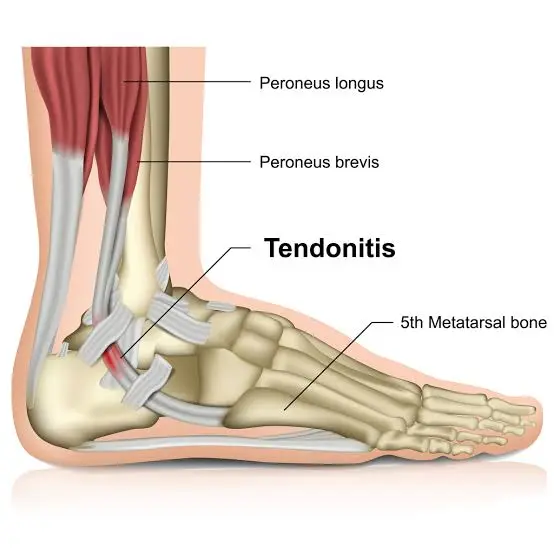
Peroneal Tendonitis
Table of Contents
What is a Peroneal Tendonitis?
An injury to the tendons in the foot and/or ankle is called peroneal tendinopathy. Athletes like basketball players, dancers, and long-distance runners are frequently affected. This condition can also affect people with weak ankles or those who have had ankle sprains.
Common symptoms include pain along the outside surface of the ankle that worsens with movement and gets better with rest. Physical therapists assist patients with peroneal tendinopathy in strengthening their muscles and lessening the strain on their ankles and feet.
Related Anatomy
Anatomy of Peroneus longus
The lateral compartment of the lower leg is composed of the Fibularis Brevis and Peroneus (Fibularis) Longus muscles. The largest of the Fibularis muscles is the Fibularis Longus, which is located superficially to the Fibularis Brevis. The Fibularis Longus extends into the lower limb’s lateral compartment, where it tapers into a long tendon that descends into the foot at the midpoint.
Origin – Tibia’s lateral condyle. Head and the first two-thirds of the fibula’s lateral surface, Septa between muscles adjacent deep fascia
Insertion – The peroneus longus tendon curves distally in the cuboid tunnel and at the retro malleolar region. The superior peroneal retinaculum holds the tendon and the peroneus brevis tendon in place within the retro-malleolar groove. First metatarsal lateral base: medial cuneiform bone
Nerve supply – L5, S1, S2: Superficial Peroneal (Fibular) nerve.
Arterial supply – Anterior Artery The arteries of the tibia and peronea (Fibular).
Function
- Ankle and foot eversion
- Helps with plantar flexion of the ankle
- The first metatarsal head depresses in a weight-bearing position because of the forceful pull at its insertion.
- Keeps the foot’s transverse arch intact because of the way it passes over the sole.
- Prevents the lateral leg from collapsing medially and stabilizes the leg on the foot in a single-leg stance.
- Patients who are young, active, and who play sports like football, soccer, and running are more likely to suffer from peroneal tendon injuries.
Clinical correlation – It can affect the fibularis longus muscle, including:
- Peroneal tendinopathy
- Peroneal Tendon Instability or subluxation
- Weakness
- Reduces the capacity to balance on tiptoe
- Reduces the ankle’s lateral stability
- Allows the foot to be in a varus position.
- Bending or shortening: leads to a valgus or everted foot.
- Tendon tears and muscles of the fibularis longus: Due to subluxation over the fibula, tears are most frequently longitudinal, but they can also appear transverse.
- Tearing of the peroneus longus tendon causes fibular avulsion fractures.
- Compartments Syndrome
- Overlying fascia-induced muscle herniation can manifest as a mass over the lateral calf.
- Muscle contraction and dynamic ultrasound are the best methods for assessment.
Peroneus brevis anatomy
The short muscle called Peroneus Brevis, sometimes called Fibularis Brevis is located deep in the Fibularis Longus in the lateral region of the lower leg. Fibularis Longus, Fibularis Brevis, and Fibularis Tertius are the three ankle everters that make up the fibularis muscles. A lateral ankle sprain frequently injures the Fibularis Brevis and Fibularis Longus, and the most frequently dislocated tendon is that of the Fibularis Brevis muscle.
