Tillaux fracture
Table of Contents
Introduction
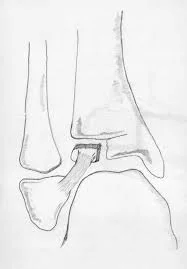
Tillaux fractures are traumatizing ankle injuries in children caused by a Salter-Harris III fracture of the anterolateral distal portion of the tibia the epiphysis.
The irregular closure of the distal tibial physeal plate causes the mechanism of injury in a Tillaux fracture, resulting in the classic Tillaux fracture pattern in adolescent patients. This is a Salter-Harris type III fracture, which is an intraarticular fracture. The distal tibial physis participates, and the distal tibial bony epiphysis is involved in the intraarticular portion of the fracture pattern.
The fracture is named after French physician Paul Jules Tillaux, who practised medicine and surgery in Paris. He was the first physician to describe the Salter-Harris type III distal tibia fracture in 1892. The fracture was described as a single injury. Still, connections with a Salter-Harris I or II distal fibula fracture or an ipsilateral distal tibial shaft fracture are possible.
Mechanism of injury
An abduction-external rotation force frequently causes the anterior tibiofibular ligament to avulse the distal tibial epiphysis’s anterolateral corner, resulting in a Salter-Harris Type III fracture. it was facilitated by the avulsion of the anterior inferior tibiofibular ligament.
The absence of a coronal plane fracture in the posterior distal tibial metaphysis distinguishes this fracture from a triplane fracture.
Epidemiology
Incidence
3-5% of paediatric ankle fractures are caused by
Demographics
more common in females
seen in children 12-14 years old nearing skeletal maturity
Due to the pattern of progression of physeal closure, this usually occurs within one year of complete distal tibia physeal closure.
older than the age group for triplane fractures
Causes of tillaux fracture
Tillaux fractures are most commonly caused by high-energy trauma, such as a car or motorcycle accident, a fall from a great height, or a skiing accident, due to rotational or axial-loading forces to the tibia bone.
Meanwhile, other factors that contribute to this type of fracture include:
- During car accidents, there is a lot of pressure.
- Side-to-side ankle twist
- Side-to-side ankle rotation
- Ankle rolling in or out
- Hyper-flexion
- Hyper-Extention
- Tripping
- Falling from a great height
- Jumping from a great height
Two factors increase a person’s risk of fractures as they age:
- Weaker bones
- Falling is more likely.
Stress fractures are common causes of fractures caused by repeated stresses and strains. Children, who lead more physically active lives than adults, are more prone to fractures.
Fractures are more likely in people with underlying diseases such as osteoporosis, infection, or a tumour affecting their bones.
This type of fracture is known as a pathological fracture, as mentioned in previous chapters.
Stress fractures, which occur due to repeated stresses and strains, are also common causes of fractures in professional athletes.
Risk factors
Several risk factors can predispose a patient to a Tillaux fracture, including:
- High-adrenaline contact sports
- Age (elderly adults are more susceptible to such fractures)
- Osteoporosis (low bone density)
- A direct hit
- Accidents on the road or in traffic
- Falling
- An ankle injury sustained directly
- Participating in any rough or high-impact sport
- Street brawls, gunshot wounds, and domestic violence can all result in the Tillaux fracture.
- Accidents on the highway.
Diagnosis of tillaux fracture
Physical examination
Physical examination will typically reveal pain and swelling in the anterior lateral part of the ankle. This symptom resembles an ankle sprain or anterior talofibular ligament injury. Because of this, the injury is frequently misdiagnosed as an ankle sprain.
However, the fact that the physis may still be open in an adolescent and that it is weaker than the ligamentous anterior talofibular ligament should prompt the examiner to order additional objective x-rays of the ankle to rule out any potential bony injury.
A closer examination may reveal a joint effusion. This represents bleeding into the joint from the fracture’s intraarticular extension and should alert the examiner to the need for additional objective evaluation of the injury.
Radiographs
Anteroposterior, lateral, and Mortise views of radiographs. Radiographs of a Tillaux fracture will show the classic pattern of anterior lateral physeal separation and fracture extension through the bony epiphysis into the ankle joint. It is a Salter-Harris type III anterolateral distal tibial epiphysis fracture.
CT scan
This is the preferred imaging modality for determining the degree of displacement of a Tillaux fracture. In evaluating fractures with as little as 2 mm displacement, CT is more sensitive than plain radiographs.
Treatment of tillaux fracture
The amount of displacement determines how a Tillaux fracture is treated. Regardless of which treatment option is chosen, the primary goal is anatomic reduction. With as little as 2 mm of displacement, the fracture can be managed non-operatively with closed reduction and immobilization in a cast. Foot internal rotation is typically used to achieve closed reduction.
Alternatively, dorsiflexion and pronation of the foot can be attempted, followed by an internal rotation. This is usually accompanied by the use of a short leg cast with the ankle slightly inverted to aid in the maintenance of the fracture reduction. Casting is typically for four weeks without weight bearing, followed by two weeks in a walker boot to allow ankle range of motion.
