is no solution to predict the patient’s progression.
Stage Three
This is the middle stage of Parkinson’s disease, and it marks the main turning point in the progression of the condition. Many of the symptoms are the same as seen in stage two, but patients are now more likely to experience loss of balance, slowness of movements, and decreased reflexes. So that falls become more general in stage 3.
Parkinson’s disease affects daily tasks such as dressing and eating at this level, but patients are still able to complete all that tasks. Medicines combined with occupational therapy may help reduce symptoms.
Stage Four
Symptoms are limiting and severe. Independence differentiates patients with stage 3 Parkinson’s disease from those with stage 4. During stage 4, it is possible to stand without support, but movement may need a walker or other type of assistive device. Many patients are unable to live alone at this stage of Parkinson’s because of significant decreases in reaction times and movement. Living alone at stage four or later may make many daily tasks not possible, and this can be hazardous.
Stage Five
This is the most advanced stage of Parkinson’s disease. Advanced stiffness in the legs can also cause freezing while standing, making patient impossible to walk or stand. Patients in this stage require wheelchairs, and they are often not able to stand on their own without falling. Around-the-clock assistance is required for all activities and to prevent falls. A patient may feel delusions and hallucinations.
Above given staging system is no longer in widespread use because staging this illness is less helpful than determining how it affects each patient’s life individually and then treating them accordingly.
Movement Disorder Society-Unified Parkinson’s Disease Rating Scale (MDS-UPDRS)
The Movement Disorder Society-Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) is healthcare’s main tool to classify this condition. The MDS-UPDRS evaluates four different areas of how Parkinson’s disease affects a patient:
Part 1: Non-motor aspects of experiences of daily living.
This section deals with non-motor or non-movement symptoms like depression, dementia, anxiety, and other mental ability and mental health-related problems. It also asks questions about constipation, pain, fatigue, incontinence, etc.
Part 2: Motor aspects of experiences of daily living.
This section deals with the effects on movement-related abilities and tasks. It includes the patient’s ability to eat, chew and swallow, speak, dress, and bathe themself if they have tremors and more.
Part 3: Motor examination.
A doctor uses this part to diagnose the movement-related effects of Parkinson’s disease. The criteria measure effects based on how a patient speaks, facial expressions, rigidity, and stiffness, walking gait and speed, balance, movement speed, tremors, etc.
Part 4: Motor complications.
This section includes a doctor determining how much of an impact the symptoms of Parkinson’s disease are affecting the patient’s life. That includes both the amount of time patients have some symptoms each day, and whether or not those symptoms affect how a patient spends his time.
Rating Scales
A doctor may refer to a scale to help them how the progression of the disease occurs. Parkinson’s stages correspond both to how much the disease affects a person’s daily activities and to the severity of movement symptoms. The most generally used rating scales focus on motor symptoms.
Hoehn and Yahr stages have a simple rating scale, first introduced in 1967. Doctors use it to describe how motor symptoms progress in Parkinson’s disease. Rates symptoms on a scale of 1 to 5. On this scale, 1 and 2 are early-stage, 2 and 3 are mid-stage, and 4 and 5 are advanced-stage Parkinson’s disease.
The Unified Parkinson’s Disease Rating Scale (UPDRS) is a more comprehensive tool used to account for non-motor symptoms, including mood, mental functioning, and social interaction. Identify cognitive difficulties, ability to carry out daily activities and treatment as well as complications.
New scales include knowledge of non-motor symptoms such as sense of smell.
While symptoms and disease progression are different for each patient, knowing the typical stages of Parkinson’s can help patient to cope with changes as they occur. Some patients experience the changes over 20 years or more. Others have the disease progresses more rapidly.
What causes Parkinson’s disease?
In Parkinson’s disease, some nerve cells or neurons in the part of the brain called the substantia nigra, is gradually die or break down. Nerve cells in this part of the brain are responsible for developing a chemical known as dopamine.
Dopamine acts as a messenger between the nervous system and parts of the brain that help control and coordinate movements of the body.
If these nerve cells become damaged or die, the amount of dopamine in the brain is decreased.
