Pathological Fracture
Table of Contents
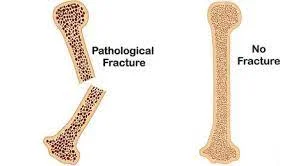
What is a Pathological Fracture?
When a bone breaks in an area that has already been weakened by another disease, this is known as a pathologic fracture. When a person’s bone is weakened due to an underlying medical condition, he or she is more prone to fracture. Tumours, infection, and certain inherited bone disorders are all causes of weakened bone. These, however, are only a few of the causes; dozens of other diseases and conditions can result in a pathologic fracture.
When a bone fracture occurs, there may have been an injury, such as a fall, that would not normally cause a fracture but did in the weakened bone. When the bone is severely weakened, a fracture can occur without any obvious event. Walking or rising from a chair can cause a fracture if the bone is severely weakened.
Bone fractures come in a variety of shapes and sizes. Pathologic fractures are so named because the bone was already weakened before the injury occurred. Pathologic fractures can be obvious at times, but it is not always obvious that there was a problem before the injury.
Pathologic fractures occur as a result of weakened bone caused by primary malignant lesions, benign lesions, metastasis, or underlying metabolic abnormalities, with the common factor being altered skeletal biomechanics as a result of pathologic bone.
Causes of Pathological Fracture
Pathologic fractures in children and adolescents can be caused by a wide range of disorders, including metabolic, endocrine, neoplastic, infectious, immunologic, and genetic skeletal dysplasia.
Osteoporosis
Osteoporosis is a disease that weakens your bones, increasing their susceptibility to fracture.
Osteoporosis symptoms usually appear in the later stages of the disease, when the bones are weak and brittle. Among the symptoms are:
- back pain
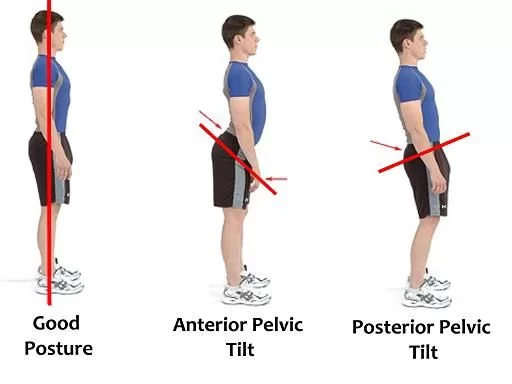
- hunched posture
- gradual height loss
- fractures, most frequently in the hip, spine, or wrist
Osteoporosis is extremely common. It disproportionately affects women. Because of osteoporosis, 50% of women and up to 25% of men will break a bone in their lifetime. It is also more common in the elderly
Cancer
Cancer is a disease explained by abnormal cell growth. It has the potential to affect almost every part of your body. Many cancers can invade and weaken bones, causing them to break.
Cancer symptoms vary greatly depending on the type and stage, but general symptoms include:
- a hard lump(s) beneath the skin
- swelling and discomfort
- lymph nodes swollen
- Fever, night sweats, and chills
- unexpected for weight loss
- variations in appetite
- abnormalities in bowel function
- changes in the appearance of the skin
- fatigue
- non-healing injuries
- a persistent cough or cold
Osteomalacia
Osteomalacia is a bone-softening condition. It usually occurs due to a lack of vitamin D, and it helps your body’s absorption of calcium. Calcium is necessary for bone health, so when you don’t get enough of it, your bones start to degenerate. Because of the outcome, they are more easily broken and fractured.
Osteomalacia symptoms include:
- weakness in the muscles
- pain, usually in the hips
- fractures
- Changing your diet or taking supplements can usually treat osteomalacia.
Osteomyelitis
Osteomyelitis is a bone infection. A bacterial or fungal infection spreads to nearby bones and causes it. Osteomyelitis can result in a pathologic fracture in rare cases.
Osteomyelitis symptoms include:
- Fever, chills, tiredness,
- irritability discomfort,
- inflammation, or heat at the site of infection
- stiffness in the region of damage
Other conditions
- Cerebral palsy
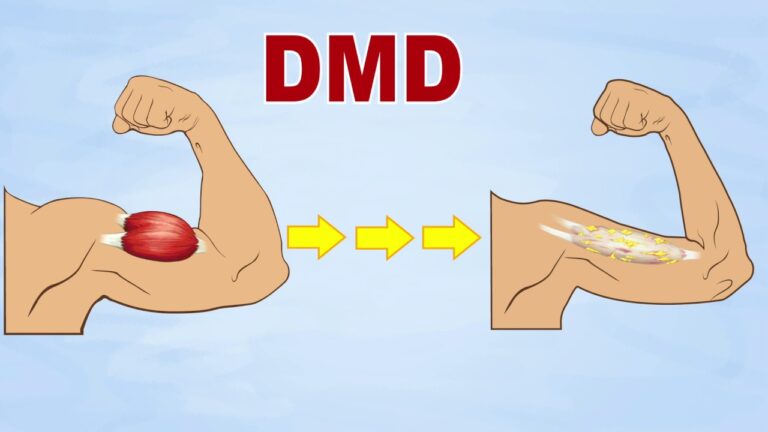
- Dystrophy of the musculoskeletal system
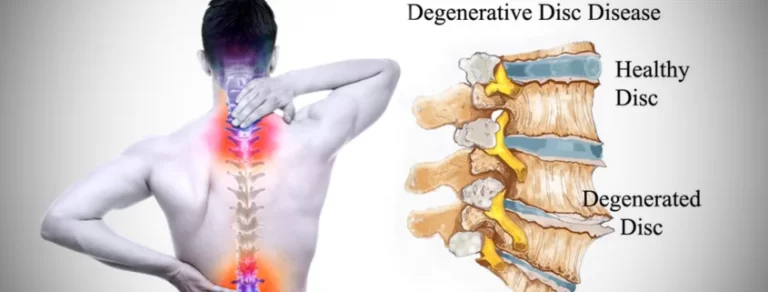
- Atrophy of the Spinal Muscles
- Spina bifida is a birth defect.
