Achilles Tendinitis
Table of Contents
What is an Achilles Tendinitis?
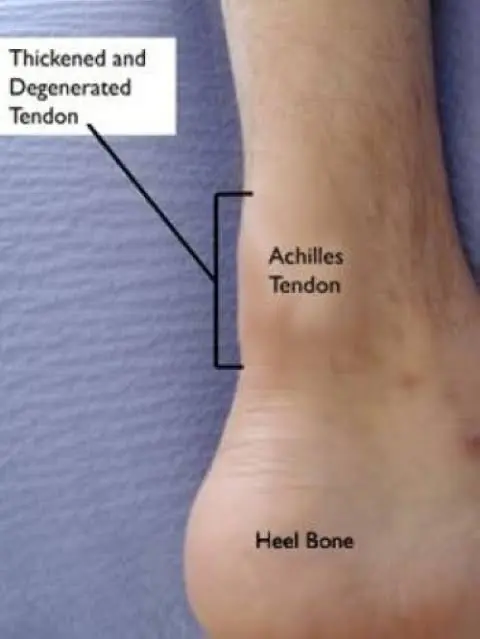
Achilles tendinitis is a common condition characterized by inflammation of the Achilles tendon, the large tendon that connects the calf muscles to the heel bone. This tendon plays a crucial role in activities such as walking, running, and jumping, making it susceptible to overuse and injury.
The condition typically develops when the Achilles tendon is subjected to repetitive stress or strain, leading to micro-tears and inflammation. Athletes, particularly runners, are often prone to Achilles tendinitis due to the repetitive nature of their activities. However, it can affect individuals of all activity levels.
An inflammation of a tendon is called tendinitis. Thick tissue cords called tendons connect muscles to bones. The longest and strongest tendon in the body is the Achilles tendon. One of the most typical causes of foot or ankle pain is Achilles tendinitis, or inflammation of the Achilles tendon. Peroneal tendinitis and posterior Tibial tendinitis are two more forms of tendinitis affecting the foot and ankle.
Causes of Achilles Tendinitis
Overuse or an injury can cause tendinitis. Tendinitis can also arise as a result of improper form when exercising or improper stretching before exertion. Tendinitis is more common in some people, such as those who have arthritis, “flat feet,” or tight tendons.
Symptoms of Achilles Tendinitis
When you walk or run, the pain and swelling in the back of your heel are the primary signs of Achilles tendinitis. Additionally, you might have a restricted range of motion when you flex your foot and tight calf muscles.
Other typical signs of Achilles tendinitis include:
Discomfort when touching or moving your heel or the area behind your calf
Discomfort or swelling in that region that gets worse when you walk or run, or discomfort or swelling in the back of your heel the day after you work out
Stiffness and soreness in the Achilles tendon upon waking up, warmth around the heel or along the tendon, limited range of motion when flexing your foot, and thickening of the Achilles tendon.
Diagnosis
The first thing your healthcare practitioner will do is a physical examination. When you stand on your toes, your doctor will check for pain and sensitivity in the tendon’s surrounding area.
Thompson Test
By applying pressure to the calf, the Thompson test verifies the strength of the Achilles tendon. To determine whether a full Achilles rupture is present, it is done as a clinical test.
Technique
Placing his foot over the end of the table, the patient rests prone. As an alternative, the patient can lie prone and flex his knee to a 90-degree angle. Using his hand, the examiner applies pressure on the gastrocnemius-soleus complex, which is located in the calf muscles. Plantar flexion should ensue from the Achilles tendon contracting as a result of calf flexion. There won’t be any visible plantar flexion if the Achilles tendon is totally torn.
An MRI scan may be performed if you are thinking about surgery or if there is a possibility that you have an Achilles tendon injury. X-rays can aid in the diagnosis of bone issues.
Treatment of Achilles Tendinitis
Management of Achilles tendinitis involves rest, ice, compression, and elevation (RICE), along with exercises to strengthen the calf muscles and improve flexibility.
In some cases, medical interventions such as physical therapy or anti-inflammatory medications may be recommended. Early detection and appropriate treatment are crucial for a successful recovery and preventing the development of chronic conditions.
Medical Treatments
Drug
If over-the-counter pain relievers like naproxen (Aleve) or ibuprofen (Advil, Motrin IB, etc.) don’t work well enough, your doctor may recommend stronger drugs to lower inflammation and relieve pain.
Corticosteroids also use.
Injections of sclerosing
In a pilot investigation, the role of neovascularization in tendon discomfort was investigated further. The area is anterior to the tendon exhibiting neovascularization was injected with a vascular sclerosant, an aliphatic non-ionized nitrogen-free chemical with a sclerosing and anaesthetic effect). After an average of two sessions, the vast majority of patients were pain-free, according to a short-term (6 months) review of this treatment.