This means the part of the brain that controls movement cannot work as well as normal, causing movements to become abnormal and slow.
The loss of nerve cells is a lower-speed process. The symptoms of Parkinson’s disease generally only initiate to develop when approximately 80% of the nerve cells in the substantia nigra have been lost or damaged.
The cause of Parkinson’s disease is not known, but some factors appear to play a role, which include:
Genetics
A number of genetic factors have been shown to higher a person’s risk of developing Parkinson’s disease, but exactly how these genes make some individuals more susceptible to the condition is still unclear.
Parkinson’s disease can go in families because of faulty genes being passed to a child by their parents or family, however, it is rare for the condition to be inherited this way.
Environmental triggers
Exposure to certain environmental factors or toxins may increase the risk of Parkinson’s disease, but the risk is comparatively slow. It is been suggested that herbicides and pesticides used in farming and industrial pollution or traffic may contribute to the condition, but the proof linking environmental factors to Parkinson’s disease is not conclusive.
Researchers have also shown that a number of changes occur in the brains of patients with Parkinson’s disease, but it is not clear why these changes happen. These changes include:
The presence of Lewy bodies
Clumps of specific substances in the brain cells are microscopic results of Parkinson’s disease, which is known as Lewy bodies, and researchers reckon these Lewy bodies hold a vital clue to the cause of Parkinson’s disease.
Alpha-synuclein found within Lewy bodies
Many substances are found within Lewy bodies, scientists believe an essential one is the widespread and natural protein called alpha-synuclein means a-synuclein. It is found in all Lewy bodies in a clumped form that cells can not die or break down. This is now an essential focus among Parkinson’s disease researchers or doctors.
What are the risk factors for Parkinson’s disease?
Risk factors for Parkinson’s disease include:
Age
Young adults rarely have Parkinson’s disease. It ordinarily starts in late or middle life, and the risk increases with age. People generally develop the disease at approximately age 60 or older.
Heredity
Having a close relative with Parkinson’s disease increases the chances that a person will develop the condition. However, someone’s risks are still small unless they have many relatives in their family with Parkinson’s disease.
Sex
Men are more having chances to develop Parkinson’s disease than women.
Exposure to toxins
Ongoing exposure to pesticides and herbicides may slightly increase a person’s risk of Parkinson’s disease.
How to diagnose Parkinson’s disease?
No specific tests are present for a diagnosis of Parkinson’s disease. A doctor trained in nervous system conditions known as a neurologist will diagnose Parkinson’s disease based on patients’ medical history, a review of their symptoms and signs, and a physical and neurological examination.
What do Doctors see while diagnosing Parkinson’s disease?
Some physical signs and symptoms noticed by the patient or his or her family members and relatives are usually what prompts an individual to see the doctor. These are the symptoms most frequently noticed by patients or their families:
Shaking or tremor: It is called a resting tremor, a trembling of a foot or hand that happens while the patient is at rest and typically stops when he or she is moving or active.
Bradykinesia: It is the lowness of movement in the face, limbs, walking, or overall body.
Rigidity: It is stiffness in the legs, arms, or trunk
posture instability: It is trouble with balance, and possibly the patient may fall.
Once the patient is visiting the doctor’s office, the doctor:
Takes a medical and family history and does a physical examination.
Asks about past and current medicines. Some medicines may cause symptoms that are similar to Parkinson’s disease.
Performs a neurological examination, testing muscle tone, agility, balance, and gait.
A doctor may advise a specific single-photon emission computerized tomography (SPECT) scan called a dopamine transporter scan (DaTscan). However, this can help support the suspicion that someone has Parkinson’s disease, it is their signs, symptoms, and neurologic examination that ultimately identify the correct diagnosis. Most patients do not need a DaTscan. It involves a machine called a single-photon emission computed tomography (SPECT) scanner, similar to an MRI, and an injection of a small amount of a radioactive drug.