Origin – The distal two-thirds of the lateral fibula is the source of the Fibularis Brevis. Its tendon loops posterior to the lateral malleolus after passing downward.
Insertion – on the styloid process at the proximal end of the fifth metatarsal, the Fibularis Brevis inserts.
Nerve supply – Nerve Surface Nerve of the Fibular (Peroneal) (L5-S2).
Arterial supply – Muscular branches of the peroneal, or fibular
Function – Together with the Fibularis Longus, the Fibularis Brevis provides 63% of the force required to evert the foot and aids in plantar flexion. Together, the fibularis muscles provide dynamic lateral ankle stability when there is an abrupt stress on the ankle inversion.
Clinical correlation – Together with the Fibularis Longus, the Fibularis Brevis provides 63% of the force required to evert the foot and aids in plantar flexion. Together, the fibularis muscles provide dynamic lateral ankle stability when there is an abrupt stress on the ankle inversion.
In physiotherapy, foot and ankle injuries are frequently observed, with a high incidence of those injuries occurring at the lateral ankle. The most frequent injuries to the Fibularis Brevis tendon are tendinopathy, sprains, splits, and dislocations/subluxations. Supination or inversion forces are typically the source of tendon injuries to the Fibularis Brevis. In the event of a lateral ankle sprain, there is associated injury of Fibularis Brevis.
Causes of the Peroneal Tendonitis
Overuse of the tendons repeatedly can lead to the development of peroneal tendon inflammation over time. Alternatively, an acute ankle injury such as a sprain could cause it to happen suddenly. It can be difficult for tendons to move smoothly due to swelling in the tendons or the lubricated sheath surrounding them.
Epidemiology of the Peroneal Tendonitis
Compared to other forms of tendonitis in the foot, like Achilles tendonitis, peroneal tendonitis is less common. Out of thousands of runners, only 13 cases (less than 1%) had peroneal tendonitis in one study.
Symptoms of the Peroneal Tendonitis
Peroneal tendonitis symptoms could include:
- Pain down your tendon in your ankle.
- Discomfort that worsens with movement.
- Redness, warmth, or swelling around your tendon.
- Thickened tendons that move with your tendon, accompanied by a mass or nodule.
- Peroneal tendonitis can develop into a tendon rupture if left untreated. This happens when a tendon tears all the way through or just partially. Tendon subluxation, or tendon dislocation, can also result from weak or damaged tendons. Subluxations or rips can result in:
- Ankle instability or weakness.
- Severe discomfort on the outside of your ankle and foot.
- A snapping, sharp sensation in your tendons.
Risk factor of the Peroneal Tendonitis
Peroneal tendonitis can affect anyone, but athletes who play sports requiring a lot of ankle movement are more likely to get it. Peroneal tendinitis is also more likely to occur if you:
- A person of more than 40 age.
- Avoid stretching right before working out.
- Possess certain ailments, such as gout, diabetes, rheumatoid arthritis, or osteoarthritis.
- Possess a history of tendon injuries.
- Your feet are arched very high.
- You are obese or overweight.
- Possess taut tendons.
- Smoke.
When to visit a doctor?
Speak with your physician if you:
- You are incapable of using your foot or ankle to walk or bear any weight.
- You are unable to move your ankle in any way.
- Feel like something is popping or snapping in your ankle or foot.
- Experience acute, sudden pain in your ankle or foot.
- Take note of any swelling or discoloration in your ankle or foot.
Diagnosis of the peroneal tendinitis
Diagnosing peroneal tendonitis can be challenging. The signs and symptoms resemble those of sprains, fractures, and other foot and ankle issues. According to one study, roughly 60% of the 40 individuals with peroneal tendonitis were initially given the incorrect diagnosis.
But your doctor will examine you physically and go over your symptoms. To feel for any soreness or swelling, they might press or palpate specific areas of your foot and ankle. If your doctor wants to assess your ankle range of motion, they may also ask you to do specific movements. Imaging is sometimes required to rule out conditions such as torn tissue, osteoarthritis, cartilage damage, and foot fractures. An MRI, CT scan, ultrasound, or X-ray may also be suggested by your healthcare professional.
