Guillain barre syndrome (GBS): Symptoms, Cause, Diagnosis, Treatment, Exercise
Table of Contents
What is Guillain barre syndrome?
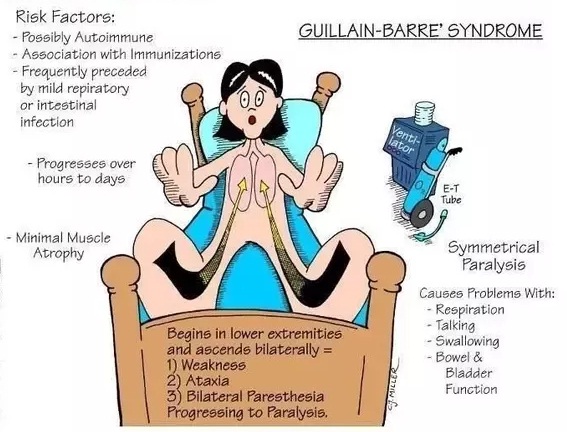
Guillain-Barre (gee-YAH-Buh-RAY) syndrome is a rare, serious neurological autoimmune disease in which the body’s immune system attacks the peripheral nervous system. Weakness and tingling in the patient’s extremities are usually the first symptoms that may last for months or years.
These types of sensations spread fast, eventually paralyzing the whole body. This disorder is a medical emergency, while its most severe form of GBS.
Most patients recover from Guillain-Barre syndrome (GBS), but the mortality rate is 4% to 7%. Around 1 or 2 cases in 100,000 people develop GBS each year in the United States. Both males and females and all parts of the world have similar rates of the condition. Researchers do not know why this disorder affects some people and not others.
The syndrome has described condition in 1916, named after the French neurologists Georges Guillain and Jean Alexander Barré, along with French physician André Strohl.
What are the symptoms of Guillain-Barre syndrome (GBS)?
Guillain-Barre syndrome (GBS) frequently starts with unexplained sensations, such as tingling sensation and weakness, sometimes even pain especially in children, occurs in the patient’s legs and feet and spreads to the patient’s upper body and arms. In around 10% of patients with this condition, symptoms begin in the face or arms. By the progression of Guillain-Barre syndrome (GBS), muscle weakness can turn into paralysis. These unexplained sensations generally disappear before the longer-term, major symptoms are seen.
Signs and symptoms of Guillain-Barre syndrome (GBS) may include:
The major symptom is weakness on both sides of the body which helps most people to look for medical attention. The weakness may first be seen as a problem with walking or climbing stairs. Symptoms generally affect the breathing muscles, arms, and also the face, which reflects more widespread nerve damage.
Occasionally symptoms begin in the upper body and move down to the feet and legs. Most patients have subsequent arm weakness, and possibly the weakness of facial, oropharyngeal, and ocular muscles.
Although few asymmetries can see in onset, weakness is always bilateral and severity is common.
GBS with proximal muscle weakness is very frequent, especially in starting phase, followed by distal arm and leg weakness. In 14% of cases, GBS with a descending pattern of weakness can see, with the initial onset of a cranial nerve or arm muscle weakness, and subsequent leg weakness. In 1/3 of the cases, the degree of weakness in the legs and arms is roughly equal.
Sensory disturbance
Prickling, needles, and pins sensations in patient’s fingers, toes, wrists, or ankles
50% of patients present with symmetric distal limb paresthesias, before clinical symptoms of limb weakness. Early finger paresthesias are known for a patchy process, likewise, the pattern is seen with distal axonopathies.
Paresthesias of the face or trunk are unusual, but sensory loss over the trunk is frequent.
Absent or reduced reflexes
Early loss of reflexes may be because of afferent impulses desynchronization in a reflex arc due to non-uniform demyelination.
Approximately 70% of patients with GBS present with a loss of reflexes; less than 5% retained all reflexes during the illness.
The presence of intact or normal reflexes can suggest an alternative diagnosis other than GBS.
Cranial nerve involvement In 45-75% of patients with Guillain-Barre syndrome (GBS), Cranial nerve involvement is seen. Cranial nerves III-VII and IX-XII can be affected.
Common complaints include:
- Facial Palsy means difficulty with facial movements including speaking.