The drug binds to dopamine transmitters in the brain, showing where in the brain dopaminergic neurons are present because dopaminergic neurons are the source of dopamine in the brain; a loss of dopamine is what leads to Parkinson’s disease. The results of a DaTscan can not show that someone has Parkinson’s disease, but they can help their doctor rule out a Parkinson’s similar conditions or confirm a diagnosis.
A doctor may order lab tests, such as blood tests, to differentiate other conditions that may be causing the patient’s symptoms.
- Imaging tests such as ultrasound of the brain, an MRI, and PET scans also may be used to help differentiate other disorders. Imaging tests are not especially helpful for diagnosing Parkinson’s disease.
- In addition to physical examination, a doctor may give the patient carbidopa-levodopa (Sinemet, Rytary, others), a Parkinson’s disease medicine. A patient must be given a sufficient dose to show the benefit, as low doses for one day or two are not reliable. Essential improvement with this medicine will often confirm the patient’s diagnosis of Parkinson’s disease.
- few times it takes time to diagnose Parkinson’s disease. A doctor may recommend regular follow-up appointments with neurologists trained in movement disorders to evaluate a patient’s condition and symptoms over the period and diagnose Parkinson’s disease.
New lab tests can useful
Researchers have found some ways to test for possible indicators or causes of Parkinson’s disease. Both of these below given new tests involve the alpha-synuclein protein but test for it in new, not usual ways. While these tests can not tell patients what conditions they have because of misfolded alpha-synuclein proteins, that information can still help their health care provider make a diagnosis.
The two tests use the following methods.
- Spinal tap. One of these tests looks for misfolded alpha-synuclein proteins in cerebrospinal fluid, which is the fluid that surrounds a person’s spinal cord and brain. This test involves a spinal tap or lumbar puncture, where a doctor inserts a needle into the patient’s spinal canal to collect some cerebrospinal fluid for testing.
- Skin biopsy. This test involves a biopsy of surface nerve tissue. A biopsy includes collecting a tiny sample of the patient’s skin, including the nerves in the skin. The samples come from a spot on a patient’s back and two spots on their leg. Identifying the samples can help determine if a patient’s alpha-synuclein has a certain kind of malfunction or damage that could increase the risk of developing Parkinson’s disease.
Is Early Diagnosis Possible?

- Researchers are becoming more aware of symptoms of Parkinson’s that precede physical manifestations. Clues to the condition that sometimes show up before motor symptoms and before a formal diagnosis are known as prodromal symptoms. These include a sleep disturbance, the loss of sense of smell called REM behavior disorder, ongoing constipation that is not otherwise explained, and mood disorders, such as depression and anxiety.
How to treat Parkinson’s disease?
Parkinson’s disease can not be cured permanently, but medicines can help control a patient’s symptoms, frequently dramatically. In some more advanced or later cases, surgery may be required. A doctor may also recommend lifestyle changes, particularly ongoing aerobic exercise. In many cases, physiotherapy that focuses on stretching and balance also is essential. A speech-language pathologist may help improve a patient’s speech problems.
Medications
Medicines may help patients manage problems with movement, walking, and tremor. These medicines increase or substitute dopamine levels. Patients with Parkinson’s disease have low brain dopamine levels. However, dopamine can not be given directly, as it can not enter the patient’s brain. A patient may have significant improvement in his or her symptoms after beginning Parkinson’s disease treatment. Over time, however, the benefits of drugs often reduce or become less consistent. Patients can generally still control their symptoms fairly well.
Medications a doctor may prescribe include:
Carbidopa-levodopa
Levodopa, the most effective Parkinson’s disease medicine, is a natural chemical that passes into a patient’s brain and is converted to dopamine. Levodopa is combined with carbidopa or Lodosyn, which protects levodopa from early conversion to dopamine outside the patient’s brain. This lessens or prevents side effects such as nausea.
Side effects may include lightheadedness or nausea (orthostatic hypotension).
After years, as the patient’s condition progresses, the benefit from levodopa may become less stable, with a tendency to wax and wane means wearing off. Also, a patient may feel involuntary movements known as dyskinesia after taking higher doses of levodopa. A doctor may lessen a patient’s dose or adjust the times of their doses to control these types of effects.