There was no external or internal neovascularization in the painless tendons. Following up on these patients for two years revealed that all eight of them were still pain-free and had no vessels in their tendons. Tendon thickness had reduced and the structure appeared somewhat normal on ultrasonography
Following a sclerosing injection, rehabilitation entails resting for one to three days before increasing tendon-loading exercise. Progressively avoiding the highest burden. Tendon loading exercises, such as sprinting, jumping, and heaving strength training, are permitted after two weeks. According to this study, sclerosing therapy may have therapeutic use for people who don’t respond to eccentric exercise.
Injections of platelet-rich plasma
When compared to a placebo (saline), injections of Platelet-Rich Plasma (PRP) given to patients with chronic Achilles tendinopathy over a three-month period show no beneficial effects. The only noteworthy difference between PRP injections and placebo was an increase in tendon thickness; this suggests that PRP treatments, as opposed to saline injections, could thicken tendons.
Minimum invasive techniques
Insertional Achilles tendinopathy is a frequent and chronic musculoskeletal illness that causes discomfort in the Achilles tendon. It is treated using a minimally invasive surgery. For sportsmen who engage in push-off exercises, such as basketball and soccer players, the chronic degenerative condition frequently causes pain. In contrast to the 23-week recovery period following typical open surgery, the keyhole method known as percutaneous Zadek osteotomy (ZO) may considerably lessen pain and give pain relief within six weeks of the procedure.
For the two weeks of the brief healing time, the foot is protected with a splint or walker boot. After four weeks, weight bearing is resumed while the walker boot is removed. Additionally, two weeks following surgery, physiotherapy starts. After the outpatient surgery, athletes are permitted to resume wearing shoes after six weeks.
Operative Procedure
The goal of surgical management for tendinopathy is to cause tendon irritation in order to trigger a chemically mediated response. Simple treatments, open procedures, percutaneous tenotomy, and excision of the infected tendon portion are all possible surgical options. After 18 months, 75% of patients who had tenotomies had a favorable outcome. The Achilles tendon treated openly produced better results for tendons free of a localized lesion.
In the event that your Achilles tendon is torn and several months of more conservative therapy are ineffective, your doctor might recommend surgery to repair it.
Physical Therapy
A physical therapist may recommend one or more of the following courses of treatment:
Practises. To encourage the healing and strengthening of the Achilles tendon and its supporting structures, therapists frequently recommend particular stretching and strengthening exercises.
It has been discovered that ”eccentric” strengthening—a unique kind of strengthening that involves slowly lowering a weight after raising it—is particularly beneficial for chronic Achilles issues.
Enhancing the tendon’s ability to store energy is the main objective of treating tendinopathy. It refers to the tendon’s and the related muscle’s capacity to operate and control load, effectively serving as a “spring” to store and release energy. There are three essential workouts for Achilles tendinopathy:
Isometric Loading
Isotonic Loading
Energy Storage Loading.
Phase 1: Isometric load exercises: Achilles tendon holds
Achilles tendon pain management has evolved significantly in the last several years. The adoption of isometric tendon loading as the cornerstone of treatment for tendinopathy is one notable shift. It has been discovered that isometric tendon loading maintains some baseline strength while also having pain-relieving benefits on tendons. Two methods can be used for these, depending on the symptoms and sensitivity of the tendons: double legs or a single leg. Double leg holds, frequently with shorter durations and fewer repetitions, can be used for Achilles tendon hyperirritability. The isometric hold can be placed halfway up or at the midpoint of the range, that is, directly up on the toes.
Phase 2: Isotonic Loading- Calf raises
When the athlete’s pain level and the tendon’s irritation decrease, these activities are frequently started. When an athlete should begin receiving isotonic loading for Achilles tendinopathy therapy, there are no “hard and fast” guidelines. Once their morning tendon stiffness has greatly decreased and they have less than 5/10 pain on NRS or tolerable and acceptable pain on repeated single-leg calf raises, then graduated isotonic loading is started.
Strengthening the tendon and the surrounding muscles is the ultimate aim of the isotonic workout. The strength of the soleus and gastrocnemius muscles is important when it comes to the Achilles tendon. Recurrent loading, such as when the tendon matrix is not sufficiently adapted by walking or running, nor the ability of the muscle-tendon unit to perform. Therefore, for the isotonic loaded exercises, higher loads are needed.
One can conduct isotonic seated calf raises by gradually increasing the loading. To create tension in the tendon, complete each repetition for three to six seconds.