- Diplopia, which is a double vision or inability to move the eyes
- Dysphagia means difficulty in chewing or swallowing
- Dysarthria
- Ophthalmoplegia
- Pupillary disturbances
- Oropharyngeal and facial weakness are usually seen after the limbs and trunk are affected.
- The Miller-Fisher variant of GBS is different in that this sub-type commences with cranial nerve deficits.
Dysautonomia
This occurs in about 65% of cases.
More general in patients with severe paralysis and ventilator difficulties but it can develop in mild cases.
Most common problems include cardiac dysfunction such as sinus bradycardia, sinus tachycardia, sinus arrest, other supraventricular arrhythmias, paroxysmal hypertension, and postural hypotension. ICU monitoring is important because of possible cardiac complications.
Other features include urinary retention, altered sweating, illus, inappropriate ADH, and mild orthostatic hypotension.
Inability to walk or unsteady gait or climb stairs
Coordination problems
Severe pain that may feel achy, cramp-like, or shooting and maybe worse at night
These all symptoms can increase in intensity over a period of hours, days, or weeks until certain muscles cannot be used at all and, when severe, the person becomes totally paralyzed, in which, the disorder is life-threatening—potentially interfering with breathing and at times with heart rate or blood pressure.
Patients with Guillain-Barre syndrome (GBS) generally get their most significant weakness within two weeks after symptoms start while by the third week 90 percent of affected patients are at their weakest level.
Symptoms of Guillain-Barre syndrome progression :
Antecedent Illness: Generally two-thirds of patients with GBS have an antecedent illness or event 1-3 weeks before the onset of weakness. Gastrointestinal and upper respiratory illnesses are the most commonly seen conditions. Symptoms are mostly solved during the time the patient presents with the neurological condition.
The time to the peak of symptoms is 12 days from 1st neurological symptoms, with 98% of patients reaching the highest level by 4 weeks. A plateau phase of unchanging and persistent symptoms then ensues, followed days later by gradual improvement of symptoms. Recovery generally starts by 2-4 weeks after the progression ends. Around 200 days is the meantime to the clinical recovery of GBS.
What are the types of Guillain-Barre syndrome?
Guillain-Barre syndrome can be known to occur in various forms.
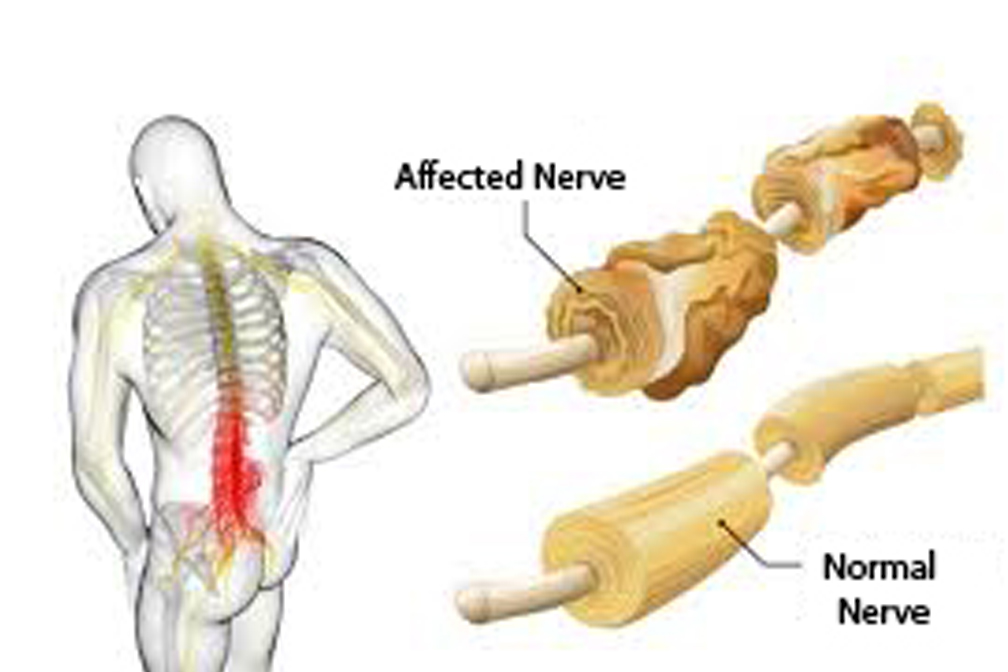
Acute inflammatory demyelinating polyradiculoneuropathy (AIDP), mainly affects the myelin. It is the most common form in Europe and North America. The major common symptom of AIDP is muscle weakness, which starts in the lower part of the patient’s body and spreads upward.
