Ankylosing Spondylitis (AS)
Ankylosing spondylitis (pronounced ankle-oh-sing spon-dill-eye-tiss) is a form of arthritis that causes chronic (long-term) spine inflammation. Ankylosing spondylitis (AS) inflames the sacroiliac joints located between the base of the spine and pelvis. This inflammation, called sacroiliitis, is one of the first signs of Ankylosing spondylitis. Inflammation often spreads to joints between the vertebrae, the bones that make up the spinal column. This condition is known as spondylitis.
Some people with Ankylosing spondylitis experience severe, persistent back and hip pain and stiffness. Others have milder symptoms that come and go. Over time, new bone formations may fuse vertebrae sections together, making the spine rigid. This condition is called ankylosis.
Ankylosing spondylitis belongs to a group of diseases known as spondyloarthropathies. Between three and 13 out of 1,000 Americans have one of these diseases.
Anyone can get Ankylosing spondylitis, although it affects more men than women. Symptoms usually appear in people between the ages of 17 and 45. Ankylosing spondylitis has a genetic link and may run in families.
Table of Contents
Symptoms of Ankylosing Spondylitis
The symptoms of ankylosing spondylitis vary. Like other forms of arthritis, it typically features mild to moderate flare-ups of inflammation that alternate with periods of almost no symptoms.
The most common symptom is back pain in the morning and at night. You may also experience pain in the large joints, such as the hips and shoulders. Other symptoms may include:
- early morning stiffness
- poor posture or stooped shoulders
- loss of appetite
- low-grade fever
- weight loss
- fatigue
- anemia or low iron
- reduced lung function
Because ankylosing spondylitis involves inflammation, it can affect other parts of the body as well. If you have ankylosing spondylitis, you may also experience:
- inflammation of the bowels
- eye inflammation
- heart valve inflammation
- plantar fasciitis and Achilles tendinitis
You should see your doctor if you experience severe or recurring joint pain or if the pain interferes with your daily life. If a primary care doctor suspects ankylosing spondylitis, they may refer you to a rheumatologist. Rheumatologists are experts in arthritis and other muscular and skeletal disorders.
Causes
Ankylosing spondylitis has no known specific cause, though genetic factors seem to be involved. In particular, people who have a gene called HLA-B27 are at a greatly increased risk of developing ankylosing spondylitis. However, only some people with the gene develop the condition.
Complications of Ankylosing Spondylitis
Ankylosing Spondylitis can cause pain and inflammation throughout your body, including in your:
- Spine: In rare cases, your vertebrae may become weak, making them more likely to fracture or break. Damaged vertebrae can press on or irritate a group of nerves in the bottom of your spinal cord called the cauda equina. You might have trouble controlling your bowels or bladder, sexual problems, or a loss of reflexes
- Eyes: About 40% of people with AS have an eye problem called uveitis. It’s a kind of eye inflammation that’s painful and can blur your vision and make you sensitive to bright light. If you have uveitis, your doctor might check for AS even if you don’t have any other symptoms
- Heart valve: Rarely, AS can enlarge your aorta, the largest artery in your body. This can change the shape of your aortic valve, allowing blood to leak back into your heart. Your heart won’t pump as well, which can leave you tired and short of breath
People with AS are also more likely to get certain types of cancers. They include bone and prostate cancers in men and colon cancer in women, as well as blood-related cancers in both sexes.
Risk Factors of Ankylosing Spondylitis
Family history
A family history of ankylosing spondylitis is a risk factor, along with the presence of the HLA-B27 protein. More than 90% of people with this condition have the gene that expresses this protein.
Age
Unlike other arthritic and rheumatic disorders, initial symptoms of ankylosing spondylitis often appear in younger adults. Symptoms often appear between ages 20 and 40.
Sex
Some guidance states that ankylosing spondylitis is around twice as common in males than females. However, the actual prevalence of the condition may be more even, according to a 2018 review.
Ankylosing spondylitis symptoms can differ between males and females, which may lead to a late or missed diagnosis.
Preventions
It’s not known how you can prevent ankylosing spondylitis because no one knows what causes it in the first place. However, if you have the disease, you can focus on preventing disability by:
- staying active
- eating a nutrient-dense diet
- maintaining a moderate weight
These health-promoting lifestyle approaches, coupled with traditional treatments, may help delay or slow disease progression.
Diagnosis of Ankylosing Spondylitis
Symptoms of ankylosing spondylitis can be similar to more common back problems, especially in the early stages.
Because of this, many people put up with the pain for some time before seeking help. It’s important to see a doctor as soon as possible if you suspect you have ankylosing spondylitis.
It’s usually diagnosed by a rheumatologist, these are doctors who specialise in conditions affecting the joints, bones and muscles.
