Cervical Degenerative Disc Disease
Table of Contents
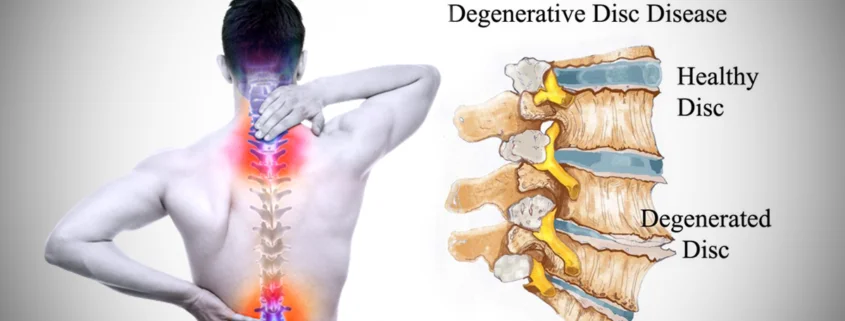
What is Cervical Degenerative Disc Disease?
- It is the most common cause of neck pain and radiating arm pain. It develops when one or more discs of the cervical spine start to break down due to degeneration or wear and tear.
- Degeneration of the disc is commonly seen in the moving sections of the spine like the cervical and lumbar levels is a natural process of “aging.” When this “aging” process happens more rapidly, it is considered “degeneration.” The dehydration or desiccation of the disc material reduces the flexibility, mobility, and typically the height of the disc. In some cases, the degeneration causes compression between the vertebra causing pain at that level.
- It is commonly known as cervical spondylosis, or spondyloarthritis, and begins as a degenerative process in the central intervertebral (body) joints. Subsequent time, it affects the posterior intervertebral (apophyseal) joints.
- Pain and stiffness in the neck are the most common symptoms of cervical degenerative disc disease. Often, there may be referred symptoms to the neck, shoulder, arms, and hands.
- There occurs degeneration of the disc, with bone reaction at the periphery that results in osteophytes and wear and tear of the articular cartilage. Osteophytes may produce pressure on the cervical nerve root at the intervertebral foramina, leading to compression symptoms. Osteophytes may encroach upon the spinal cord and cause pressure over the spinal cord in rare cases. The symptoms may vary with the site and degree of compression.
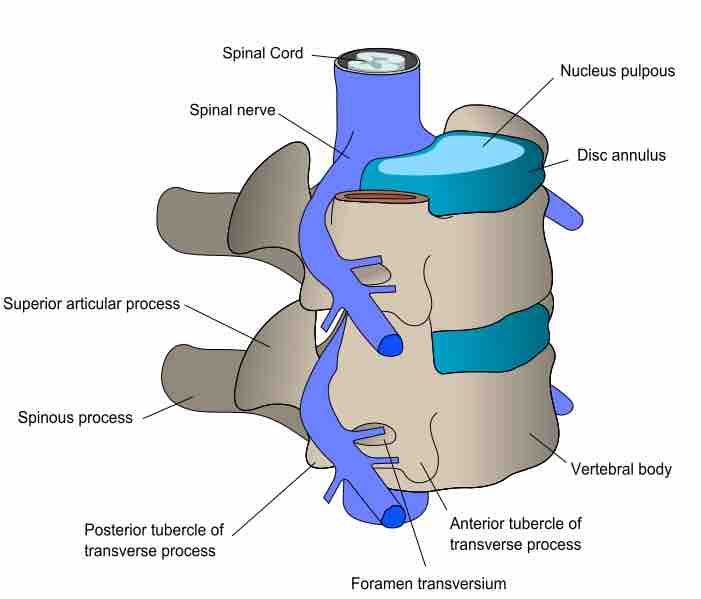
Structure of cervical spine:
- The cervical spine is composed of the first seven vertebrae C1-C7. The spine is connected by ligaments and supported by muscles. The spine is separated by discs, which act as shock absorbers and provide cushioning. The spinal nerves come out from openings in the spinal cord called foramen. The nerves from the cervical spine conduct sensory messages which provide motor control to the muscles of the neck, upper back, shoulders, and arms.
Causes of Cervical Degenerative Disc Disease:
- Cervical degenerative disc disease generally occurs when one or more of the cushioning discs in the cervical vertebrae starts to break down because of wear and tear. There may be a hereditary component that predisposes some people to wear and tear. The injury may also accelerate and cause degenerative changes in the spine.