- The Down syndrome
- Endocrine disorders such as hyperthyroidism and hyperparathyroidism
- Cystic fibrosis (CF)
- Renal dysfunction
- cholestasis of the liver
- Gluten intolerance
- IBD (Irritable Bowel Disease)
- Arthritis rheumatoid
- Other uncommon genetic conditions
- Tumours and cysts that are not cancerous
- Paget’s disease of bone is a rare condition that results in abnormal bone structure.
- Imperfect osteogenesis
Symptoms of Pathological Fracture
Pathologic fractures are not always related to symptoms. They present the same symptoms as an injury-related fracture. These are some examples:
- pain varying from mild to severe near the broken bone
- bruising, tenderness, and swelling in nearby areas of the broken bone
- numbness, tingling, or weakness in nearby areas of the broken bone
In some cases, identifying between symptoms of a pathologic fracture and those of the underlying condition affecting your bones can be difficult.
Risk factors
While it is possible to strengthen your bones when you are young, it is impossible to predict whether you will suffer a pathologic fracture. The following factors raise your risk:
- You are not getting enough nutrients in your diet, specifically vitamin D, calcium, and protein.
- Being underweight or obese
- Backache or bone pain
- Physical inactivity and immobility
- There is insufficient time spent in the sun to absorb vitamin D.
- Disruptions in sex or growth hormones
- Inflammatory conditions are becoming more prevalent.
- Your family has a history of pathologic fractures.
Diagnosis
The doctor will take a thorough medical history and conduct a thorough physical examination.
If the doctor suspects a pathologic fracture, he or she may order the following diagnostic procedures:
X-ray (also known as plain films): a test that produces images of bones using invisible electromagnetic energy beams (X-rays). Soft tissue structures such as the spinal cord, spinal nerves, the disc, and ligaments are typically not visible on X-rays, nor are they visible in the majority of tumours, vascular malformations, or cysts. X-rays assess the bone anatomy as well as the curvature and alignment of the vertebral column.
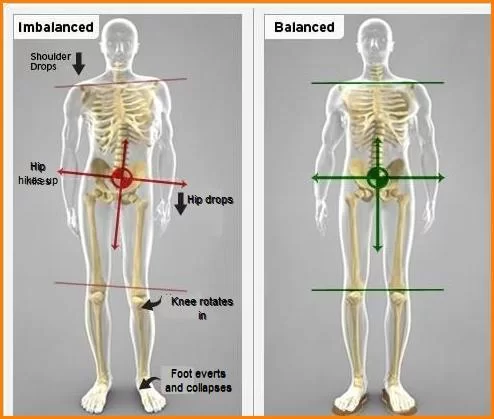
X-rays can detect spinal dislocation or slippage (also known as spondylolisthesis), kyphosis, scoliosis, and local and overall spine balance. Plain film X-rays can also detect specific bony abnormalities such as bone spurs, disc space narrowing, vertebral body fracture, collapse, or erosion. Dynamic X-rays, also known as flexion/extension X-rays (X-rays that show the spine in motion), can be obtained to determine whether there is any abnormal or excessive movement or instability in the spine at the affected levels.
Magnetic resonance imaging (MRI) is a diagnostic procedure that produces detailed images of organs and structures within the body using a combination of large magnets, radio frequencies, and a computer.
Computed tomography scan (CT scan): a diagnostic imaging procedure that produces detailed images of the body using X-rays and computer technology. A CT scan produces high-resolution images of any part of the body, including the bones, muscles, fat, and organs. CT scans give more information than standard X-rays.
Nuclear bone scan: a diagnostic procedure that involves injecting a radioactive substance into the body to measure bone activity. (The amount of radiation is small–less than half of one CT scan.) This scan aids in the identification of broken bones.
Certain laboratory tests to assess calcium levels may be performed, as well as a biopsy (tissue examination) to determine the exact cause of the fracture.
