Acute transverse myelitis: Cause, Symptoms, Treatment, Exercise
Table of Contents
What is acute transverse myelitis?
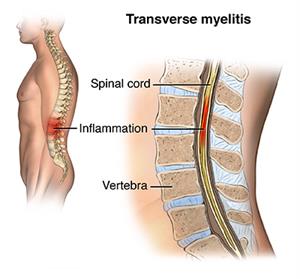
Acute transverse myelitis (ATM) is a rare, acquired neuro-immune spinal cord disorder, which involves a brief but intense attack of acute inflammation(swelling) of white and gray matter in the spinal cord segments, that damages myelin. It is one type of demyelinating disorder, due to it affecting myelin which is the protective covering of nerve fibers. The spinal cord transfers information between the body and the brain. This condition generally affects the middle or thoracic portion of the spinal cord, but it can affect the upper or cervical portion of the spinal cord. It can present with the rapid onset of weakness, bowel or bladder deficits, and motor and sensory alterations below the level of the lesion.
The clinical features, diagnostic criteria, and acute and chronic treatment can change between different forms of Transverse myelitis (TM). It is essential in the evaluation of patients with acute myelopathies to exclude noninflammatory and compressive causes of myelopathy along with to differentiate various types of Transverse myelitis (TM), because of the prognosis, treatment options, and risk of recurrence may differ among all other types.
Most children with acute transverse myelitis (ATM) have a nearly or complete recovery. Acute transverse myelitis (ATM) is related to multiple sclerosis (MS); however, a child with multiple sclerosis (MS) has repeated attacks in both the spinal cord and brain, while acute transverse myelitis (ATM) typically occurs only in the spinal cord and only once.
What are the symptoms of Acute Transverse Myelitis?
There are a lot of variations in the presentation of symptoms of Acute transverse myelitis, which are based on the severity of the damage to the neurons and the myelin in the spinal cord and on the level of the spinal cord affection.
it is called “transverse” because, in this condition, numbness and weakness occur on both sides of the patient’s body.
If the upper or cervical portion of a child’s spinal cord is affected, both upper limbs and lower limbs can be affected, along with, In severe cases, breathing can be affected.
If the middle or thoracic portion of the child’s spinal cord is affected, lower limbs will be affected, but arms will be spared.
This condition occasionally recurs in people with SLE, multiple sclerosis, or antiphospholipid syndrome.
Symptoms of acute transverse myelitis may include:
- Pain in the neck, head, or back
- A band-like tightness around the abdomen or chest
- Weakness in the limbs
- Abnormal feelings in the lower limbs, like tingling, burning or pricking
- Numbness of the legs and feet
- loss of bladder and bowel function or difficulty voiding
- Sexual dysfunction
These symptoms of transverse myelitis develop over a few hours to a few days, or over a longer period of 1 to 2 weeks. This condition can progress over a few more days to a complete transverse sensorimotor myelopathy, which causes paraplegia, urinary retention, sensory loss below the level, and fecal incontinence. Frequently, vibration and position sensation is intact, at least in the initial period.
In a few cases, symptoms progress over hours while in other cases, it progresses over days. A neurological function may be reduced during the acute phase in 4 to 21 days, whereas 80% of cases reach their maximal deficit within 10 days of onset of symptoms. At its worst point, 80-94% of patients experience paresthesias, numbness, banding, or girdling, 50% of people have lost all movements of their legs, and almost all people have some degree of bladder dysfunction.
Some patients recover from acute transverse myelitis with no or minor residual problems, however, the healing process can take a few months to years. Some patients suffer permanent impairments that affect their ability to perform daily living ordinary tasks. Most patients have only one episode of this condition, while 10-20%, which is a small percentage can have a chance of recurrence.
What are the causes of Acute Transverse Myelitis?
The exact cause of acute transverse myelitis is unknown. Around fifty percent time, doctors are not sure what causes acute transverse myelitis. However, doctors know it can happen while a person’s body tries to fight a disease or while the immune system of a person attacks healthy cells for any reason.
Bacterial, viral, and fungal infections affect the spinal cord, which can cause acute transverse myelitis. The inflammatory diseases appear after recovery from the infection, in most cases.
Bacterial infections which are associated with acute transverse myelitis may include:
- Syphilis
- Lyme disease
- Actinomyces
- Tuberculosis
- Diphtheria
- Pertussis
- Tetanus
- Bacterial skin infections
- Gastroenteritis
- Bacterial pneumonia
Viral infections which are associated with acute transverse myelitis may include:
- Herpesviruses, including the varicella-zoster, causes shingles and chickenpox (zoster)
- Cytomegalovirus
- Zika
- Epstein-Barr
- Influenza
- HIV
- Enteroviruses like coxsackievirus and poliovirus
- West Nile
- Echovirus
- Mumps, rubella, and measles
- Hepatitis B
- Other viruses can trigger an autoimmune reaction without directly affecting the spinal cord.