It is recommended to execute isotonic standing calf raises at the midpoint of the muscle’s range of motion. Engaging in heavy slow resistance (HSR) exercise in the mid-range has the advantage of preventing tendon compression near the end of the range, which can happen when exercising with heavier weights. For instance, the Achilles tendon is susceptible to compressive forces at the extreme limit of ankle plantar flexion (toes pointing) or dorsiflexion (imagine letting the heel drop off the edge of a step). Loads against the calcaneus, the heel bone, which may cause discomfort and irritability.
Phase 3: Energy Storage Loading- Plyometric Exercises
The start and completion of “energy storage” tendon activities constitute the final and most important phase of rehabilitation. The tendon is deformed during these activities, which involve hopping and jumping. Through the stretch-shortening cycle that occurs when an athlete lands and then pushes off at toe-off, these workouts assist the tendon in regaining its ability to absorb and then release energy.
When the athlete reports little to no improvement in morning Achilles tendon stiffness upon awakening, these workouts might be started. Athletes should also meet certain additional requirements before beginning these exercises, such as having progressed well with isotonic calf raise exercises, having very little tenderness palpable in the Achilles tendon, and being able to handle light running without experiencing a flare-up in tendon irritability or worsening of symptoms.
For instance, lengthening the time under tension during intense slow-resistance training may put more pressure on the tendon and promote greater adaptation; yet, speeding up will probably enhance power and better prepare for sports that need the Stretch Shortening Cycle.
The listed exercises are as follows:
Two-legged hop
One leg hop
One leg step hop
Hopscotch with band
Tapping
Expert opinion, not clinical data, supports antipronation tape. Taping may be used in the acute period, perhaps before Introduction to Orthotics. When treating patients with Achilles tendinopathy, clinicians shouldn’t utilize therapeutic elastic tape to ease pain or enhance functional performance. In patients with Achilles tendinopathy, clinicians may employ stiff taping to modify foot posture and/or lessen tension on the Achilles tendon.
Night splints
Expert opinion exists to Encourage the use of braces and night splints during the acute phase.
There is a fair amount of research against the long-term use of braces and night splints.
In the acute stage, think about utilizing night splints and braces; nevertheless, do not use them in the chronic stage in addition to exercising.
Electro modalities
The use of dexamethasone in iontophoresis during the acute phase, but not during the chronic phase. Iontophoresis’s function is still being studied. When the condition is acute, iontophoresis with 0.4% aqueous dexamethasone and 80 mA min may be tried in six sessions spread over three weeks. If exercise loading is tolerated, a programme of concentric-eccentric exercises should be continued in addition to iontophoresis.
Extracorporeal shock wave therapy (ESWT)
The use of extracorporeal shock wave therapy (ESWT) during the chronic stage is supported by conflicting evidence. Research indicates that shock wave energy dose (EFD ‐ energy flux density = mJ/mm²) determines the results instead of shock wave generating type (focused vs. radial ESWT). Additionally, there is proof that the efficacy of ESWT is diminished when anaesthetic is used, as required in high-energy regimens. As a result, it is advised to use low-energy ESWT procedures instead of anaesthesia since they are more workable, bearable, and cost-effective while producing results that are comparable. It is possible to use low-energy ESWT techniques for both radial and focused ESWT. If alternative therapies have failed, take into consideration a trial of ESWT in the chronic stage at the following
Parameter
Low energy SWT
EFD=0.18 – 0.3 mJ/mm² (2‐4 Bars)
Shocks – 2000 ‐3000
Frequency ‐30 Hz
Duration – 3‐5 sessions, weekly intervals.
Home Treatment of Achilles Tendinitis
Castor Oil
This plant-based oil is used to treat a variety of conditions, including wrinkles, dandruff, and stomach discomfort. For the treatment of Achilles tendon pain, castor oil is the recommended oil. How can oil perform so many tasks? We know that castor oil is a triglyceride, and that nearly ninety percent of its content is the powerful anti-inflammatory ricinoleic acid. When applied to the affected areas, the acid in castor oil reduces Achilles tendon pain and inflammation.
Vitamin E Oil
Second, vitamin E oil is a strong antioxidant. By eliminating pain-causing free radicals from the body, vitamin E aids in the reduction of inflammation and pain. Additionally, the oil promotes healthy circulation, which eases soreness and swelling.
Turmeric
As we all know, turmeric is a wonder spice. Because curcumin is present, it is a great treatment for Achilles tendon pain. The scientific community as a whole affirms that curcumin ranks among the best naturally occurring analgesics.
