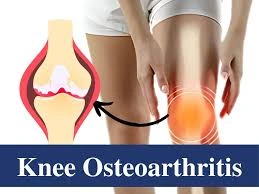
Knee Osteoarthritis
Knee osteoarthritis is a degenerative joint condition where the protective cartilage in the knee gradually wears down, leading to pain, stiffness, and reduced mobility. It is one of the most common causes of knee pain, especially in older adults, and often develops due to aging, overuse, or previous injuries.
Your knee’s cartilage gradually deteriorates when you have osteoarthritis, a degenerative disease. The most prevalent kind of arthritis that affects the knee joint is this one. Therapy can assist in reducing the symptoms of OA, even though it is a long-term, advancing condition. If it gets really bad, your doctor may suggest knee replacement surgery.
Table of Contents
What is Knee Osteoarthritis?
- Your knee joint develops osteoarthritis when the cartilage becomes damaged and the bones start to rub against one another. Your knee becomes rigid as a result of the pain and swelling caused by this contact.
- Constant strain and damage lead to osteoarthritis, often called degenerative joint disease.
- Osteoarthritis (OA) is a long-lasting, degenerative condition affecting the knee that currently has no cure. Numerous therapies are available to reduce its progression and reduce your symptoms, and altering your lifestyle can be beneficial. However, it can eventually result in impairment and does have a tendency to get worse over time.
- Your doctor will keep an eye on your arthritis as it develops. Surgery may become necessary when it begins to significantly affect your life.
Causes of Knee Osteoarthritis
- Age
- Weight
- Heredity
- Gender
- Repetitive stress injuries
- Athletics
Age: As you age, your cartilage becomes damaged because your cells are less able to repair themselves. Previously, doctors believed that nearly everyone would eventually acquire OA, but they have now discovered that this is false.
Weight: All of your weight-bearing joints, especially your knees, are exposed to greater strain when you carry weight. For each pound of weight gained, there is an increase of four pounds of pressure on the knees.
Heredity: Family members may have OA. Some people with connective tissue conditions, such as Ehlers-Danlos, are hypermobile and have collagen vascular diseases. Those patients get arthritis sooner than others. Hereditary anomalies in the form of the bones around the knee joint might be an additional risk.
Repetitive stress injuries: People who frequently do the same tasks—whether for job or personal hobbies—put continuous strain on their joints. As a result, osteoarthritis of the knee may develop if you kneel, squat, or lift large weights regularly.
Athletics: Long-distance runners and other athletes who play sports that strain their knees may be more susceptible to osteoarthritis of the knee. Their participation frequency and other risk variables, such as past knee problems, will determine this. Additionally, female-born athletes may be at greater risk. It is notable that consistent moderate exercise can reduce the risk of osteoarthritis and strengthen the muscles around the joints. Osteoarthritis can really result from weak knee muscles.
Secondary Causes Of Knee Osteoarthritis
- Rheumatoid arthritis
- Infectious (septic) arthritis
- Psoriatic arthritis
- Previous knee injuries
- Knee surgery
- Malformation of the leg
- Scoliosis
Illnesses such as rickets, hemochromatosis, Wilson’s disease, hemophilia, Paget’s disease, and Sickle cell disease.
Symptoms of Knee Osteoarthritis
The signs that are most frequently linked to osteoarthritis in the knee include the following:
- Knee pain, particularly pain that is bone-on-bone.
- knee pain, particularly after spending a lot of time sitting or lying down.
- knee swelling.
- Having the feeling that your knee is unstable or locked in.
- A sound of cracking or grinding when the knee is moved.
Stages Of Knee Osteoarthritis
Osteoarthritis in your knee is a degenerative disorder that advances gradually, even though there are no clear stages. (This is not the same as other kinds of knee arthritis.) Your doctor may describe the severity of your disease using stages or levels. Understanding the progression of osteoarthritis may assist you in interpreting your symptoms and anticipating what comes next.
Stages consist of:
- Phase 1 (Minor): Your knee joint’s cartilage has some wear and tear. It is likely that you have not yet experienced any kind of pain.
- Phase 2 (Slight): During this mild stage, you might experience some pain and stiffness; however, there is still sufficient cartilage to keep the bones from rubbing against each other.
- Phase 3 (Moderate): You have substantially less cartilage if you are in this stage. Particularly while walking, sitting, kneeling, and sprinting, this makes the pain worse. Additionally, you may experience increased joint stiffness or trouble moving, particularly after extended periods of inactivity.