Miller Fisher syndrome (MFS), in which paralysis begins in the eyes and affects the tendon reflexes. MFS is more common in Asia but is less common in the U.S. It is an acquired nerve disease and one of the variants of GBS. This disease can lead to problems with walking associated with unsteady gait and balance.
Acute motor axonal neuropathy is a rare form of GBS, which affects the axons of the nerves going to the muscles, and causes sudden weakness in the limbs and sometimes trouble to breathe. It may affect nerves in the head sometimes. The commonest form in some Asian countries, and called “Chinese paralytic syndrome”.
Acute motor and sensory axonal neuropathy in which affect the axons of the sensory and motor nerves that begins with sensory changes, such as numbness or tingling.
Acute motor-sensory axonal neuropathy (AMSAN) and acute motor axonal neuropathy (AMAN) are less common in the U.S. But these types are more frequent in China, Mexico, and Japan.
Some types start more slowly and involve all symptoms. In chronic inflammatory demyelinating polyneuropathy, periods of weakness develop again over a number of years.
In multi-focal motor neuropathy, weakness affects several muscles in a specific part of a single or both legs or arms.
What are the causes and risk factors of the Guillain-Barre syndrome?
Causes
The main cause of Guillain-Barre syndrome (GBS) is not known. The condition generally appears days or weeks after a digestive tract or respiratory infection. This suggests that Guillain-Barré syndrome is triggered by a less proper immune response to the previous condition.
Sometimes, vaccination or recent surgery can cause or trigger Guillain-Barre syndrome. Recently, there have been cases noted after infection with the Zika virus. Guillain-Barre syndrome (GBS) can occur after the COVID-19 virus infection. It is also a rare response in a person who receives the Johnson & Johnson COVID-19 vaccine. It is not inherited or contagious.
In Guillain-Barre syndrome (GBS), a patient’s immune system usually attacks only invading organisms, which begin attacking the nerves. In Acute inflammatory demyelinating polyradiculoneuropathy (AIDP), the most common form of Guillain-Barre syndrome in the U.S., the nerves’ protective covering known as myelin sheath is damaged. The damage prevents nerves from transmitting signals to the patient’s brain, causing numbness, weakness, or paralysis.
Risk factors
Guillain-Barre syndrome (GBS) may affect all age groups. But risk increases as the age of a person is higher. It is generally more common in men than women.
Guillain-Barre syndrome may be triggered by:
- Infection with Campylobacter jejuni infection, a type of bacteria often found in undercooked food, especially poultry
- Mycoplasma pneumonia is caused by bacteria-like organisms which is an atypical pneumonia
- Cytomegalovirus, a strain of the herpes virus
- Epstein-Barr virus mononucleosis, which is typically caused by EBV
- Influenza virus
- Zika virus
- Hepatitis A, B, C, and E
- HIV, the virus that causes AIDS
- Hodgkin’s lymphoma
- Surgery
- Trauma
- Rarely, influenza vaccinations or childhood vaccinations
- COVID-19 virus
- COVID-19 Johnson & Johnson Vaccine
How is Guillain-Barré syndrome (GBS) diagnosed?
Guillain-Barre syndrome (GBS) may be hard to diagnose in its earlier stages. Its symptoms and signs are similar to other neurological conditions and may vary individually from person to person.
A doctor is likely to commence with a medical and recent history of illness and a thorough physical examination. Like some disorders, the diagnosis of Guillain-Barre syndrome (GBS) is mainly based on a patient’s symptoms along with their neurological examination. A healthcare provider may also need to order tests to differentiate other conditions that may present with similar symptoms as GBS.