- Sometimes, fungal and parasites infections may infect the spinal cord, which causes acute transverse myelitis.
- Fungal infections include:
- aspergillus
- Blastomyces
- coccidiosis
- cryptococcus
- Parasites infections include:
- toxoplasmosis
- cysticercosis
- schistosomiasis
- angtiostrongyloid
Some inflammatory conditions can cause acute transverse myelitis:
- Multiple sclerosis: acute transverse myelitis can be the initial sign of multiple sclerosis or represent a relapse, which usually causes symptoms on only one side of the patient’s body.
- Neuromyelitis Optica (Devic’s disease): acute transverse myelitis associated with this condition generally affects both sides of the patient’s body.
Patients may feel symptoms of damage to the myelin of the optic nerve, which includes temporary vision loss and pain in the eye with movement.
- Autoimmune disorders can affect acute transverse myelitis in a few patients, which include:
- Sjogren’s syndrome causes severe dryness of the eyes and mouth.
- lupus, which affects multiple body systems
- Vaccinations for infectious diseases are sometimes associated as a possible trigger for acute transverse myelitis.
How to diagnose Acute Transverse Myelitis?
A doctor will diagnose acute transverse myelitis based on signs and symptoms of a patient, family, and medical history, test results, and a clinical assessment of nerve function.
These tests indicate inflammation of the spinal cord, which includes:
Magnetic resonance imaging (MRI) uses radio waves and magnetic fields to create 3D images of soft tissues of the body. An MRI can show inflammation and swelling of the spinal cord and other potential causes of the symptoms, including abnormalities affecting the blood vessels or spinal cord.
MRI frequently shows an altered signal in the spinal cord which extends to multiple segments along the spinal cord, suggesting nerve injury in the spinal cord and demyelination, which is a process in which the coating or, myelin, which covers many nerve fibers is stripped off by disease.
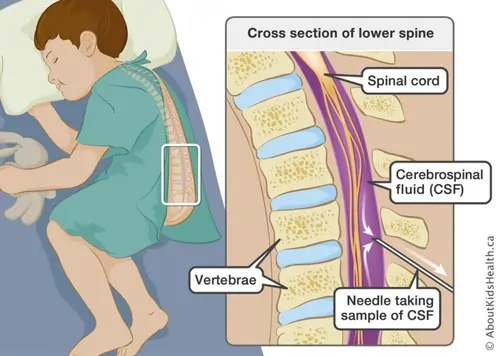
Lumbar puncture or spinal tap is the technique in which the use of a needle draws a small amount of cerebrospinal fluid (CSF), the protective fluid that surrounds the brain and spinal cord.
In some patients with acute transverse myelitis, CSF may have monocytes, abnormally high numbers of white blood cells (WBCs), our immune system proteins that indicate inflammation, and IgG index is elevated, which is normal by ≤ 0.85.
Blood tests include a test that checks for antibodies associated with neuromyelitis optica, a condition in which inflammation occurs both in the nerve in the patient’s eye and in the patient’s spinal cord. People with a positive antibody test are at higher risk of having multiple attacks of acute transverse myelitis and it requires possible treatment to prevent future attacks of transverse myelitis.
Other blood tests may recognize infections that may cause acute transverse myelitis, or rule out other reasons for symptoms.
Tests for treatable causes include:
- PPD (purified protein derivative) for tuberculosis
- Chest x-ray
- Serologic tests for Lyme disease, mycoplasma, and HIV
- Erythrocyte sedimentation rate (ESR)
- Antinuclear antibodies
- Blood and CSF Venereal Disease Research Laboratory (VDRL) tests
What is the Prognosis for Acute Transverse Myelitis?
Most patients with transverse myelitis have at least partial or half recovery, which may take a year or more. Most of the recovery of the patient occurs within the initial 3 months after the episode of transverse myelitis, and it strongly depends on the cause of transverse myelitis.
About one-third of a patient with transverse myelitis are in one of three categories after an attack of the condition, which includes:
(1) No or slight disability: These patients experience only minimal lingering symptoms or maybe recover.
(2) Moderate disability: These patients are mobile, but may have difficulty in walking, tingling or numbness, and bladder and bowel problems such as urinary urgency.
(3) Severe disability: Some patients are bed-bound and incontinent or may permanently need a wheelchair and require ongoing assistance with daily living activities and care.