Inhaled carbidopa-levodopa
Inbrija is in an inhaled form, which is a new brand-name drug-delivering carbidopa-levodopa. It may be useful in managing symptoms that arise when oral medicines suddenly stop working during the daytime.
Carbidopa-levodopa infusion
Duopa is a brand-name medicine made up of carbidopa and levodopa. But, it is administered through a feeding tube that delivers the medicines in a gel form directly to the small intestine. Duopa is for individuals with more-advanced Parkinson’s disease who still respond to carbidopa-levodopa, but who have a lot of instability in their response. Duopa is continually infused, due to this blood levels of the two drugs remain stable. Placement of the tube needs a tiny surgical procedure. Risks associated with having the tube include infections at the infusion site or the tube falling out.
Dopamine agonists
Unlike levodopa, dopamine agonists do not turn into dopamine but, they produce mimic dopamine effects in a patient’s brain. They are not as effective as levodopa in treating a patient’s symptoms. However, they stay longer and may be used with levodopa to smooth the sometimes on and off the effect of levodopa. Dopamine agonists include ropinirole (Requip), pramipexole (Mirapex), and rotigotine (Neupro, given as a patch). Apomorphine (Apokyn) is a short-acting injectable dopamine agonist used for fast and quick relief. Some of the side effects of dopamine agonists are the same as the carbidopa-levodopa side effects. But they can also include sleepiness, hallucinations, and compulsive behaviors such as gambling, hypersexuality, and eating. If a patient is taking these medicines and he or she behaves in a way that’s out of character for them, talk to a doctor.
MAO B inhibitors
These medications include rasagiline (Azilect), selegiline (Zelapar), and safinamide (Xadago). They help avoid the breakdown of brain dopamine by inhibiting the brain enzyme (MAO B) monoamine oxidase B, which metabolizes brain dopamine. Selegiline or zelapar given with levodopa may use to prevent wearing-off. Side effects of MAO B inhibitors may include nausea, headaches, or insomnia. While added to carbidopa-levodopa, these medicines raise the risk of hallucinations. These medicines are not often used in combination with certain narcotics or most antidepressants due to potentially dangerous but rare reactions. Check with a doctor before taking any extra medicines with an MAO B inhibitor.
Catechol O-methyltransferase (COMT) inhibitors
Opicapone (Ongentys) and Entacapone (Comtan) are the primary medicines in this category. This medicine mildly takes a longer time to the effect of levodopa therapy by blocking an enzyme that breaks down dopamine. Side effects, including a higher risk of involuntary movements known as dyskinesia, mainly result from an enhanced levodopa effect. Other side effects include nausea, diarrhea, or vomiting. Tolcapone (Tasmar) is another COMT inhibitor that is rarely prescribed due to the risk of liver failure and serious liver damage.
Anticholinergics
These medicines were used for a number of years to help control the tremor associated with Parkinson’s disease. Several anticholinergic medications are available, including trihexyphenidyl or benztropine (Cogentin). But, their modest benefits are often offset by side effects such as constipation, dry mouth, impaired memory, confusion, hallucinations, and impaired urination.
Amantadine
Doctors may prescribe amantadine single to provide short-term relief of symptoms of early, mild stage Parkinson’s disease. It may also be given with carbidopa-levodopa therapy during the later or advanced stages of Parkinson’s disease to control involuntary movements (dyskinesia) induced by carbidopa-levodopa. Side effects may include ankle swelling, a purple mottling of the skin, or hallucinations.
Surgical procedures
Placement of electrode and device location in deep brain stimulation.
- Deep brain stimulation
- In deep brain stimulation (DBS), surgeons implant electrodes into a particular part of a patient’s brain. The electrodes are connected to a generator implanted in the patient’s chest near their clavicle that sends electrical pulses to his or her brain and may reduce the symptoms of Parkinson’s disease.
- A doctor may adjust a patient’s settings as required to treat his condition. Surgery involves risks, including strokes, infections, or brain hemorrhage. Few patients experience complications due to stimulation or problems with the DBS system, and a doctor may need to replace or adjust a few parts of the system.