Differential Diagnosis of the peroneal tendinitis
Differentiating between peroneal tendinopathy can be challenging.
- Ankle Sprain: Talar Tilt Test, Anterior Drawer Test
- Ottawa ankle rules for fractured ankles
- MRI and passive forced plantar flexion in Os Trigonum syndrome
- Persistent lateral ankle pain with an additional cause:
- MRI showing a longitudinal peroneal tendon tear
- Ultrasonography, CT, MRI, or peroneal ethnography can detect peroneal subluxation
- Injury to the flexor hallucis longus tendon
Physiotherapy Examination of the Peroneal Tendonitis
A thought-provoking examination of peroneal pathology has been detailed. The patient’s foot is examined while it is hanging loosely and with its knee 90 degrees bent. The peroneal tendons are slightly compressed posterior to the fibula. Next, the patient is instructed to forcibly dorsiflexion and evert the foot. One may experience subluxation of the tendons or be prompted to pain.
Ankle tilt testing and the anterior drawer should be used to assess the stability of the lateral ankle ligaments.
Lower Extremity Functional Scale (LEFS): measuring “patients’ initial function, ongoing progress, and outcome” for a variety of lower-extremity conditions is the goal of the LEFS. It is scored from 0-80, where 80 represents no limitations, and can be used to assess the degree of difficulty of various functional tasks with a lower extremity disability.
The Foot and Ankle Ability Measure, or FAAM for short, is a 29-question self-report outcome measure designed to assess the physical function of patients with foot or foot disabilities. The two subscales of the questionnaire are sports and daily living activities.
Treatment of Peroneal Tendonitis
Immediate treatment for Peroneal Tendonitis
Within three to four weeks, conservative treatments typically help reduce tendon pain and inflammation. If tendonitis is the consequence of another injury, like a sprain, recovery may take longer.
For peroneal tendonitis, common treatments include:
- Bracing: If you have to run or jump, for example, an ankle brace can help support and stabilize your ankle.
- Immobilization: To immobilize your foot and relieve pressure on your tendons so they can heal, you may need to wear a soft cast or boot.
- Medication: NSAIDs, or non-steroidal anti-inflammatory drugs, can lessen inflammation and pain. In certain situations, your doctor may advise injecting steroids into the tendon sheath, which surrounds the tendon.
- Physical therapy: To help you regain the strength and flexibility in your feet, physical therapists lead you through stretches and exercises.
For muscle strains and injuries, physicians frequently advise starting treatment with the RICE method. The RICE method entails:
- Rest – Make every effort not to move the aching muscle. Sleep enough to allow your body to heal itself.
- Cold therapy – Ice should be applied to the affected area to reduce pain and inflammation. Use a thin towel to cover the ice to avoid skin burns from the ice.
- Compression – Use a medical bandage to compress the injured area to lessen swelling. To prevent stopping the blood supply, avoid wrapping the leg too tightly. Loosen the bandage if the area is tingly, feels cold, or looks blue.
- Elevation – Keep the leg above the heart as much as possible to minimize bruising and pain.
Medical management of Peroneal Tendonitis
The main goals of treatment are to alleviate pain, improve mechanics, and get the patient back to the level of active engagement they want. Non-steroid anti-inflammatory drugs (NSAIDs) can be used to treat patients with peroneal tendinitis, and their activity levels can be lowered to reduce discomfort. The use of corticosteroids is not supported by evidence. Additionally, mild cases of peroneal tendinitis can be managed with the use of lateral heel wedges.
An open tenosynovectomy is advised if Non-operative treatment is ineffective or fails after three to six months. Following surgery, patients are not allowed to bear weight for the first two weeks. After that, they are put in a boot or short-leg weight-bearing cast. Exercises for a range of motion and strengthening (eccentric exercise) are initiated.
Surgical treatment of Peroneal Tendonitis
Surgery might be necessary if conservative measures for peroneal tendonitis don’t work. During a procedure known as a synovectomy, the damaged outer layers of tissue from your peroneal tendons are removed. A minimally invasive synovectomy, which requires fewer incisions and a quicker recovery, may be appropriate for some patients.