There is no one test that can show for certain that you have ankylosing spondylitis. A diagnosis will be made based on several things, including:
- History: the history of your condition and the symptoms you’ve experienced, including whether pain and discomfort is waking you up during the second half of the night
- Physical Examination: a physical examination done by the doctor
- Blood tests: this may show inflammation
- Imaging: x-rays or a magnetic resonance imaging (MRI) scan
- Age: It can be diagnosed at any age, but most often begins before the age of 40, and often much younger
There are disease activity and pain scores that can help doctors diagnose ankylosing spondylitis. Your doctor will ask if you have key symptoms, such as swollen and painful joints, especially around the spine, and fatigue. You’ll be asked if you have pain in the mornings and how long for. Your answer to these questions could help lead to a diagnosis.
Blood tests can confirm whether you have the HLA-B27 gene. Most people with ankylosing spondylitis test positive for HLA-B27, but so do many people who don’t have the condition. A positive test may point to someone having ankylosing spondylitis, but it won’t confirm the diagnosis.
Treatment of Ankylosing Spondylitis
There’s no current cure for ankylosing spondylitis, but treatment can help manage pain and prevent disability. Timely treatment may also slow or even stop possible complications, such as bone deformity.
Medications
Doctors may prescribe a range of medications to treat ankylosing spondylitis. Which medications a person receives will depend on the progress and severity of their condition.
- NSAIDs: Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, are often used to help manage pain and inflammation. They’re generally safe with few complications
- Corticosteroids: Corticosteroids are powerful inflammation fighters that can ease symptoms and slow damage around the spine, but it cannot be used long term
- Biologics: Tumor necrosis factor (TNF) and IL-17 inhibitors are drugs that can block inflammation triggers in your body. These drugs act to prevent inflammation, and they may ease joint pain and stiffness
- DMARDs: Your doctor may also prescribe disease-modifying antirheumatic drugs (DMARDs). These drugs work to slow the process of the disease in the body to prevent worsening symptoms
Surgery
If you have severe damage or deformity to your knee or hip joints, joint replacement surgery may be necessary. Likewise, people with poor posture from fused bones may require an osteotomy. During this procedure, a surgeon will cut and realign the bones in the spine.
Treatment relies largely on how severe the condition is and how troublesome the symptoms are.
Natural Remedies
In addition to more traditional medical treatments, some natural remedies may help ease symptoms of ankylosing spondylitis. A person may often use these alongside prescribed treatment plans. Talk with your doctor about which ones are safe to use together and which are best for you.
Exercises: Daily exercise and posture practice can help you maintain flexibility and range of motion. Each of these exercises may help reduce symptoms of ankylosing spondylitis:
- yoga
- deep breathing
- stretching
- swimming
- posture practices
These practices may be part of a holistic treatment plan that includes medication and physical therapy.
Stretching: Stretching can make your joints more flexible and improve strength. This can lead to less pain and a better range of motion in your joints.
Posture Training: Stiffness in the spine may encourage bad posture. Over time, bones in the spine can fuse together in slouching or slumping positions. You can reduce the risk of this by practicing good posture. Because this may not come naturally after years of poor posture positions, you may need to encourage better posture with reminders to correct your posture regularly. You can also use support devices, such as ergonomic support chairs or seat cushions.
Heat and Cold therapy: Heating pads or a warm shower can help ease pain and stiffness in the spine and other affected joints. Ice packs can reduce inflammation in painful or swollen joints.
Acupuncture: This alternative treatment may help reduce pain and other symptoms of ankylosing spondylitis. It does so by activating natural pain-relieving hormones.
Massage Therapy: In addition to being relaxing and invigorating, massage can help you maintain flexibility and improve your range of motion. Be sure to tell your massage therapist that you have ankylosing spondylitis. They can be aware of tender points around your spine.
Many treatments for ankylosing spondylitis are also smart practices for a healthier life.
Bracing
Depending on how spondylosis affects the parts of your spine, it may cause spinal instability. That means that the parts of your spine aren’t working properly to control your movements. With an unstable spine, you’re more at risk for neurological injury (injury to the nerves). To address this instability, your doctor may recommend you wear a brace for a while.
Bracing is a temporary treatment option for spondylosis, one more often used for spondylosis in the neck (cervical spine). Braces can, however, also be used for spondylosis in other regions of the spine, such as the low back (lumbar spine). A brace will help control your pain by limiting motion. Braces also help support your spine, taking some of the pressure off your vertebrae. Additionally, braces can help the muscles relax, and that relaxation alone can provide a level of pain relief.
Long-term bracing isn’t usually recommended because it can cause the spinal muscles to weaken. It’s better for you to go to physical therapy to learn how to strengthen your muscles so that they better support your spine.
Your doctor will decide if bracing is a good option for you, what kind of brace you should wear, and how long you’ll need to wear it. With a brace, it’s absolutely critical that you follow the doctor’s order exactly for how and when you’re supposed to wear it. If you don’t, the brace won’t be as effective at relieving your pain and providing support.
Exercises for Ankylosing Spondylitis
Press Up to Stretch Your Spine
Ankylosing spondylitis (AS) can shorten the spine and muscles in your back. Stretch with this move to help “rounded” back and back pain. Lie on your stomach with your legs behind you. Slowly prop yourself up on your elbows so your chest is off the ground. If you’re able, straighten your arms. Hold for 10 to 20 seconds. Repeat 3-5 times. Do this move once a day.
