Chondromalacia Patellae (CMP)
Chondromalacia patellae (CMP) is referred to as anterior knee pain due to the physical and biomechanical changes. The articular cartilage of the posterior surface of the patella is going though degenerative changes which manifest as a softening, swelling, fraying, and erosion of the hyaline cartilage underlying the patella and sclerosis of the underlying bone.
Chondromalacia patellae is one of the most frequently encountered causes of anterior knee pain among young people. It’s the number one cause in the United States with an incidence as high as one in four people. The word chondromalacia is derived from the Greek words – chrondros, meaning cartilage, and malakia, meaning softening. Hence chondromalacia patellae is a softening of the articular cartilage on the posterior surface of the patella which may eventually lead to fibrillation, fissuring, and erosion.
The differential diagnosis of chondromalacia includes patellofemoral pain syndrome and patellar tendinopathy. Chondromalacia is not considered to be under the umbrella term of PFPS. The pathophysiology is thought to be different and therefore there is an alternative treatment.
Table of Contents
Symptoms of Chondromalacia Patellae
- Chondromalacia patella symptoms (patellofemoral syndrome) include a vague discomfort of the inner knee area, aggravated by activity (running, jumping, climbing, or descending stairs) or by prolonged sitting with the knees in a moderately bent position.
- Some people with chondromalacia patella may also have a vague sense of tightness or fullness in the knee area, particularly if the knee becomes swollen.
- Occasionally, if chronic symptoms are ignored, the associated loss of quadriceps (thigh) muscle strength and bulk may cause the leg to weaken.
Causes of Chondromalacia Patellae
Chondromalacia patellae occurs most often in young adults and teenagers. It is more common in women. The reason why damage occurs to the cartilage is not clear. It is thought that the kneecap (patella) may rub against the lower part of the thigh bone (femur) instead of gliding smoothly over it. This may damage the patellar cartilage. Situations where this is more likely include the following:
- Overuse of the knee, such as in certain sports.
- Some people may have a slight problem with the alignment of the knee. This may cause the patella to rub on, rather than glide over, the lower femur. It may be due to the way the knee has developed. Or, it may be due to an imbalance in the muscles around the knee – for example, the large quadriceps muscle above the knee. If one side of the quadriceps muscles pulls harder than the other side, the patella may not glide smoothly and may rub on one side.
- A combination of an alignment problem (as above) and overuse with sports, may be the most common reason for developing chondromalacia patellae.
- Injury to the knee may contribute – perhaps repeated small injuries or stresses due to sports, or due to slack ligaments (hypermobile joints).
- In older people it may develop as part of the ageing process where there is wear and tear of cartilage in many joints.
Risk Factors of Chondromalacia Patellae
There are a variety of factors that may increase your risk for developing chondromalacia patellae.
- Age: Adolescents and young adults are at high risk for this condition. During growth spurts, the muscles and bones develop rapidly, which may contribute to short-term muscle imbalances.
- Sex: Females are more likely than males to develop a runner’s knee, as they typically possess less muscle mass than males. This can cause abnormal knee positioning, as well as more lateral (side) pressure on the kneecap.
- Flat feet: Having flat feet may place more stress on the knee joints than having higher arches would.
- Previous injury: A prior injury to the kneecap, such as a dislocation, can increase your risk of developing a runner’s knee.
- High activity level: If you have a high activity level or engage in frequent exercises that place pressure on your knee joints, this can increase the risk for knee problems.
Arthritis: Runner’s knee can also be a symptom of arthritis, a condition causing inflammation to the joint and tissue. Inflammation can prevent the kneecap from functioning properly.
Preventions of Chondromalacia Patellae
You can help reduce your risk of developing runner’s knee by following these recommendations:
- Avoid repeated stress to your kneecaps. Wear knee pads if you have to spend time on your knees.
- Create muscle balance by strengthening your quadriceps, hamstrings, abductors, and adductors.
- Wear shoe inserts that correct flat feet by increasing your arch. This will decrease the amount of pressure placed on your knees and may realign the kneecap.
Finally, excess body weight may stress your knees. Maintaining a healthy body weight can help take pressure off the knees and other joints. You can take steps to lose weight by reducing your sugar and fat intake, eating plenty of vegetables, fruits, and whole grains, and exercising for at least 30 minutes a day, five times a week.
Diagnosis of Chondromalacia Patellae
The patient’s posture can be an initial clue as well as any observed asymmetries, such as; limb alignment in standing, internal femoral rotation, anterior or posterior pelvic tilt, hyperextended or ‘locked back’ knees, genu varum or valgum and abnormal pronation of the foot. Gait patterns may also be affected.
Mobility and range of motion (ROM) of the joint are tested, which can be limited. If bursitis is present, passive flexion or active extension will be painful. Loss of power in the affected leg may also be present on isometric testing. There are specific tests for anterior knee pain syndrome:
- Patellar grind test or Clarke’s sign: This test detects the presence of patellofemoral joint disorder. A positive sign on this test is pain in the patellofemoral joint.
- Compression test
- Extension-resistance test: This test is used to perform a maximal provocation on the muscle-tendon mechanism of the extensor muscles and is positive when the affected knee demonstrates less power when trying to maintain the pressure.