Curcumin lessens pain by triggering the opioid system, which is connected to our body’s reaction to pain. Additionally, curcumin has anti-inflammatory properties.
Turmeric has anti-inflammatory properties that can be reaped by using it as a tincture, in tea, or even as a garnish for food. Using turmeric in other ways includes applying a poultice to your painful Achilles tendon to reduce inflammation.
Resting The Affected Leg
Overuse is the primary cause of Achilles tendon injuries. Thus, getting enough sleep is a useful self-care strategy for easing Achilles tendon pain. Rest your Achilles tendon by avoiding activities that put a strain on it, such as running, climbing stairs, and even excessive walking. We would advise you to start exercising by swimming instead. But be patient—it can take days, weeks, or even months for Achilles tendon pain to go away.
Cold Compresses
Two of Achilles tendinitis’ primary symptoms, pain, and swelling, can be lessened with the use of a cold compress. It will also aid in the afflicted muscles’ relaxation
Elastic Bandages Or Warm Wraps
To lessen the strain on the injured muscles, apply compressive, elastic bandages or warm wraps. This in turn expedites the healing process and reduces pain and swelling.
Massage
Another effective treatment for Achilles tendinitis is massage. A light massage can ease muscle tension, improve circulation, and lessen stiffness and edoema. Use olive, coconut, sesame, or mustard oil when massaging.
Avoid the Use of Tobacco
Smoking hinders healing by reducing blood flow to the injured areas and postponing tissue restoration. This implies that the tendon pain will last longer for you. Thus, give up using tobacco products.
Put On Protective Footwear
We advise you to choose athletic shoes that cushion the heel and support the arch of your injured foot. The Achilles tendon has an opportunity to heal thanks to this shoe. Another excellent option are silicone heel pads, which lessen the strain on the Achilles tendon. These are some methods for treating Achilles tendon pain, not exactly home remedies.
Brace while Sleeping
Wear a night brace while you sleep to avoid the shortening and stiffening of your tendon. This will ensure that your Achilles tendon receives the best possible rest while you sleep, ensuring that your heel and calf will be less sore and stiff during the day.
These are the successful home treatments for Achilles tendon. If you are overweight, we also advise you to lose weight in order to prevent further Achilles tendon injuries. Please let us know if using our advice has made your Achilles tendon painless.
How to Prevent Achilles Tendinitis?
Your podiatrist will collaborate with you to lower your risk of tendinitis reoccurring. Custom orthotics can lessen excessive pressures or strains and help you control how your feet move. In order to improve the elasticity of the tendon and fortify the muscles that are connected to it, he or she might also suggest specific stretches or exercises. Reducing the chance of re-injury can be achieved by gradually increasing your level of activity.
Summary
An overuse injury to the Achilles tendon, which connects your heel bone to the calf muscles at the back of your lower leg, is known as Achilles tendinitis.
It’s also typical among middle-aged individuals who participate in weekend-only sports like basketball or tennis.
Under your doctor’s supervision, the majority of cases of Achilles tendinitis can be treated with reasonably straightforward at-home care. In most cases, self-care techniques are required to stop recurrent episodes. Severe instances of Achilles tendinitis can result in tendon ruptures or tears, which may need to be surgically repaired.
FAQs
When running or walking, there is pain in the tendon’s length and in the heel.
In the morning, there is stiffness and pain in that area.
Rest(Exercise avoidance for a few days or a transfer to an activity like swimming that doesn’t strain the Achilles tendon may be necessary), Ice, Contraction, and elevation.
Degeneration causes structural alterations in the tendon that are mostly permanent.
The blood flow to tendons is not as great as that of muscle tissue.
References
- Home remedies for achilles tendinitis. (n.d.). Cornerstone Foot & Ankle. https://www.cornerstonefootandankle.com/blog/achilles-tendinitis-top-5-home-remedies.cfm
- tendinitis – Diagnosis & treatment – Mayo Clinic. (2021, September 30). M Achilles ayo Clinic. https://www.mayoclinic.org/diseases-conditions/achilles-tendinitis/diagnosis-treatment/drc-20369025
- Badii, C. (2023, July 3). Achilles Tendinitis. Healthline. https://www.healthline.com/health/achilles-tendinitis#symptoms
- Rcsadmin. (2020, February 19). Popular home remedies for Achilles tendon injury. Orthopaedic Surgery Associates in Boca Raton & Boynton Beach. https://ortho-surgeon.com/popular-home-remedies-for-achilles-tendon-injury/
- Achilles tendinopathy. (n.d.). Physiopedia. https://www.physio-pedia.com/Achilles_Tendinopathy







6 Comments