Examination
A doctor or health care specialist may:
- Ask about symptoms of a patient, such as how long they have lasted and whether they are getting worse or not?- muscle weakness, which is getting worse over time is a common sign of Guillain-Barré syndrome (GBS)
- Examine the patient’s feet, hands, or limbs to check for symptoms like numbness
- Ask about the recent illness of a patient – Guillain-Barré syndrome (GBS) frequently follows an infection such as flu or food poisoning
- Check the patient’s reflexes, such as whether the patient’s leg twitches when the knee is tapped in a particular place (knee jerk) – patients with Guillain-Barré syndrome (GBS) generally have reduced or no reflexes
Diagnostic tests
Your doctor may recommend some tests:
Spinal tap
It is also known as a lumbar puncture. A small amount of fluid is taken from the spinal canal in the lower back of a patient. The fluid is tested for a type of change such as infection or else that generally occurs in patients who have Guillain-Barre syndrome (GBS).
It is a procedure that allows for the sampling of the cerebrospinal fluid, which surrounds a person’s brain and spinal cord. During this process, a small needle is inserted into the patient’s lower back. A small amount of cerebrospinal fluid is then removed and do analysis. The main motive of the analysis is to see for signs and symptoms of other disorders which may appear similar to Guillain-Barre syndrome (GBS) such as an infection of the nervous system as well specific findings which support a diagnosis of Guillain-Barre syndrome (GBS).
Electromyography
It is a test of the health and function of a patient’s muscles and nerves. Thin, tiny needle electrodes are inserted into the muscles, that doctor wants to study. Electrical recordings are taken to watch how they react when nearby nerves are activated. Guillain-Barre syndrome (GBS) damages the nerves, so findings on EMG test can be helpful to a patient’s healthcare provider in making the diagnosis of Guillain-Barre syndrome (GBS).
Nerve conduction studies
Small discs electrodes are taped on the patient’s skin above his nerves and minor electric shocks are used to activate the nerves and measure the speed of nerve signals or how quickly these signals travel along with them.
In patients with Guillain-Barré syndrome, these tests generally show that signals are not traveling along the nerves in a proper manner.
What are potential complications of Guillain-Barré syndrome (GBS)?
Guillain-Barre syndrome (GBS) affects a patient’s nerves. Because nerves control a person’s body functions and movements, patients with Guillain-Barre syndrome (GBS) may experience below given complications:
Breathing difficulties
The paralysis or weakness can spread to the muscles that control a person’s breathing, a potentially fatal complication. Around 22% of patients with Guillain-Barre syndrome need temporary help from a machine to breathe when they are hospitalized for treatment within the first week in the initial period. If this happens, patients may need a respirator to help them
to breathe.
Residual numbness or other sensations
Most patients with Guillain-Barre syndrome (GBS) recover completely or they have only minor, residual numbness or tingling, lingering weakness, or other odd sensations even after recovery.
Heart and blood pressure problems
Irregular heart rhythm means cardiac arrhythmia and Blood pressure fluctuations are common side effects of Guillain-Barre syndrome (GBS).
Blood clots
Patients who are immobile due to Guillain-Barre syndrome (GBS) are at risk of developing blood clots. Until the patient is able to walk independently, taking blood thinners and wearing support compression stockings may be recommended to minimize clotting.
Pressure sores
Being immobile also puts Patients at risk of developing bedsores or pressure sores. Frequent repositioning of the patient’s body relieves prolonged body pressure, which leads to bedsores or pressure sores.
Pain
About one-third of patients with Guillain-Barre syndrome (GBS) experience severe nerve pain, which may be resolved with medication.
Bowel and bladder function problems
Urine retention and Sluggish bowel function may be due to Guillain-Barre syndrome (GBS).
Relapse
Around 2% to 5% of patients with Guillain-Barre syndrome (GBS) experience a relapse.
Severe, early symptoms of Guillain-Barre syndrome (GBS) generally raise the risk of serious long-term complications. Rarely, death may occur from complications such as heart attacks and respiratory distress syndrome.
How to treat Guillain-Barré syndrome (GBS)?
Treatment for Guillain-Barré syndrome (GBS) can help decrease the symptoms and fasten the recovery.
Most patients are treated in hospital and generally need to stay in hospital for some weeks to a few months.
Intravenous immunoglobulin (IVIG)
- The most frequently used treatment for Guillain-Barré syndrome (GBS) is intravenous immunoglobulin (IVIG).