Treatment of Pathological Fracture
The treatment of a pathologic fracture depends on the underlying condition. Many diseases weaken your bones without impairing their ability to heal. In these cases, a cast or splint will most likely be sufficient. Depending on the location of the fracture, a pin, plate, or screw may be required for maintaining the bone in place while it heals.
While you heal, you should rest and avoid activities that require you to use the parts of your body affected by the fracture. Depending on the affected body part, recovery can take anywhere from a few weeks to several months.
If you have a condition that makes it difficult for your bones to heal, you may require additional treatment, such as surgery. Depending on your underlying condition, your doctor may decide that treating your symptoms is the best option.
You may need to wear a cast or splint to treat the fracture. Sometimes surgery is required to insert plates, pins, or screws to keep the bone in place. You may need to rest for a while and avoid doing activities that put a strain on the fractured area.
If the fracture is pathological, your doctor will want to treat the underlying cause of the bone break to help prevent it from happening again. The cause of the weakened bone heavily influences the treatment of a pathologic fracture. Some causes of pathologic fractures may weaken the bone but not change its healing properties. Some causes of a pathologic fracture, on the other hand, may prevent normal bone healing. As a result, some pathologic fractures require standard treatment, while others may necessitate highly specialized care.
Prevention
Pathologic fractures cannot always be prevented. If you have a bone-weakening condition, talk to your doctor about ways to reduce your risk of a pathologic fracture.
Depending on your current state of health, your doctor may advise you to:
- Exercise regularly to keep your muscles strong and your bone health in good shape.
- Get enough calcium and vitamin D.
- Receive treatment for the underlying condition as soon as necessary.
- Prosthetics or assistive devices, such as supportive shoes, a cane, or a walker, should be used.
- High-intensity activities should be avoided.
Summary
Pathologic fractures occur when a bone breaks in an area that has already been weakened by another disease, such as tumours, infections, or inherited bone disorders. These fractures can occur due to weakened bone caused by primary malignant lesions, benign lesions, metastasis, or underlying metabolic abnormalities. Causes include osteoporosis, cancer, osteomalacia, osteomyelitis, and other conditions.
Symptoms of pathologic fractures include pain, bruising, tenderness, swelling, and numbness. Risk factors include not getting enough nutrients in your diet, being underweight or obese, backache or bone pain, physical inactivity, and immobility, insufficient time spent in the sun to absorb vitamin D, disruptions in sex or growth hormones, and inflammatory conditions.
Diagnosis of pathologic fractures involves a thorough medical history and physical examination. Diagnostic procedures may include X-rays, magnetic resonance imaging (MRI), computed tomography scan (CT scan), nuclear bone scan, and laboratory tests to assess calcium levels and determine the exact cause of the fracture.
Pathologic fractures can be treated with casts, splints, or surgery depending on the underlying condition. The recovery period may extend range from weeks to months. Treatment depends on the underlying cause, which can affect healing properties. Preventative measures include regular exercise, adequate calcium and vitamin D intake, timely treatment for the underlying condition, use of prosthetics or assistive devices, and avoiding high-intensity activities.
FAQs
Being underweight or obese. You have bone or back pain. Physical inactivity and immobility. There isn’t enough time in the sun to absorb vitamin D.
Patients with breast (50%), kidney, lung, or thyroid cancer account for more than 80% of pathologic fractures. Approximately 10% to 30% of pathologic fractures in long bones caused by a metastatic lesion require surgical intervention.
MRI is useful for distinguishing pathologic from stress fractures, especially when radiographic findings are inconclusive. Pathologic fractures, in particular, have well-defined T1 marrow alterations, endosteal scalloping, and adjacent soft-tissue abnormalities.
Most patients with a completed or impending pathologic fracture of a long bone will require surgical bone fixation
X-rays can help doctors diagnose bone fractures. They may also employ CT (computed tomography) and MRI (magnetic resonance imaging) scans.
Osteoporosis has also become a widespread cause of pathologic fractures. Osteoporosis is a condition that causes weak and brittle bones in older women.
References
- Cluett, J. (2022, July 22). What Is a Pathologic Fracture? Verywell Health. https://www.verywellhealth.com/pathologic-fracture-2548526
- Vandergriendt, C. (2018, September 18). Pathological Fracture. Healthline. https://www.healthline.com/health/pathologic-fracture#causes
- What Is a Pathologic Fracture? (2021, April 18). WebMD. https://www.webmd.com/a-to-z-guides/what-is-a-pathologic-fracture
- Pathologic Fracture. (2021, July 21). Columbia Neurosurgery in New York City. https://www.neurosurgery.columbia.edu/patient-care/conditions/pathologic-fracture
- Pathological Fracture Treatment Detroit | Broken Bone Treatment Bloomfield Hills, Mount Clemens, MI. (n.d.). https://www.sarcomadoc.com/pathological-fractures-orthopaedic-oncologist-detroit-mi.html
- Pathologic fracture. (2021, December 12). Wikipedia. https://en.wikipedia.org/wiki/Pathologic_fracture


One Comment