Fractures that are displaced more than 2 mm with disruption of the distal tibial articular congruity should be treated surgically as follows:
Closed Reduction and Percutaneous Pinning (CRPP)
As previously stated, the reduction can be achieved by using a K-wire in the fracture fragment as a joystick. The reduction quality can be assessed intraoperatively using fluoroscopy or an arthrogram. If the reduction is satisfactory, the fracture is stabilized with K-wires or cannulated screws placed parallel to the articular surface across the epiphysis.
Open Reduction and Internal Fixation (ORIF)
An anterolateral approach is used for optimal reduction by allowing direct visualization of the articular surface. Internal rotation is used to reduce the fracture, which is then held in place with trans epiphyseal K wires or a periarticular clamp. K wires or cannulated screws are used to secure the epiphysis.
Tillaux fractures occur in children who are nearing skeletal maturity, so crossing the physis has little effect on remaining growth. Fracture fixation is typically supplemented with a cast or splint for four weeks, followed by a walker boot for an additional two weeks to allow for ankle range of motion exercises.
The anterolateral portal is typically used for arthroscopically assisted reduction and fixation. It enables direct anatomic fracture reduction with minimal intervention.
Rehabilitation
Individualized immobilization and rehabilitation strategies are required for complex Tillaux fractures. Because most multi-fragmentary Tillaux fractures are caused by high-energy injuries, prolonged wrist immobilization and soft-tissue rest may be beneficial but have not been shown to affect clinical outcomes.
The ankle is typically immobilized in a splint for 6 weeks following surgery. After radiographs show consolidation of the fracture, full weight bearing begins about 3 months after surgery.
Ankle stiffness of varying degrees is unavoidable and can be caused by poor pain control, a lack of effort in controlled mobilization, oedema, concomitant ipsilateral lower extremity fractures, or peripheral nerve injuries. Preventing finger stiffness requires early stretching and mobilization of the hand’s intrinsic and extrinsic tendons.
Compression gloves, digital massage, and active and passive ankle ROM can help to control oedema. A home exercise programme or outpatient occupational therapy is initiated immediately following surgery to maintain a full ankle range of motion and limit the development of intrinsic muscle tightness.
Complications of tillaux fracture
A persistent articular surface step, like any intra-articular fracture, predisposes the joint to premature secondary osteoarthritis.
Ankle arthritis is caused by a traumatic injury.
Pain and stiffness in the ankle.
Tillaux fractures occur near the end of physeal growth, so premature growth arrest is uncommon.
Summary
Tillaux fractures are ankle injuries in children caused by a Salter-Harris III fracture of the anterolateral distal portion of the tibia. The mechanism of injury in a Tillaux fracture is an abduction-external rotation force, resulting in the classic Tillaux fracture pattern. The fracture is named after French physician Paul Jules Tillaux, who was the first to describe the fracture in 1892. It is more common in females and seen in children 12-14 years old nearing skeletal maturity. Causes include high-energy trauma, high-adrenaline contact sports, age, osteoporosis, direct hits, road or traffic accidents, falling, and participating in rough or high-impact sports.
Diagnosis involves physical examination, radiographs, and CT scans. Treatment focuses on anatomic reduction, with closed reduction and immobilization in a cast or a walker boot for four weeks. For fractures displaced more than 2 mm, surgical treatment includes closed reduction and percutaneous pinning (CRPP), open reduction and internal fixation (ORIF), and anterolateral portal. Rehabilitation strategies include individual immobilization and rehabilitation strategies. Tillaux fractures, a persistent articular surface step, can lead to premature secondary osteoarthritis, ankle arthritis, and pain, but premature growth arrest is uncommon due to their location near physeal growth.
FAQs
Tillaux fractures are intraarticular fractures of the distal tibia’s physis and epiphysis that occur in children and adolescents. Salter-Harris type III fractures are what these are.
The fracture is frequently caused by an abduction-external rotation mechanism. The inferior anteroinferior tibiofibular ligament avulses the anterolateral corner of the distal tibial epiphysis using this mechanism.
The amount of displacement determines how a Tillaux fracture is treated. Regardless of which treatment option is chosen, the primary goal is anatomic reduction. With as little as 2 mm of displacement, the fracture can be managed non-operatively with closed reduction and immobilization in a cast.
A forced external rotation of the foot in supination or a medial rotation of the leg on the fixed foot, usually between the ages of 11 and 15 years, is usually responsible for an avulsion injury to the anterolateral epiphysis, known as a Tillaux fracture.
References:
- Tillaux fracture – wikidoc. (n.d.). https://www.wikidoc.org/index.php/Tillaux_fracture
- Ahn, L. (n.d.). Tillaux Fractures – Pediatrics – Orthobullets. https://www.orthobullets.com/pediatrics/4028/tillaux-fractures
- Hacking, C., & Gaillard, F. (2008, May 2). Tillaux fracture. Radiopaedia.org. https://doi.org/10.53347/rid-2185
- Habusta, S. F. (2023, April 22). Tillaux Fracture. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK482332/
- Tillaux fracture. (2022, June 7). Wikipedia. https://en.wikipedia.org/wiki/Tillaux_fracture