- Deep brain stimulation is most frequently offered to a patient with advanced Parkinson’s disease who have unstable medicine (levodopa) responses. DBS can stabilize medication fluctuations, halt or reduce involuntary movements (dyskinesia), reduce rigidity, reduce tremors, and improve slowing of movement.
- DBS is effective in controlling fluctuating and erratic responses to levodopa or for controlling dyskinesia that doesn’t improve with medicine adjustments, but DBS is not helpful for problems that do not respond to levodopa therapy apart from a tremor. A tremor can be controlled by Deep brain stimulation (DBS) even if the tremor is not very responsive to levodopa. DBS may provide sustained advantages for Parkinson’s symptoms, but it does not keep Parkinson’s disease from progressing.
Experimental treatments
Researchers are inventing other possible therapies or treatments that could help with Parkinson’s disease. While these are not widely available, they do offer hope to a patient with this condition. Few of the experimental treatment approaches include:
Stem cell transplants
These add new dopamine-using neurons into the patient’s brain to take over for damaged neurons.
Neuron-repair treatments
These treatments try to repair damaged neurons and encourage new neurons to develop.
Gene therapies and gene-targeted treatments
These treatments target particular mutations that cause Parkinson’s disease. Few also boost the effectiveness of levodopa or other medical treatments.
Supportive therapies
There are many therapies that can make a patient confident in living with Parkinson’s disease easier and help a patient deal with his or her symptoms on a day-to-day basis.
Physiotherapy treatment
A physiotherapist can work with a patient to relieve joint pain and muscle stiffness through movement or manipulation and exercise. The physiotherapist aims to make moving easier and improve a patient’s flexibility and walking. They also try to improve a patient’s fitness levels and ability to manage things for them-self.
Occupational therapy
An occupational therapist can identify areas of difficulty in a patient’s everyday life, such as dressing by them-self or getting to the market or local shops. They can help a patient work out practical ways and ensure a patient’s home is safe and properly set up for him. This will help a patient to maintain his independence for as long as possible.
Speech and language therapy
Many patients with Parkinson’s disease have swallowing difficulties known as dysphagia and problems with their speech.
A speech and language therapist can frequently help a patient to improve these problems by teaching swallowing and speaking exercises or by providing assistive aids.
Diet advice
For a few patients with Parkinson’s disease, making dietary changes can help improve some symptoms.
These changes can include:
Increase the amount of salt in a patient’s diet and eat frequent, small meals to avoid issues with low blood pressure such as dizziness when they stand up fast.
Increase the amount of fiber in a patient’s diet and make sure they are drinking enough fluid to decrease constipation.
Make changes to a patient’s diet to avoid unintentional weight loss.
Tai Chi
This type of exercise promotes coordination and balance, so it stands to reason that it can be beneficial for patients with Parkinson’s disease.
Yoga
The practice of yoga is known to help increase balance and flexibility, and yoga may have the same effects on patients with Parkinson’s disease. Yoga, particularly if it is adapted for the needs of patients with a movement disorder like Parkinson’s disease can increase balance, mobility, strength, and flexibility. It may also help improve mood and help a patient sleep better.
Massage Therapy
The effectiveness of massage in relieving side effects of Parkinson’s disease, mainly tremors looks clear, even if that relief is not permanent. A review of one study showed a measurable decrease in resting tremor and muscle rigidity immediately after a 60-minute massage
Weight training
- Movement Therapies
Because Parkinson’s disease affects balance and leads to a gradual reduction of motor skills, some movement therapies may help counteract those effects.
- The Alexander Technique, a discipline that improves balance and posture may help patients with Parkinson’s disease retain mobility.
- The Feldenkrais Method aims to retrain the body to do hard and difficult movements. Even if a patient does not participate in “official” movement therapies, activities like dancing and strength training mean weight lifting or using machines at a gym can help alleviate some symptoms.
Acupuncture
Acupuncture is a staple of traditional Chinese medicine, with the basic principle being that simulating points along the body’s meridians or energy pathways can reduce pain among other positive benefits. For that reason, it is mostly used to treat Parkinson’s disease in China and other countries.