It is hard to give a prediction of the course of acute transverse myelitis. The responsiveness to treatment and prognosis is strongly given by the cause of the condition and to some extent by how early and fast treatment is started. In general, patients who experience a rapid onset of severe symptoms and signs and patients who have a positive test for a particular antibody can have a worse prognosis than patients with comparatively milder symptoms, slower onset, and negative antibody test.
In about 10 to 20% of patients, in whom the cause is unknown initially, in that multiple sclerosis develops eventually.
What is the medical treatment for ATM?
Several therapies and medicines mainly target the acute symptoms and signs of acute transverse myelitis:
Intravenous steroids: Patients may receive steroids through a vein in their arm over a period of a few days, which helps in reducing the inflammation in the spinal column.
Intravenous immunoglobulin (IVIG): The doctor injects antibodies from healthy donors into a system of patients. Antibodies will bind to the patient’s antibodies, which cause the problem and remove them from circulation.
Plasma exchange therapy: It is also called plasmapheresis. Patients who don’t respond to intravenous steroids and If steroids don’t lower inflammation, they may need plasma exchange therapy. This therapy includes removing the straw-colored fluid in which blood cells are suspended (plasma, the liquid part that holds the blood cells) and replacing the plasma with special fluids. This may get solve something that, which causing a patient’s immune system to attack their body and keep it away from damaging other organs. It is not sure how this therapy helps patients with acute transverse myelitis, but it may remove inflammatory antibodies by replacing plasma.
Antiviral medications: Any patients who have a viral infection of the spinal cord or a virus causing illness may be treated with medications to treat the virus.
Pain relieving medication: Chronic pain is a most general complication of acute transverse myelitis. Medications, which may decrease muscle pain include common pain relievers, such as ibuprofen (Motrin IB, Advil, others), acetaminophen (Tylenol, others), and naproxen sodium (Aleve).
Nerve pain can be treated with anticonvulsant drugs, which stop seizures such as gabapentin (Gralise, Neurontin) or pregabalin (Lyrica), and antidepressant drugs, such as sertraline (Zoloft).
Medications to treat symptoms and other complications:
a doctor may prescribe other medications as needed to treat problems such as urinary or bowel dysfunction, muscle spasticity, ease stiffness, manage depression, help with sexual problems, or other complications associated with acute transverse myelitis.
Medications to avoid recurrent attacks of acute transverse myelitis:
Patients who have antibodies associated with neuromyelitis optica need these medications, such as immunosuppressants and/or corticosteroids, to reduce their chances of developing optic neuritis or more transverse myelitis attacks.
Ventilator: If symptoms of patients affect their breathing, this machine can help them to breathe with a breathing tube. It will make sure the patient’s body gets enough oxygen and have good saturation.
Rest: Patients need to stay in bed while they fight the disease.
Other therapies
Additional therapies generally focus on care and long-term recovery:
Physiotherapy: This treatment therapy helps improve coordination and strength.
Physiotherapists can teach patients about:
- Different ways to keep patient’s limbs flexible and muscles strong, while they recover
- How to use various tools that make life easier, such as wheelchairs, braces, or canes
- Various techniques to control bladder and bowels
Occupational therapy: This helps patients with transverse myelitis learn new ways of performing day-to-day activities, such as taking a bath, getting dressed, preparing a meal, and cleaning the house.
Psychotherapy: A psychotherapist can use talk therapy to treat the mental effects of anxiety, depression, sexual dysfunction, and other behavioral or emotional issues from dealing with transverse myelitis conditions.
Vocational therapy: This can help patient to find a job that works with their employer to make changes that patients need or suits their abilities.
Physiotherapy treatment for Acute transverse myelitis
A patient with transverse myelitis should take physiotherapy treatment because physiotherapy will improve function and promote quality of life. Physiotherapy is the most essential aspect of managing transverse myelitis in the short and longer-term.
Immediate goals for patients: To reduce pain and the frequent muscle spasms with jerking movements, which are experienced by the patient along with that to prevent extra physical deterioration.
Medium-term goals for patients: To improve joint range of motion and to normalize muscle tone.
Long-term goals for patients: To strengthen the affected muscles and to improve functional independence.
Early-stage, 1st 6-12 weeks:
Immediately after the onset of acute transverse myelitis, there is frequently a period of transient reduction or loss of neural activity below the involved spinal cord lesion; this is known as “spinal shock,” and generally it lasts around 6 to 12 weeks, although it may long for 6 months or more.