- Phase 4 (Severe): Your knee’s bones grind against each other as you move, and the cartilage is almost completely gone because of severe osteoarthritis. Your knee pains, feels rigid, and may have limited mobility. You may now think about having knee replacement surgery.
Diagnosis
A physical examination will be conducted by your doctor prior to diagnosing osteoarthritis in your knee. They might look at:
- Your knee’s appearance. Is there swelling or discoloration?
- where the pain is. When you indicate the area of pain, is it a specific spot or more widespread over the knee?
- Symptoms indicative of damage
- How well were you able to move your knee?
- When they touch your knee, does it seem loose or unsteady?
- how you walk. What does your step look like when you walk?
MRIs are performed when X-rays fail to clearly identify the cause of your joint pain or when they indicate that additional joint tissue types may be damaged. Blood tests may also be requested by your doctor to rule out other medical conditions, such as rheumatoid arthritis, as the source of your pain. Lastly, if necessary, your doctor may want to extract fluid from your knee for analysis.
Treatment For Knee Osteoarthritis
Treatment for osteoarthritis in the knee can involve surgery, non-invasive therapies, and changes to one’s lifestyle. Medical professionals usually recommend nonsurgical therapies for knee OA before suggesting surgery.
- Lifestyle and at-home treatments
- Weight loss
- Exercise
- Pain relievers and anti-inflammatory drugs
- Using devices such as braces
- Physical and occupational therapy
- Injections
Lifestyle and at-home treatments: Before beginning any new activity, including exercise, it’s important to consult your doctor. There are a few things you can do at home to assist in managing OA pain and slow down its progression. To prevent accidentally causing further harm, you must cooperate.
Weight loss: If necessary, losing even a little amount of weight can help reduce osteoarthritis-related knee pain.
Pain relievers and anti-inflammatory drugs: You can control your pain with over-the-counter (OTC) medications like naproxen sodium, ibuprofen, or acetaminophen, but don’t take OTC drugs for longer than ten days without consulting your doctor. Prolonged use of these can increase the likelihood of negative effects. In the event that over-the-counter drugs prove ineffective, your physician may prescribe greater dosages or other medications to help relieve the pain.
Using devices such as braces: Two kinds of braces exist:
Braces called “unloaders” remove weight from the knee’s arthritis-affected side.
Braces that provide “support” for the whole knee.
Physical and occupational therapy: Physical therapy or occupational therapy may be helpful if you are experiencing difficulties with everyday tasks. You may learn how to strengthen your muscles and increase the flexibility of your joints from physical therapists. Occupational therapists can teach you how to conduct everyday tasks like cleaning or give you the tools you need to complete them more comfortably.
Injections: The first line of therapy is injections. Because noninvasive therapies are less likely to produce problems, doctors favor them.
Among the injections are:
Corticosteroid: Strong anti-inflammatory medications like steroids can reduce joint inflammation.
Apply hyaluronic acid knee gel to the knee: Your body already contains hyaluronic acid, a natural lubricant. Additional gel injections could help to lubricate your knee and reduce the friction between the bones.
Blocking of the genicular nerve: This therapy is intended to manage pain temporarily. To relieve your knee pain, your doctor would provide a local anesthetic and steroids around certain nerves.
Exercises For Knee Osteoarthritis
- Straight leg raise
- Quad set
- Lying quad stretch
- Side-lying leg raise
- Bridging
- Step-ups
- Sit-to-stand
- Mini squats at a countertop
- Tandem balance
- Single-leg balance
- Calf stretch with towel, strap, or resistance band
- Seated hamstring stretch
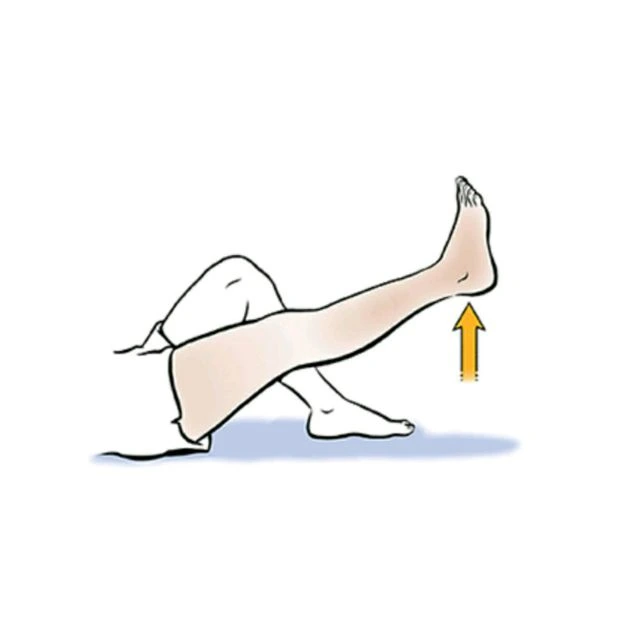
- Lie on your back on a yoga mat or the floor, making sure that your arms are positioned alongside your body and your legs are fully extended in front of you.
- Keeping your knee straight, raise one leg approximately a foot off the ground while activating your quadriceps.
- Repeat this process for two sets of fifteen repetitions for each leg.
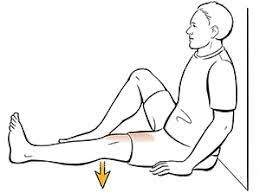
Quad set:
- Relax the back of your bent leg on the towel while you engage your thigh muscles.
- Keep your back flat against the floor while carrying out this exercise.
- Keep your back flat against the floor for the entire duration of this exercise.
- Perform these steps for two sets of fifteen reps on each leg.
Side-lying leg raise:
- Position your upper arm in front and utilize your hand to help you stay balanced.
- For two to three seconds, raise your upper leg to hip height while maintaining a straight posture. Lower your leg slowly after that.
- Perform these steps for two sets of fifteen repetitions on each leg.