Risk of surgery for Peroneal Tendonitis Ankle surgery for peroneal tendonitis carries some risks, just like any other surgery: Sickened. Blood clots. infection. damage to nerves. Ankle pain or recurring tendinitis. formation of scar tissue.
Physiotherapy Treatment of Peroneal Tendonitis
Exercises in peroneal Tendonitis
A program of proprioceptive and balancing exercises, stretching, strengthening, mobilization, and manipulation, as well as icing, ankle bracing, or taping during contact sports, are all part of the treatment for peroneal tendonitis. A cast or ROM boot immobilization is recommended for ten days if the symptoms are severe. Following the resolution of symptoms, the patient starts a progressive rehabilitation program and gradually increases their level of activity.
Ankle strengthening
Resistance band strengthening for the ankle: You can strengthen your ankle by using a resistance band. Ten to fifteen repetitions of each movement, including eversion (turning outward), inversion (turning inward), plantar flexion (bending the ankle away from the body), and dorsiflexion (flexing upward), may be done.
Ankle circles or ankle alphabet
You can do gentle range-of-motion exercises by using your ankle and toes to draw the alphabet.
Stretching your calf
Involves pulling your foot and ankle up towards your shin using a strap or towel. You can hold each stretch for thirty seconds and perform three repetitions of it.
Eccentric Strengthening of the calf muscle
Contracting (tightening) a muscle while it is growing longer is known as eccentric strengthening. If eccentric strengthening exercises are not performed correctly, they can lead to Achilles tendon damage. They should initially be carried out under a physical therapist’s supervision. The exercises can then be performed at home after being mastered by a therapist. These exercises may hurt a little, but not too much.
Strengthening of Toe Extensors
This exercise is excellent for helping the foot and ankle regain their balance. Place your injured foot flat on top of a chair or bench while facing away from it. After that, move your weight forward and bend your knee to align it with your toes. Align your knee with the front of your big toe if your flexibility permits it. Next, raise all five toes towards the ceiling while maintaining the ball of your foot on the ground. maintain the position for up to 6 seconds. Ensure that you are raising all of your toes at once, not just the big toe.
Repeat two to three sets of ten to fifteen repetitions.
Towel toe scrunches

To better support the ankle, this will strengthen the muscles in the feet. With a hand towel folded out beneath your feet, take a seat in a chair. Lay your feet flat over the towel at hip width from the floor. Next, try to scrunch up the towel and bring it closer to you by curling your toes under. Once you run out of towels to move and repeat, keep scrunching.
Twist your toes up to thirty times in two sets a day.
Exercises for Balance
Enhancing your ankle and foot stability can be achieved by putting your balance to the test. You can start with more focused functional moves or just stand on one foot. Balance and add a foam pad for an added challenge.
Bilateral heel drop
Place only the front half of your foot on the stair as you stand at the edge of a stair or stable raised platform. Your heel can go up and down in this position without running afoul of the stairs. To avoid falling and getting hurt, you must take care to make sure you are balanced correctly. Be with someone who can give support or hold something so that you can not lose balance.
Exercises for single-leg balance
These may be recommended if reduced proprioception and balance are discovered. Stand on one foot and maintain your balance for fifteen seconds to accomplish this. Try closing your eyes and maintaining your balance if that’s not too difficult. Try standing on one foot on a folded towel or pillow for an added challenge.
Marching on a foam pad

All you have to do is march steadily in place on a softer surface, like grass or a foam pad, to strengthen your lower leg and get ready for more intense exercises like jumping and running. Make sure you are balanced before stepping onto the foam pad and marching into position on top of it. You can raise the height at which you march to further strengthen your upper legs. Continue for a minute. two to three times
Hopping Exercises and Plyometrics
Exercises involving plyometrics include hopping and jumping. If you intend to resume competitive sports, they might be suggested. To try these, your rehab has to have advanced to the point where your lateral ankle pain is either non-existent or very minimal.
Running and jumping put your ankle under high-velocity forces, which these exercises help it withstand. A few possible exercises are lateral hops, jumping up to and lowering to different boxes.