Wall Sit for Better Posture
Stand with your back against a wall. Put your feet shoulder-width apart, and away from the wall. Slowly slide your back down the wall. It may take time, but work towards being able to get to the point where your thighs are parallel with the floor, like you’re sitting in a chair. Hold for 5 to 10 seconds. Hold for longer as you get stronger. Repeat 3-5 times. Do 3 to 5 times a week. Exercising muscles that Ankylosing Spondylitis affects in your back, shoulders, neck, butt, and hips. This exercise can help you move more easily.
Plank for a Stronger Core
To make sure you’re strong enough for this exercise, start in a standing position with your feet flat on the floor and your forearms on the kitchen counter. Once you can do that fairly easily, move on to the harder version. Your stomach, back, and butt muscles help your posture. Work them with this move, no crunches needed! Kneel on a mat.
Put your forearms on the ground. Push your legs out behind you and balance on your toes. Squeeze your stomach and butt muscles to hold your body in a straight line. Don’t crane your head up or let it hang down. Keep your neck in line with your spine. Hold for 5 seconds. Repeat 3-5 times. Add more time as you become stronger. Always keep your core tight. Do this 3 to 5 times a week.
Try Standing Leg Raises to Loosen Tight Hips
Hold the back of a chair or railing. Keep your back straight with a slight bend in your knees. Slowly lift one leg out to the side so it’s a few inches off the ground. Then lower it back to the starting position. Next, kick the same leg straight behind you to 45 degrees. Remember to keep good posture. Avoid bending over at the waist. Repeat 10 to 15 times on each leg. Do this move 3 to 5 times a week.
Do Chin Tucks to Stretch Your Neck
Ankylosing Spondylitis can make you lean forward. That can cause your neck to get tight and give you headaches. This move can strengthen your neck to keep you upright and relieve tightness. Lie on your back. Without lifting your head off the floor, tuck your chin in slightly toward your chest. Hold for 5 to 10 seconds. Repeat 3 to 5 times. If you feel uncomfortable, place a rolled-up towel under your neck. Do this stretch twice a day.
Roll Your Shoulders to Loosen Up
Stand or sit up tall. Keep your spine as straight as you’re comfortably able to. Gently shrug your shoulders up toward your ears, then move your shoulders back and down. You can feel this in your upper back. Think about pulling your shoulder blades together and down in a rolling motion. Then pull your shoulders back up toward your ears. Repeat 5 to 10 times. Do this stretch daily.
Stretch Your Hips to Ease Low Back Pain
This lengthens the muscles at the front of your hips. They connect to your lower back. Take a big step forward. Sink into a lunge: Move your back knee down and rest it on the ground. Keep your back upright. Be mindful not to bend forward at the hips. You should feel this stretch in your back leg (the one that is resting on the ground). You’ll feel it on the front of the thigh and hip.
To get a deeper stretch, gently push both your hips forward. Hold for 20-30 seconds. Repeat with your other leg. Hold a chair for balance if needed. Do this stretch daily.
Corner Stretch to Open Your Chest
Find a corner and stand facing it. Raise your arms up. Rest the palms of your hands on the walls. Gently press your chest toward the corner. Your arms will provide tension. You’ll feel the stretch across the front of your chest. Along your back, you’ll feel your shoulder blades move toward each other. Hold for 20 to 30 seconds. Do this stretch daily.
Walk, Move
Exercise can ease pain and inflammation. When you boost your heart rate, it also makes feel-good chemicals in your body. Any exercise is great. But you get a bonus from doing weight-bearing exercise. When your joints have to support your weight, like when you walk instead of swim. It helps “feed” the cartilage in your joints and spine. Get your heart pumping most days of the week. Start with 5 to 10 minutes a day. Try to work up to 30 minutes or more. It’s OK to do 5 to 10 minutes at a time, a few times a day. It adds up!
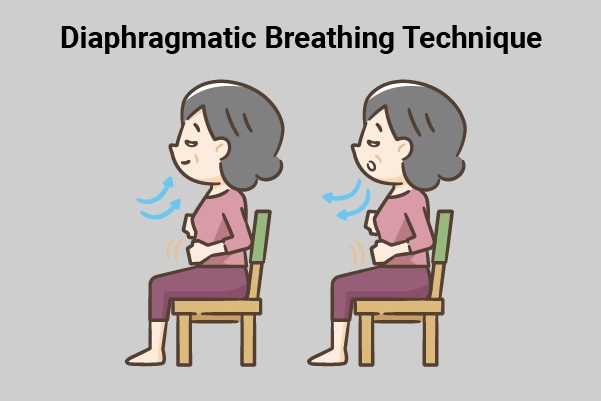
Take Deep Breaths
Many people with AS eventually notice that they have trouble fully extending their ribs and chest while they breathe. But deep-breathing exercises can help prevent this problem. Several times a day, take 3 to 4 deep breaths. Focus on pulling air deep into your chest as you inhale. Then, exhale slowly.







2 Comments