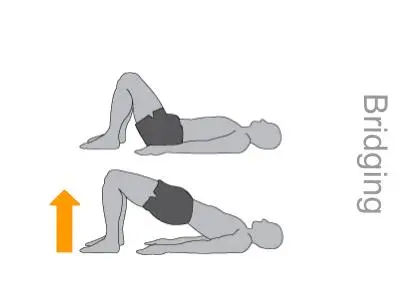
Bridging:
- First, lie flat on your back.
- Tighten your glutes, lift them off the surface or bed, and maintain a straight back by engaging your lower abdomen or core muscles. Maintain this posture for five seconds.
- Complete this exercise in two groups of 15 repetitions.
Step-ups:
- Start by standing upright in front of a yoga block or at the foot of a set of steps.
- Hold onto a secure object for stability, such as a railing, bend your knee, raise one foot, and place it on the step or block using that foot.
- Taking the opposite stairs will bring you back to the earth.
- Do one or two sets of ten repetitions of this procedure.
- This can also be done laterally (sideways) by switching postures. In that case, ensure you stay balanced during the exercise, keeping your hips even and your pelvis aligned parallel to the floor.

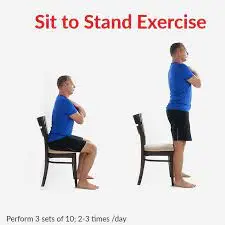
Sit-to-stand:
- To begin, take a chair so that your head is looking forward and your back is straight.
- Fold your arms over your chest and lean your upper body forward without raising your eyes.
- Straighten up by pressing into your feet, then slowly sit back down and do it again.
- It’s essential to keep your balance and ensure that your weight is evenly distributed between both legs. Avoid locking your legs when standing.
- Do this three times for five repetitions.
- If necessary, you can stand with additional support by gripping the back of a small tabletop or another chair.
Mini squats at a countertop:
- Start standing up straight, placing your hands on a tabletop and your feet shoulder-width apart.
- Carefully lower yourself into a mild squat by bending your knees a little.
- After a few seconds of holding this squat position, push onto your feet to go back to your standing, upright position.
- When you need assistance balancing, use the counter, but maintain your heels on the floor. Your knees should not fall inward or bend forward past your toes.
- Do this three times for five repetitions.
Tandem balance:
- First, stand upright and let your arms rest by your sides.
- Align your feet in a straight line, placing one foot directly in front of the other.
- Keep your back straight, avoid pulling your arms away from your body, and keep your balance in this position.
- As long as you can, maintain this posture, switching between your left and right foot as the leg in front, and aiming for two or three repetitions of 30-second holds.