To ensure you perform the appropriate exercises for your condition, consult your physical therapist before beginning any peroneal tendonitis exercise program. In addition, your therapist can advise you on the safety of exercising.
Risk of exercises
A person must gradually introduce exercise and stretching while they are healing from peroneal tendonitis. One runs the risk of aggravating peroneal tendon damage if one undertakes this exercise too soon or takes on too much too soon.
A person recovering from peroneal tendonitis should talk to their doctor or physical therapist before adding any stretches or exercises to their daily regimen.
Benefits of exercises
Enhancing the tendon’s elasticity and range of motion can be achieved by stretching it. Stretching may therefore aid a person in regaining any motion they may have lost as a result of the injury.
Exercises targeting the peroneal muscles can help strengthen and enhance the area after the resting phase of recovery. To stabilize the area and lower the chance of further injury, calf and ankle exercises and stretches may be helpful.
Electrotherapy
Ultrasound and electric stimulation machines may help with this condition. In physical therapy, ultrasound is a deep heating modality that is occasionally used to warm tissues and increase blood flow. There is a lack of comprehensive research on the application of ultrasound for tendon issues. A lot of therapists steer clear of it since it hasn’t shown any results.
In the physical therapy clinic, electrical stimulation may be utilized to help reduce pain and enhance your ankle’s range of motion. To block painful signals from your lateral ankle to your brain, your physical therapist will place tiny electrodes on your body and use electrical signals.
Additionally, local blood flow to the muscles and tendons may be enhanced by electrical stimulation. Research indicates that electrical stimulation does not improve functional outcomes when compared to not using it, even though some therapists use it to treat peroneal tendonitis.
Orthotics

One of the conditions that could be the cause of your peroneal tendonitis is a collapsed arch or bad foot posture. In this situation, your physical therapist might recommend orthotics or shoe inserts.
Either off-the-shelf or custom-molded orthotics are possible. They are made to support the arch of your foot and maintain its natural position when you run or walk.
Tapping

Taping Kinesiology tape, also known as K-tape, can help your peroneal tendons and muscles work better and lessen lateral ankle pain. This is a relatively new method of taping that improves ankle motion in general. There is a lack of research on K-tape’s application for peroneal tendonitis.
Massage

1. Golf Ball Massage – Use a golf ball or any other hard, round object for this exercise. The foot’s tense muscles will become less so after the massage. To carry out the task: Take a chair. Lay the ball under the foot’s arch on the ground. Maintaining pressure as you slowly apply your weight to the ball, roll it forward and backward. Give your feet one or two more minutes of massage therapy. Carry out the same action using the opposite foot.
Deep tissue friction massage – To increase peroneal tendon mobility on the lateral side of your ankle, your therapist might apply soft tissue massage techniques. Before stretching and exercise, massage can help increase circulation and tissue elasticity. It can also be used to increase general mobility.
Ice massage
- Step 1 Put a paper cup in the freezer after filling it to ¾ full with water.
- Step 2: Peel off the paper cup’s top after the ice has fully frozen.
- Step 3: Apply ice to the sore foot or ankle region and massage it for five minutes, or until the area becomes numb.
- Once more, even though an ice massage can provide temporary relief from tendonitis pain, it’s crucial to have a specialist examine your ankle and foot if you think you may have a long-term injury. Make sure your tendon feels flexible by lightly stretching it after icing.
- Restart your training with a slower, more methodical progression of distance and load once you’ve lessened the tendinitis in your ankles or feet.
Biomechanical ankle platform (BAPS).
Acupuncture, extracorporeal shock wave therapy (ESWT),
Tendinopathy is treated with acupuncture, extracorporeal shock wave therapy (ESWT), and other methods. However, the evidence from studies supporting these treatments is quite weak.
Manual therapy in peroneal tendonitis
There is proof in favor of manual therapy, with the lateral calcaneal glide in particular: The patient lies on their left side with their left calcaneus hanging over the table to mobilize it. The therapist glides from the medial to the lateral side (in the transversal plane) while holding the foot in a neutral position and stabilizing the talus.