- The degeneration in the cervical spine is sometimes caused by trauma, such as an accident or a fall. Some people can trace the starting of their neck pain to an incident that resulted from trauma. However, degeneration is often due to wear and tear or repetitive movements.
Symptoms of Cervical Degenerative Disc Disease:
- Cervical disc degenerative disease characterized by neck pain. Repetitive movements or postural strains may give rise to pain on the posterior aspect of the neck over the trapezius. Stiffness or reduce cervical movements and grating may also be present on movement. Tenderness may present at the affected cervical level.
- Radiating pain from the shoulder, arm, hands, and digits along the course of the nerve indicates nerve root compression. Paraesthesia in the form of tingling, burning, and numbness may be present in the hand. This symptom can interfere with activities such as typing, holding objects, or writing.
- Muscular weakness or sensory impairment also happens in rare cases. Sometimes headaches occur from cervical degenerative disc problems.
Risk factors of Cervical Degenerative Disc Disease:
- Cervical degenerative disc disease commonly develops with age, But there are some factors that can make it sooner: Genetic, Obesity, Smoking, Poor posture, Trauma such as an accident or fall injury, and such as a herniated disc, which can accelerate cervical degenerative disc disease.
How to diagnose Cervical Degenerative Disc Disease:
- This condition can be diagnosed by following the process;
- Medical history: If the patient has any medical history relevant to current symptoms.
- Physical examination: By palpating the neck and measuring the range of motion of the neck. Ask to do certain movements and see if the pain increased or decreased. Check whether any neurological symptoms are present or not. such as pain with tingling or numbness and weakness in the shoulder, arm, and hands. Perform special tests for proper diagnosis.
- Imaging study: X-ray, MRI, and CT scan to confirm whether and where degeneration is occurring, as well as identify other conditions.
Other conditions associated with cervical degenerating disc disease:
- Herniated cervical disc: A degenerating cervical disc has its nucleus wedge into tears in the annulus fibrosus. When the Nucleus pulposus came through the annulus fibrosus, then the disc is considered herniated.
- Cervical myelopathy: Cervical Myelopathy is a disease of the spinal cord. It results from degeneration or stenosis of the central spinal canal.
- Cervical osteoarthritis: It is a disc degeneration in which space between the intervertebral joints is decreased.
- Cervical spinal stenosis: It is a narrowing of the spinal canal, which the spinal cord runs through, due to the formation of bone spurs. it can lead to degeneration of the disc.
- Cervical Spondylolisthesis: When one vertebra slipped forward to another vertebra it calls spondylolisthesis. It is rarely seen condition in the cervical region.
- There are many other conditions like, cervical syndrome, prolapsed cervical disc, and cervical radiculopathy which is associated with degenerating disc disease.
Treatment for Cervical Degenerative Disc Disease:
It depends on the severity of the condition. There are two treatment options for this cervical degenerative disc condition.
1. Non-surgical management
2. Surgical management
I. Non-surgical management:
- There are the following treatments for cervical degenerative disc conditions:
Rest or lifestyle modification:
- Certain daily activities might be more painful for the neck, such as working on the computer monitor for a long time, writing for long hours, work with a forward head. Modifying these certain activities will usually reduce the pain. Take a rest between working hours
Pain management with medication or injections:
- Pain relievers, such as acetaminophen or others might be beneficial. If they do not work, a stronger pain medication, such as oral steroids or muscle relaxants may be prescribed. Also, topical ointment can be used for pain relief such as diclofenac gel. Other options could include an injection, such as a cervical epidural steroid injection.
Ice or heat therapy:
- Pain can be relieved by applying an ice pack or a heat pack to the affected part.
Physical therapy:
- Physical agents and Massage
- Exercises
- Cervical traction
- Cervical manipulation
- Postural and ergonomic advice
1. Physical agents and massage:
There are various physical agents which can be used mainly to :
- control inflammation
- control pain and spasms
- Reduce stiffness of soft tissue and joints
- Increase blood supply and relieve ischemia
- In the earliest stage following modalities can be used for pain reduction and relaxation
- Superficial modalities hydro collator packs and infrared; subsequently, deep heating modalities such as short-wave diathermy, microwave, and ultrasound can be used.