To achieve the immediate goals for Acute transverse myelitis, the Physiotherapist positioned the patient to reduce the low back and gluteal pain, and their trunk to relieve pressure off the low back. This can be achieved by placing a firm pillow under the thighs of a patient in a supine lying position. The patient is placed on a personalized splint using a crepe bandage on the left foot to correct the fixed plantar flexion.
Neuromuscular Stimulation: Neuromuscular electrical stimulation (NMES) is a therapeutic electrical modality frequently used in physiotherapy treatment. It is a form of electrical stimulation used to help contract a group of muscles or one of the muscles. If a patient is suffering from weakness in a particular muscle group because of transverse myelitis, a physiotherapist may choose to use NMES, in order to improve your overall function to help improve the contraction of that muscle group. NMES is a relatively passive treatment, and physiotherapy sessions should include active movement and exercise whenever required.
Later stage, post-spinal shock:
In this stage, two general problems can affect the bladder.
- The bladder becomes relatively insensitive, and so becomes overextended and tends to overflow OR the bladder become overly sensitive, and empty after only a small amount of urine has collected.
- An overly distended bladder increases the chances of urinary tract infections and it may threaten the health of the kidneys. Depending on the dysfunction, treatment options include medicines, timed voiding, padding for women, external catheters for males (a catheter connected to a condom), intermittent internal self-catheterization, an indwelling catheter, Botox, or electrical stimulation.
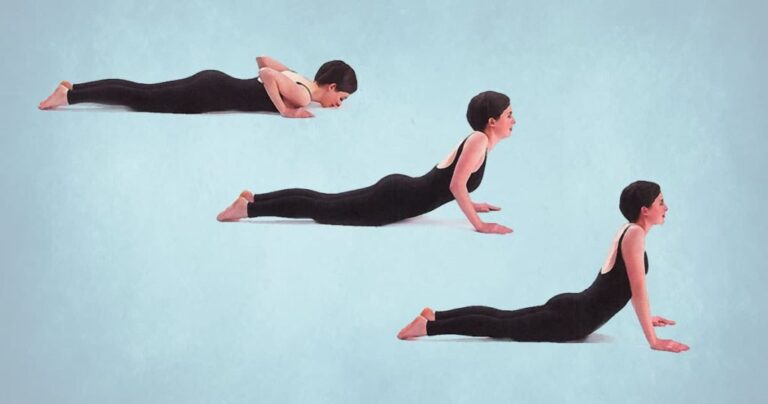
Muscle Weakness: It is important to do exercise. Physiotherapy treatment will increase muscle strength by improving running, walking, or swimming. Hydrotherapy treatment helps the muscles relax and will prevent muscle shortening and stiffness. Exercise will improve posture and balance.
Pain: Few patients with acute transverse myelitis may feel the pain that can arise from using the body in an unfamiliar way or muscle strain caused by nerve compression. Physiotherapy treatment will help reduce stiffness and pain by teaching the patients new ways of moving and improving their posture.
To reduce muscle spasms, physiotherapists advise cryotherapy using ice cubes wrapped in a clean towel, for 10 to 12 minutes, twice per day. After that, gentle stroking can be applied to the muscles of the legs and thighs. This is applied slowly from proximal to distal, in a straight line with help of the tips of the fingers.
Fitness levels: Physiotherapy treatment will help to achieve daily living tasks by improving energy levels, fitness, and stamina.
Mobility: Physiotherapists can advise patients for mechanical support like walking aids, wheelchairs, and orthotic devices in order to improve the functional ability of patients. Physiotherapy treatment can also teach transfer activities such as getting in and out of a bed, wheelchair, shower/bath, car, and onto and off a toilet, to improve safety and make patients independent.
For the medium-term goals, soft tissue mobilization and sustained gentle passive stretches were used to normalize muscle tone. Wringing and Kneading techniques were applied to each muscle group of the lower limbs, with more attention given to the affected lower limb with considerably more hypertonicity. Passive mobilization is also started to improve the joint range of movement of limbs.
Free active and resisted exercises can start subsequently with targeting all muscle groups, starting from the proximal to the distal muscle groups in an alternate manner, right to left and back to right for each muscle group. Resistance is provided manually with the help of the physiotherapist’s hands. Functional retraining mainly focused on bed mobility exercises, including rolling from side to side, bridging exercises, lower trunk rotation, curl-up exercises, standing and stepping exercises, and squatting and walking exercises.
Gait Training: The patient is having difficulty walking, therefore physiotherapists can work with patients on their gait. Patients will make sure that they are using the proper assistive device for their condition, and exercises can be performed to help improve overall gait. An important component of gait, walking, and mobility is the proper timing of muscle contractions. Physiotherapists may choose to work with patients to improve overall awareness and body control by performing exercises to help improve the speed and timing of muscle contractions.