What is the Physiotherapy treatment for Parkinson’s disease?
It is remembered that optimal outcome is achieved through the combination with others from a team of health and social care workers or professionals with expertise in other domains of Parkinson’s disease, from family, volunteers, and friends.
Aims of Physiotherapy Treatment
- Improve and maintain levels of independence and function, which will help to improve a patient’s quality of life.
- Use movement and exercise strategies to improve mobility
- Improve and Correct abnormal posture and movement patterns, where required
- Maximize joint flexibility and muscle strength
- Improve and correct posture and balance, and reduce risks of falls
- Maintain an effective cough and a good breathing pattern
- Educate the patient with Parkinson’s disease and their family members or carer
- Improve the effects of drug therapy
Exercise
In the earlier stages of diagnosis, greater emphasis is placed on self-management and education. The patient should be encouraged to participate in physical exercise and continue being active for as long as possible. Essential respiratory complications develop in many patients as their Parkinson’s disease progresses, so attention should be paid to managing and monitoring encroaching weakness of respiratory muscles and rigidity of the thoracic cage.
Exercise for neuroprotection mainly focuses on endurance and uses motor learning principles approaches, such as dual-task training and mental imagery. Neuroprotection training is to be effective and should be introduced in the early phases, but helps at all stages. It involves powerful, complex, and intensive exercises.
The exercise undertaken in a group setting has the added value of providing a social connection for those who are newly diagnosed, or those becoming increasingly isolated as the condition progresses, so they can see the advantages of maintaining activity and exercise. A group environment also permits time for patients to ask questions and discuss their symptoms and own treatment plan strategies with another one.
The transition Care setting improves the functioning and independence of the patients to delay their entry into aged residential care. It provides goal-oriented, time-limited, and therapy-focused packages of services to older patients after a hospital stay which includes low-intensity therapy.
Physical activity particularly, aerobic exercise might slow down depression and motor skill degeneration. Moreover, it increases the living quality of life of patients with Parkinson’s disease. A randomized controlled trial study showed favorable outcomes with horticultural intervention and exercise programs for older adults with memory problems and depression.
Quality of life may be improved when performing strength training against external resistance such as weight machines, cycle ergometers, therapeutic putty, elastic and, weight cuffs. This also improves gait parameters, physical parameters, such as balance and coordination, and physical performance but the muscle strength does not increase necessarily.
Executing a dual-task such as talking while walking, is generally difficult in patients with Parkinson’s. Training this with Motor Cognitive Dual-Task training improves dual-task ability and might improve balance, gait, and cognition.
Progressive resistance training (PRT) is effective in improving functional performance and decreasing bradykinesia in patients with mild to moderate Parkinson’s Disease.
Movement Strategy Training
Basal ganglia disorders cause deficits in the generation of automatic or internal behavior. Strategies such as physical or attentional cues and combined therapies can help reduce some of the resultant problems and, hence have become an increasingly utilized method of intervention for patients with Parkinson’s disease.
Music-based movement therapy
It is a promising method that needs some more research. It is interesting since it combines cueing techniques, cognitive movement strategies, balance exercises, and physical activity. The focus is on enjoying moving and not on the mobility limitation which might attract more patients with Parkinson’s disease than standard exercises.
Motor learning
If executed and practiced as a strategy to train improvements in the movement of the body. It takes the form of dual-task training and cued functional compensatory strategy training and uses external cues, attention, and self-instruction. Examples include:
- Visual cueing
- A focus point to initiate gait and step over; strips of tape on the floor to start or continue walking through areas that cause freezing or slowing.
- Auditory cueing
- In that, counting 1-2-3 to commence walking, stepping to the specific music or the beat of a metronome at a specified cadence to continue the rhythm of a walk.
- Attention
- Think about taking a wide step, making a wider arc turn. This is applicable in case of correcting a bad habit such as walking with hip hiking or a stiff hip.
- Proprioceptive cueing
- In that, rocking from side to side ready to start a step, taking one step behind or backward as a cue ready to then walk forwards.





8 Comments