- Pain reduction using cryotherapy in the form of ice massage and ice packs, TENS, IFT, and dial pulse is useful.
Massage:
- Deep massage techniques such as effleurage, kneading, and friction to the localized areas effectively reduce the spasm and pain and induce relaxation.
2. Exercises:
The type of exercise is to be planned according to the patient’s needs, inabilities, and comfort.
Relaxed passive movements:
- This includes manipulation and mobilization when the chief aim is mobilization.
Stretching exercises:
- Stretching helps maintain or increase the range of motion and improves the cervical joints’ flexibility.
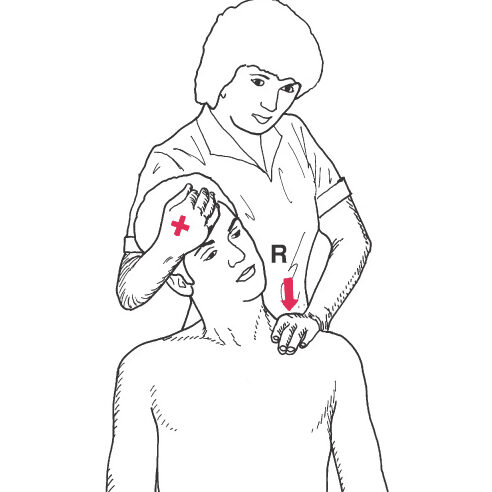
Scalene muscle stretch-
- Manual stretching exercise:
- In a sitting position, The patient first performs chin tuck and then side bends.
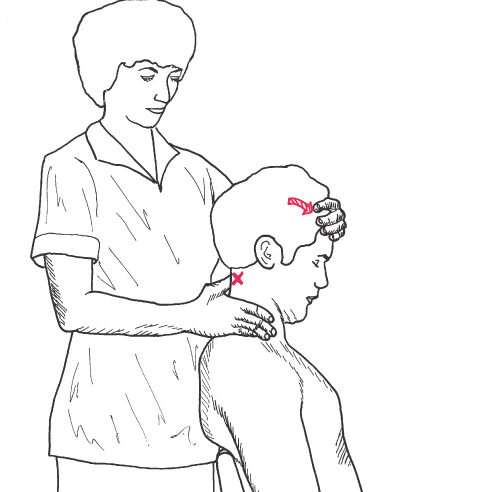
- The Therapist stands behind the patient and stabilizes the head with one hand around the side of the patient’s head and face, holding the head against the trunk and shoulder. Place the other hand across the top of the rib cage on the side of the tightness.
- Instruct the patient to inhale and exhale; apply downward pressure as the patient inhale again. As the patient exhales, take up the slack. Repeat. This is a gentle, hold-and-relax stretching technique. Describe as figure.1.1.
- Self-stretching exercise:
- The patient is Sitting on a chair or table with a straight back. bend the head to one side, and keep the chin straight. Gently tense or stretch the neck muscle.
- Tilt the head to one side, and over the shoulder, while keeping the chin straight.
- Gently stretch, he or she leans away from the table, inhales, exhales, and holds the stretch position for 20-30 seconds, returning to the normal position.
- Repeat the exercise 3-5 times on both sides.
Suboccipital muscle stretch-
- Manual stretching exercise:
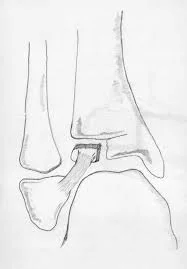
- In the sitting position, Identify the spinous process of the second cervical spine and stabilize it with the thumb or with the second MCP joint.
- Have the patient slowly nod, doing just a motion of the head on the upper spine.
- Place the other hand across the patient’s forehead and guide the movement. Describe as figure.1.2.
- Self-stretching exercise:
- The patient is in a supine or sitting position and has to perform a chin tuck, then flex the neck, and bring the chin toward the throat or neck until a stretch is felt.
- The patient has to put pressure over the back of the head with the hand while doing the head forward to reinforce the movement.
- For a unilateral stretch, the patient is to do a chin tuck, then rotate gently 45° towards both sides then nod.
- Repeat the exercise 3-5 times.
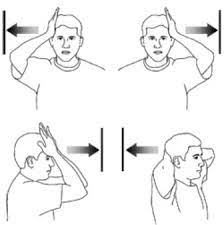
Isometric exercises: Self-Resistance
- The intensity of the isometric exercises is depending upon the patient’s tolerance and symptoms.