Single-leg balance:
- Position yourself standing straight with your feet close together and your arms hanging by your sides.
- Balance on the opposing leg while raising one foot off the ground. When in this position, attempt to maintain your equilibrium.
- Keep your arms near your body and maintain a stable stance. To improve balance, stretch your arms out to the sides or grasp a railing or countertop with one hand.
- On each foot, aim for two to three repetitions of 15 seconds.

Calf stretch with towel, strap, or resistance band:
- Begin by sitting on the floor, bed, or bench, one foot extended forward.
- Bend the opposite knee so that your thigh is parallel to the ground and your foot extends outward at a right angle to your body.
- Put a resistance band, towel, or strap around your bent foot, then gently bring it closer to you until your calf starts to stretch.
- When performing this exercise, keep your knee straight.
- Switch legs with each hold, performing three to five sets of 10 to 15 seconds per side.

Seated hamstring stretch:
- Begin by sitting erect on the edge of a solid, raised surface (such as a bed or bench), one foot flat on the ground and one leg straight on the surface.
- Lean forward with your hips hinging gently until the back of your leg feels stretched, then maintain that posture.
- Bend forward without rounding your back.
- For three to five sets of ten to fifteen seconds each, switch legs between holds.

Knee Osteoarthritis Video
Prevention
Since knee osteoarthritis typically has no one cause, it is impossible to completely avoid. However, to lessen your risk, try to reduce the pressure and stress on your knee joint. As an illustration:
- If you work a job that strains your knees, think about methods to change the way you do it.
- Look for soft surfaces rather than pavement if you run or jog.
- Include low-impact activities like cycling or swimming in your training routine to mix things up.
- Even a 10% weight loss can greatly lower your chances of developing knee OA if you are overweight.
Summary
Knee osteoarthritis is quite frequent, but it’s not a guarantee as you age. It’s a wear-and-tear kind of arthritis that affects your knees and other supporting joints. If you need to, you can try to slow down its progression by exercising to strengthen the muscles surrounding your knee and decreasing weight. Talk to your doctor if you’re experiencing knee pain from osteoarthritis, though, since there may be some medication and surgery alternatives that might help.
FAQ’s
From moderate to severe, the four phases of osteoarthritis in the knee are often categorized: Stage 1 is characterized by mild wear and tear and frequently no symptoms; Stage 2 is characterized by mild symptoms, including minor cartilage damage and early bone spurs; Stage 3 is characterized by moderate cartilage damage, significant stiffness and pain, and visible bone spurs on X-rays; and Stage 4 is characterized by severe cartilage damage, nearly no cartilage remaining, bone grinding, and ongoing pain.
Knee osteoarthritis (OA) is best treated with a combination of techniques rather than a single solution that focuses on reducing pain, enhancing function, and preventing additional damage. Weight loss (if relevant), physical therapy and exercise to increase strength and mobility, and activity management to prevent high-impact motions are all important components. Injections of corticosteroids or hyaluronic acid are among the pain management options, as are over-the-counter and prescription acetaminophen and NSAIDs (including topical gels). In more severe situations, when medicinal treatments are not enough, knee replacement surgery may be considered.
You should stay away from the following five activities if you have osteoarthritis in your knees to lessen the chance of joint damage and pain:
Walking over rough ground.
High-impact workouts.
Repeated movements.
lifting large, heavy objects.
Wearing heels.
As a low-impact activity that increases joint flexibility, strengthens supporting muscles, and helps in maintaining a healthy weight, walking can benefit people with osteoarthritis in their knees by easing pain and stiffness. In addition to selecting suitable, supportive footwear and flat surfaces to reduce joint stress, it is advised to begin with shorter walks and progressively increase the duration and frequency.
References:
- Knee osteoarthritis. (2025, June 26). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21750-osteoarthritis-knee
- Durning, M. V., RN. (2025, June 17). What is knee osteoarthritis? WebMD. https://www.webmd.com/osteoarthritis/ostearthritis-of-the-knee-degenerative-arthritis-of-the-knee
- Knee osteoarthritis: Symptoms & Causes | Brigham and Women’s Hospital. (n.d.-b). https://www.brighamandwomens.org/orthopaedic-surgery/osteoarthritis-of-the-knee
- Clinic, C. (2025, January 22). Try these exercises if you’ve got knee arthritis. Cleveland Clinic. https://health.clevelandclinic.org/knee-arthritis-exercises




One Comment