- When patients have Guillain-Barré syndrome (GBS), the immune system means the body’s natural defense system, produces harmful or dangerous antibodies that attack the nerves of the body.
- It is a treatment made from donated blood, which contains healthy and pure antibodies. These are given directly into a vein (intravenously) to the patients which helps to stop the harmful antibodies from damaging their nerves.
- High doses of immunoglobulin (IG) can block the damaging antibodies that may contribute to Guillain-Barre syndrome (GBS).
Plasma exchange or plasmapheresis
- A plasma exchange, also known as plasmapheresis, is sometimes used instead of Intravenous immunoglobulin (IVIG).
- The immune system produces antibodies, which are proteins that normally attack viruses, bacteria, and other harmful foreign materials. Guillain-Barré syndrome (GBS) occurs when a patient’s immune system makes antibodies by mistake, which attack the healthy nerves of the patient’s nervous system.
- This treatment includes being attached to a machine that removes the liquid portion of blood, which is known as plasma from a vein and filters out the harmful antibodies that are attacking the patient’s nerves before returning the blood to the body.
- Most patients need treatment over the period of approximately 5 days.
Other treatments
While in hospital, patients will be closely monitored to check for any problems with their heart, lungs, or other body functions. A patient will also be given treatment to ease their symptoms and reduce the risk of further complications. These may include:
- A breathing machine or ventilator, if a patient is having to breathe with difficulty.
- A feeding tube if patients have problems swallowing.
- painkillers if a patient is in pain.
- To avoid bed sores and keep the patient’s joints healthy, gentle movement around on a regular interval
- A thin tube called a catheter is in the patient’s urethra (the tube that carries urine out of the body) if they have difficulty peeing
- laxatives if patients have constipation
- Special leg stockings and/or medicine to prevent blood clots
- Once patients start to improve, they may also need extra support to aid their recovery.
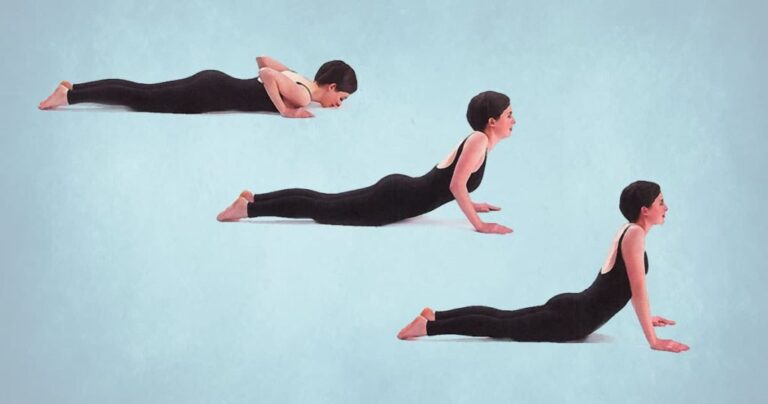
Physiotherapy treatment for Guilian-Barre syndrome (GBS)
A patient with Guilian-Barre syndrome (GBS) will benefit from physiotherapy. Physiotherapy treatment aims to fasten patients’ recovery and lessen the severity of their condition. Once discharged from the hospital a patient with Guillian-Barre syndrome (GBS) can go on to make important improvements with the help of physiotherapy. Physiotherapy treatment should be started as early as possible.
Physiotherapy treatment for Guillain-Barré syndrome (GBS) should commence in the hospital and continue until patients reached their maximum potential.
Goals of physiotherapy treatment include:
- Regain the patient’s independence with daily living tasks.
- Retrain the normal movement patterns of the patient.
- Improve patient’s posture while sleeping, sitting, and, standing.
- Improve the coordination and balance
- Maintain clear airways
- Prevent lung infection
- Improve muscle strength
- Increase mobility
- Increase fitness and energy levels
- Increased ability to relax
- Minimize secondary complications such as chest infections and muscle contractures.
- Support joint in functional position to minimize deformity or damage
- Prevention of pressure sores
- Maintain peripheral circulation
- Promote recovery
- Provide psychological support for the patient and their relatives.