- Patient Position and Procedure: Sitting
- 1. Flexion: The patient Places both hands on the forehead and presses the forehead into the palms. that time motion is not allowed.
- 2. Side bending/flexion: The patient Places one hand against the side to perform the motion and tries to bring the head toward the shoulder but the motion is not allowed.
- 3. Extension: The patient Presses the back of the head with both hands, close to the top of the head.
- 4. Rotation: The patient presses one hand against the region just superior and lateral to the eye and performs to turn the head to look over the shoulder without allowing motion.
Isometric resistance activities:
- The Patient Position and Procedure: Standing with the ball between the forehead and wall. the patient keeps the chin tucked and does not go into a forward-head posture.
- The patient maintains this position while superimposing arm motions. This can progress by using weights.
Manual resistance: For cervical muscles
- The Patient Position and Procedure: Supine. Therapist position: Stand at the end of the table and support the patient’s head for exercise.
- Place one hand on the patient’s head to resist the opposite motion. The resistance is given to isolated muscle actions or general ROMs, whichever best gains muscle balance and function.
- Avoid jerking when applying or releasing the resistance, and gradually increase the intensity.
- Ask the patient to match your resistance, holding and releasing then ask to relax.
Muscle energy techniques(MET):
- This technique is also used to increase craniocervical mobility and improve joint mobility. The Patient holds the muscle contraction against the therapist’s resistance for 3-5 seconds, then relax. Do 3 to 5 repetitions.
PNF techniques:
PNF technique for cervical is also used to improve stability and strength.
Cervical traction:
- Cervical traction is applicable in problems from sprains, fractures, dislocations, and degeneration of the cervical vertebrae.
- There is static or continuous and intermittent cervical traction that can be used in these conditions.
- Cervical traction was given in supine and sitting positions.
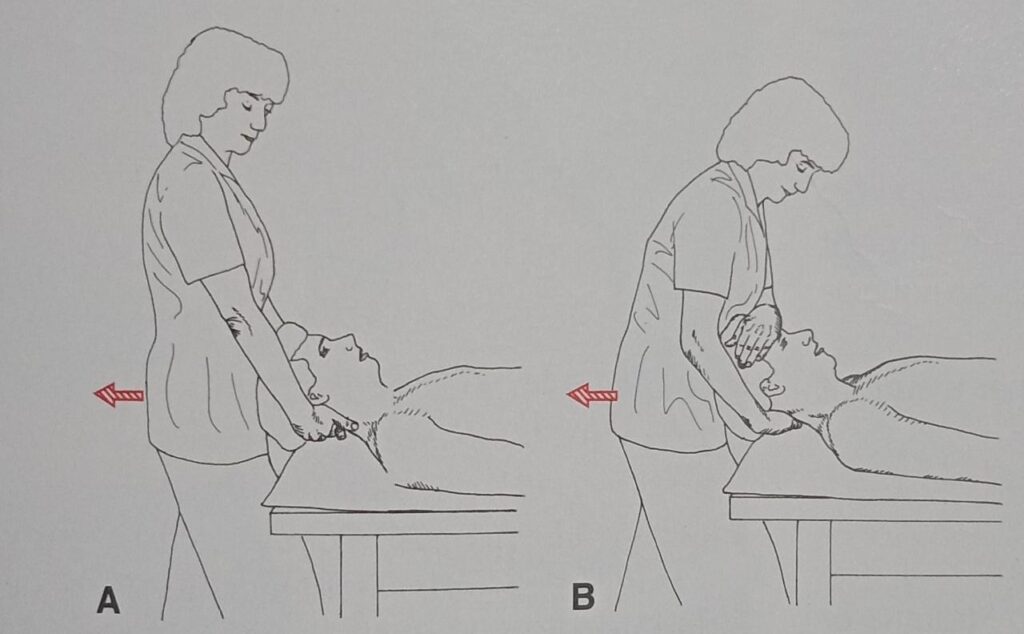
- Manual Traction: for the cervical spine:
- The traction technique is used for the purposes of stretching the muscles and the facet joint capsules and widening the intervertebral foramina, the force can be specially applied with minimum stress to regions that should not be stretched.
- Procedure and Position: Supine and the therapist stand at the head of the treatment table.
- Placement depends on the comfort of the therapist and patient.