Activity modification in the peroneal tendonitis
Steering clear of activities that cause pain in your lateral ankle is one of the most crucial things you can do to treat your peroneal tendonitis. If you experience pain when running, stop for a few weeks. Select a different kind of exercise, such as swimming or biking, that could be less tension in muscles.
You must participate actively in your rehabilitation. Collaborate closely with your physical therapist to make sure you understand the various prescribed treatments and how to perform them, as well as to ensure you perform the appropriate exercises for your condition.
The first step in a successful treatment plan is to control the inflammation. The next step is to determine the maximum weight your peroneal tendons can support and gradually increase your load tolerance.
Duration of treatment in the peroneal tendonitis
For peroneal tendonitis, physical therapy treatments typically last three to six weeks. Depending on the severity of your condition and any comorbidities (other medical conditions you may have), your experience may vary slightly.
That being said, your peroneal tendons should heal completely in an average of six weeks. It should have also become clear to you how to prevent the pain from coming again.
Make sure you discuss your particular situation and comprehend the prognosis (results) for your peroneal tendonitis with your physical therapist. Should your discomfort persist, you might have to see an orthopedic surgeon for more invasive treatments such as peroneal tendon surgery or cortisone injections.
Prevention of the Peroneal Tendonitis
Here are some suggestions to avoid peroneal tendon pain:
- Increase your level of physical exertion gradually.
- Never ignore pain in your ankles or feet.
- Give up smoking.
- Take breaks from exercises, games, or other physical activities.
- To warm up your ankles and feet before engaging in physical activity, stretch.
- Put on supportive shoes, ankle braces, or other suitable safety gear.
- If your arches are high, wear orthotics, but only if your doctor advises you to.
Prognosis
The majority of people get well from this illness in around a month. Consult your healthcare provider before returning to your sport or full activities. If you require surgery for peroneal tendonitis, your recovery period will be prolonged. Your lower leg will be in a cast for four to six weeks following surgery. During the first few weeks, crutches might also be necessary. When it’s okay for you to resume bearing weight on your ankle, your provider can advise you. After surgery, the majority of patients require physical therapy to regain ankle strength and stability.
Summary
Inflammation in the tendons that run along the side of your foot and your outer ankle bone is known as peroneal tendonitis. The muscles in your lower leg and the bones in your foot are joined by these strong bands of tissue.
They shield your ankle and foot from injury while assisting with balance and stabilization. Usually brought on by overuse, this kind of tendonitis in the feet can also develop suddenly from a fall or other foot injury.
FAQs
If you follow the recommended advice, the majority of people with peroneal tendinopathy will see improvement in their symptoms within three months; however, for some people, the symptoms may not improve for up to a year.
You might be able to walk pain-free if your illness is not too severe.
Avoiding the afflicted foot and stopping intense exercise
Even though they usually heal on their own, there is a chance that the nerve will be permanently damaged.
References
- Professional, C. C. M. (n.d.-j). Peroneal tendonitis. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/22003-peroneal-tendonitis
- Pt, B. S. (2021, September 16). Physical therapy for peroneal tendonitis. Verywell Health. https://www.verywellhealth.com/physical-therapy-for-peroneal-tendonitis-5114651#toc-pt-for-peroneal-tendonitis
- Guide | Physical Therapy Guide to Peroneal Tendinopathy. (2019, December 17). Choose PT. https://www.choosept.com/guide/physical-therapy-guide-peroneal-tendinopathy
- Morales-Brown, L. (2020, September 22). Stretches and exercises for peroneal tendonitis. https://www.medicalnewstoday.com/articles/peroneal-tendonitis-exercises#risks
- Vive Health. (n.d.). Peroneal tendonitis exercises to try at home. https://www.vivehealth.com/blogs/resources/peroneal-tendonitis-exercises
- Peroneal tendon problems. (n.d.). https://www.sportsrehabu.com/Injuries-Conditions/Ankle/Ankle-Issues/Peroneal-Tendon-Problems/a~123/article.html
- Martin, & Martin. (2023, May 3). Relieve ankle and foot tendonitis | Midwest Orthopedic Specialty Hospital. Midwest Orthopedic Specialty Hospital. https://www.mymosh.com/physical-therapy/ankle-and-foot-tendonitis-exercises/