Respiratory Care
The common respiratory complications in the rehabilitation setting include incomplete respiratory recovery including restrictive respiratory disease ( pneumonia, pulmonary scarring), chronic obstructive pulmonary disease, tracheitis from respiratory muscle insufficiency, and chronic intubation. Sleep hypoxia and hypercapnia, which worsen during sleep can be the result of a restrictive pulmonary function. Treatment methods are:
- Saturation records at night time with a pulse oximeter and bi-level positive airway pressure (Bi-pap) may be indicated for the patients.
- Special weaning protocol to avoid over fatigue of respiratory muscles can be recommended for more severe patients with a tracheotomy.
- Patients with cranial nerve involvement may need extra monitoring because they are more prone to respiratory dysfunction.
- Patients should be encouraged to stop smoking.
- 2-hourly turning into supine or side-lying positions for posturally drain areas of lung tissues.
- To improve chest expansion, a 2-4 liter anesthetic bag can be used. So, two people are needed for this technique, one to squeeze the bag and another to apply chest manipulation.
- Rib springing to stimulate cough.
- After the removal of a ventilator and adequate expansion, effective coughing techniques must be taught to the patient.
- Physiotherapy measures include breathing exercises, chest percussion, and resistive inspiratory training may be required to clear respiratory secretions to reduce the work of breathing.
According to Bensman (1970), the below given four guidelines are to be followed for the prescription of exercises:
- Use short periods of non-fatiguing exercises matched to the patient’s strength and endurance.
- Progression of the exercise should be done only if there is no deterioration in status after a week or if the patient improves.
- Return back the patient to bed rest if a decrease in function or muscle strength occurs.
- The goals should be directed towards improving function as well as improving strength.
Maintain normal Range of Motion
Gentle passive movements through full ROM at least three times a day especially at the shoulder, wrist, hip, ankle, and feet.
Prevention of Pressure Sores
Change in patient’s position from supine to side-lying every 2- hours. If the bedsores have developed then ice cube massage or UVR is given to enhance healing.
Maintenance of Circulation
Passive movements
Effleurage massage in lower limbs.
Relief of Pain
Transcutaneous electrical nerve stimulation (TENS)
Massage with passive range of motion
The patient can have increased sensitivity to light touch, a cradle may be used to keep the bed sheet away from the skin. Snug-fitting garments or low-pressure wrapping can provide a way to avoid light touch.
Strength and Endurance training
Strengthening exercises can involve isometric, isokinetic, or isotonic exercises.
Endurance training involves progressively increasing the intensity and duration of functional activities such as stair-climbing or walking.
Functional training
Retraining of bed mobility, transfers, dressing, washing, and ambulation activities comprise a big part of the rehabilitation process.
Proprioception and balance retraining in all these functional activities should be included, while motor control can be gained by doing Proprioceptive Neuromuscular Facilitation (PNF) techniques.
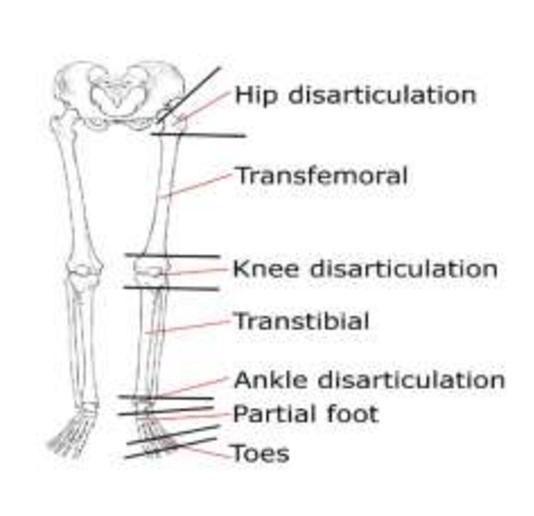
Orthoses
Use of light splints that are using PLASTAZOTE may be required for the given purpose listed below:
- Support the peripheral joints in a functional and comfortable position during flaccid paralysis.
- To prevent abnormal movements.
- To stabilize patients using pillows, and sandbags.
Assistive devices
Assistive devices such as wheelchairs, quadrupeds, and walking sticks should be made available to patients if required in order to facilitate effective and safe ambulation.



2 Comments