- The critical test: This is done with the patient in high sitting and performing isometric quadriceps contractions at 5 different angles (0°, 30°, 60°, 90° and 120°) while the femur is externally rotated, sustaining the contractions for 10 seconds. If pain is produced then the leg is positioned in full extension. In this position, the patella and femur have no more contact. The lower leg of the patient is supported by the therapist so the quadriceps can be fully relaxed. When the quadriceps is relaxed, the therapist is able to glide the patella medially. This glide is maintained while the isometric contractions are again performed. If this reduces the pain and the pain is patellofemoral in origin, there is a high chance of a favourable outcome.
It is possible to diagnose incorrectly and these tests may aid in determining chondromalacia, but other possible conditions also need to be excluded.
A doctor will perform a physical examination of the knee to determine the cause of pain. If the diagnosis is not clear or symptoms do not improve a doctor may order one of the following:
- Blood tests and/or a standard knee X-ray: This may help to rule out some types of arthritis or inflammation.
- MRI scan: A test that shows details of the knee joint and can reveal many cases of chondromalacia patella.
- Arthroscopy: A tiny, flexible camera is inserted into the knee to see exactly what the cartilage looks like.
Grading of Chondromalacia Patellae
There are four grades, ranging from grade 1 to 4, that designate the severity of a runner’s knee. Grade 1 is least severe, while grade 4 indicates the greatest severity.
- Grade 1 severity indicates softening of the cartilage in the knee area.
- Grade 2 indicates a softening of the cartilage along with abnormal surface characteristics. This usually marks the beginning of tissue erosion.
- Grade 3 shows thinning of cartilage with active deterioration of the tissue.
Grade 4, the most severe grade, indicates exposure of the bone with a significant portion of cartilage deteriorated. Bone exposure means bone-to-bone rubbing is likely occurring in the knee.
Treatment of Chondromalacia Patellae
- Avoid strenuous use of the knee: until the pain eases. Symptoms usually improve in time if the knee is not overused.
- Painkillers: paracetamol may be advised to ease the pain. Anti-inflammatories such as ibuprofen may be helpful for pain in the short term but there is no evidence that they provide any long-term benefit.
- Physiotherapy: improving the strength of the muscles around the knee will ease the stress on the knee. Also, specific exercises may help to correct problems with alignment and muscle balance around the knee. For example, you may be taught to do exercises which strengthen the inner side of the quadriceps muscle.
- Taping of the kneecap (patella): is a possible treatment which can reduce pain. Adhesive tape is applied over the patella, to alter the alignment or the way the patella moves. Some people find this helpful. Some physiotherapists can offer patellar taping treatment.
- Icing: Ice may be useful for reducing pain in an acute flare-up, but not as a long term treatment protocol.
Surgery for Chondromalacia Patellae
Surgery is not usually necessary but it may be advised if the above treatments have not helped. Arthroscopic surgery is the usual operation. A tiny flexible camera is inserted into the knee. The surgeon sees the inside of the knee joint and the cartilage, and may then operate through the camera tube, using very fine instruments. Possible surgical treatments are as follows:
- Tight ligaments on the side of the patella may be cut to allow the patella to align better and move more smoothly.
- Smoothing or shaving the cartilage behind the patella.
- Rarely, if all other options do not help, the patella can be removed (the knee can still function without it).
Exercises for Chondromalacia Patellae
Conservative treatment of chondromalacia patellae is both physical and highly advised. Short-wave diathermy can help to relieve pain and to increase the blood supply to the area, improving nutrition supply to the articular cartilage. Care must be taken when planning an exercise programme. Conservative therapeutic interventions include the following:
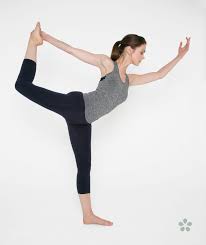
- Isometric quadriceps strengthening and stretching exercises Restoration of adequate quadriceps strength and function is an essential factor in achieving good recovery. The most effective exercises are isometric and isotonic in the inner range. Isotonic exercises through a full range of motion will only lead to increased pain and even joint effusion. Stretching of the vastus lateralis and strengthening of the vastus medialis is often recommended, but they are difficult to isolate due to shared innervation and insertion. It has shown that closed kinematic chain exercises can improve patellofemoral joint performance by increasing quadriceps muscle strength and patellar alignment correction.
- Hamstring stretching exercises
- Temporary modification of activity
- Patellar taping
- Foot orthoses
- NSAIDs
- Hip strength and stability training, as hip positioning and strength have a significant influence on anterior knee pain.
- Hip abductor strengthening as an increased hip adduction angle is associated with weakened hip abductors.
- Patellar realignment brace
Not only is strengthening important, but stretching should also be part of the programme. It has been shown that patients with patellofemoral pain syndrome have shorter and less flexible hamstrings than asymptomatic individuals.. Although stretching can improve flexibility and knee function, it doesn’t necessarily directly improve pain.
Another form of therapy is warm needling. In combination with rehabilitation exercises, it has a prolonged pain-relieving effect than in warm needling in combination with medication.
Taping and Braces for Chondromalacia Patellae
Taping the patella to influence its movement may provide some short term relief, but the evidence is varied. A commonly used technique is ‘McConnell taping or kinesio taping’.
Supporting the patella and knee joint by bracing is a further way to reduce pain and symptoms, but it will also alter patella tracking and reduce active function of the quadriceps. Bracing may be useful in the short term to offer patients some support and pain relief to help them avoid antalgic movements and normalise gait as much as possible. Bracing can also be used for patients pre- and postoperatively, but a brace should allow variation in medial pull on the patellar and pressure. Wearing a patellar realignment brace and following physical therapy has a synergistic effect on patients with chondromalacia patellae.




One Comment