- Place the fingers of both hands under the occiput. also can place one hand over the forehead and another hand under the occiput.
- Cervical Traction:
- It is a modality of choice for cervical dysfunctions.
- There are continuous, static, intermittent, and polyaxially types of cervical traction, which can use in this condition.
- Traction should be applied in the position of greatest comfort.
- Contraindication to traction: Ligamentous instability, malignancy, fracture, rheumatoid arthritis with necrosis of the ligaments adjacent to the traction level.
Cervical manipulation:
- In cervical spondylosis, cervical manipulation techniques are very effective, provided the spondylosis is not too advanced.
- The cervical manipulation techniques are indicated for pain modulation and to improve joint motion.
- Precautions should be taken during this technique.
- Contraindications for manipulation: Unhealed fracture, rheumatoid arthritis, vertebral artery disease, acute joint inflammation.
Postural and ergonomic advice:
- Advice on the maintenance of posture of the neck in relation to various body positions and ergonomics plays a predominant role in the majority of patients with cervical pain. Faulty posture also accelerates degenerative changes.
- The correct posture of the neck during working is observed, to avoid excessive stress. The ideal posture is a straight neck with the chin tucked in. Ergonomic advice is the most important approach which can prevent recurrent neck pain. Educate the patient on correct ergonomics to prevent common neck pain.
II. Surgical management for cervical degenerative disc disease:
- Surgery for cervical degenerative disc disease is generally considered in the following cases:
- If there are neurological symptoms present, such as numbness and weakness in arms, and hands. In these cases, surgery may be recommended to reduce further complications like nerve damage due to pressure on nerve roots.
- If the chronic pain is not relieved after at least six months of non-surgical treatments, and difficulty performing daily living activities. Better surgical results are predicted for patients with these complaints.
The most common types of surgery for CDDD are as follows:
- Anterior cervical discectomy: The most common surgery for cervical disc diseases involves a discectomy, which is the removal of an injured part of the disc and decompression of the nerve root in the cervical spine. Typically, the surgery is performed through the front of the neck, called “anterior cervical discectomy”.
- Cervical fusion: Cervical fusion is act as a bridge between the vertebrae after worn out the affected disc of the cervical spine is removed by using a graft of bone or metal plats, if there is any need to remove the vertebrae, the surgeon will remove entire vertebrae and will fuse the cervical spine, this procedure called as cervical fusion.
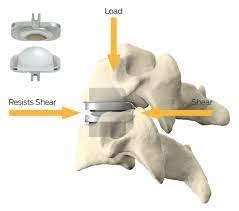
- Cervical artificial disc replacement: This is a procedure in which the affected disc is removed and replacing it with an artificial disc. These cervical artificial disc replacement results may be a very good option in patients with initial arthritic changes to the posterior facets. It’ll get relief from pain and also help to maintain the regular normal movement of the cervical vertebrae.
Post-operative physiotherapy management:
- In the immediate post-operative phase: The patient is kept in bed for at least 10-12 days after the operation.
- Use a cervical collar for immobilization.
- The following advice was given to the patient during this phase:
- Avoid strenuous activities
- Chest physiotherapy
- Lower extremity movements
- During mobilization: In this phase exercise started at low intensity.
- Isometric exercise of the neck muscles.
- Stretching exercise of the neck for increased mobility.
- Active and passive ROM exercises can be performed after the doctor suggested.
- Do the exercises slowly and smoothly. Do not make any fast or jerky movements. Stop exercise that causes pain, nausea, dizziness, or discomfort.
FAQs
1. What is cervical degenerative disc disease?
Cervical degenerative disc disease is known as one or more discs of the cervical spine starting to break down due to degeneration or wear and tear.
2. Causes of cervical degenerative disc disease?
Cervical degenerative disc disease generally occurs when one or more of the cushioning discs in the cervical vertebrae starts to break down because of wear and tear. Also can occur due to trauma.
3. Common symptoms of cervical degenerative disc disease:
Neck pain, tenderness at the back of the neck, stiffness, radiating pain in the arm, muscular weakness.
4. The most common exercise for cervical degenerative disc disease:
Isometric exercise of the neck, stretching exercise of neck muscles, relaxed passive movements.
5. The most common types of surgery for cervical degenerative disc disease:
Anterior cervical discectomy, Cervical spine fusion, Cervical Laminectomy, Cervical artificial disc replacement.