Spastic cerebral palsy and physiotherapy treatment:
Table of Contents
What is a Spastic Cerebral Palsy?
Spastic cerebral palsy is the type of cerebral palsy characterized by spasticity of muscle or hypertonicity (high muscle tone) often resulting in stiff, jerky movements. Spastic cerebral palsy influence the motor cortex of the brain, a specific portion of the cerebral cortex which targets to the planning and completion of voluntary movement.
Spastic CP is the most usual type of overall cerebral palsy, representing approximately 80% of cases. Spastic CP is a life long condition and will affect an individual across the lifespan.
The brain damage that causes spastic CP continuous stable over time, but the direction of spasticity affecting a person can change. For example, with growing age they may develop bone deformities from the pull of spastic muscles which does not allow free muscular movement and pulls both end of muscles that are attached to bone, muscular deterioration ( decrease in girth and function),and loss of range of motion in a joint. Thus, patients with spastic CP often have different support needs( splints and braces that correct the movement and posture) as they get older.
Patients of spastic CP are further classified according to the limbs or parts of the body that are most affected.Such classifications include:
Types of Spastic cerebral palsy:
Spastic diaplegia: In this condition either tow upper limbs or both lower limbs are affected.Its prognosis is around 50%.
Spastic hemiplegia: In this condition half of the body is affected ,either left or right , on the spastic side both limbs are symptomatic and contra-lateral side has muscular power up to 70%. Sometimes it also affects trunk and diaphragm.
Spastic quadriplegia: This is complete form of paralysis in which all four limbs and trunk looses muscle power, eventually in also targets bladder and bowel muscles.It is more severe type than others ; additionally , it has worst prognosis and chances of complete recovery are considerably low.
Spastic monoplegia: Monoplegia is rarest case of spastic cp . it only targets one limb unilaterally either leg or arm . It has best prognosis among all types.
Patients with the spastic type of CP typically have muscles that are “tight” and stiff due to high muscle tone ( hypertonicity). Spastic cerebral palsy has various symptoms that affects the patients.
Signs and symptoms of Spastic cerebral palsy:
In Initial 6 months there are some typical signs that appears only in spastic CP.
Lower limbs crossing when a child is picked up, also called scissoring
Stiffness
Head “lagging”( not in control – falls while picked up) when the child is picked up
6–10 months Making fist one hand
Difficulty in rolling
Problem while bringing hands together
Older than 12 months of age
Faces challenges while crawling
Difficulty in sit to stand activity, even with support
Walking with an unsteady, uncontrolled, or stiff gait
Spastic CP is different from other forms of cerebral palsy by its progressive symptom of spastic or stiff muscles, tight movements and gait patterns such as the scissoring gait. However, spasticity as a symptom is also observed in other life threatening conditions such as stroke and multiple sclerosis.Thus, the influence of spasticity alone does not accurately diagnose a conclusive of spastic cerebral palsy.
Changes in spasticity and correlated postures may also occur with other brain’s neural activity, such as excitement, fear or anxiety, or even pain, which elevates adrenaline secretion in body and increase the tone of muscle.A person with spastic CP will usually show, in addition to higher muscle tone, persistent primitive exaggerated reflexes, greater stretch reflexes, plantar reflex, and massive ankle clonus.
A third of people with cerebral palsy have seizures ( episodes of convulsions) – this is most common in spastic CP. Audiovisual, cognitive compromise and behavioral disorders can occur.
Causes and risk factor
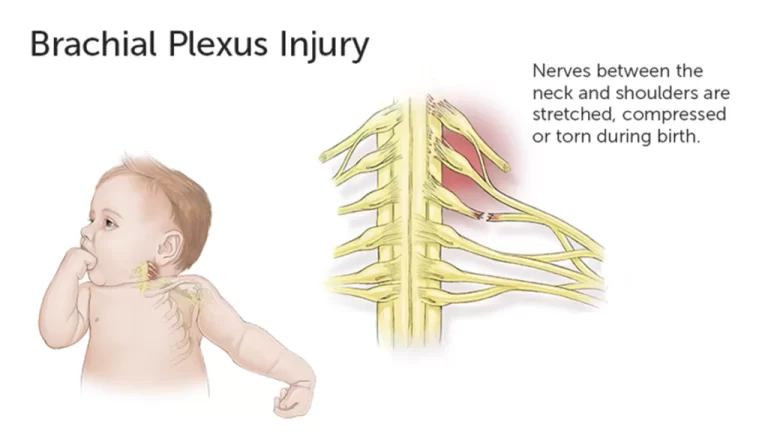
Spasticity in children can come from any disease process that affects the upper motor neuron within the central nervous system. Damage to the upper motor neuron reduces cortical input to the descending reticulo-spinal and cortico-spinal tracts, which results weakness, loss of motor control, and reduction in voluntarily active motor units. The reduction of these descending tracts removes the normal inhibition of the reflex arcs within the grey matter of the spinal cord, resulting in to a exaggerated reflex arc and spasticity. Which in certain cases there is no identifiable cause, typical causes include problems in intrauterine fetal development ( exposure to radiation, infection), asphyxia before birth, hypoxia (reduced oxygen supply) of the brain, birth trauma during labor and delivery (breech delivery), and complications in the prenatal period or during childhood. Infections to the mother, low birth weight (less than 2.0 Kg) is a major risk factor for CP. Also, between 40 and 50% of all children who develop CP were born prematurely ( birth before completing three trimesters). Premature infants are vulnerable, in part because their organs are not fully matured, increasing the risk of hypoxic damage to the brain that may manifest as cerebral palsy.
Each type of cerebral palsy is caused by damage to a specific part of the brain.Spastic cerebral palsy is caused by injury to the motor cortex and the pyramidal tracts of the spinal cord, which connect the motor cortex to the spinal cord. Understanding the function of the motor cortex and pyramidal tracts helps to explain how injury to these systems affects movement in patients with spastic CP.
An important aspect of the motor cortex in relation to cerebral palsy is its regulation of voluntary movement. Damage to this region of the brain makes voluntary movement harder to control and less fluid, or “spastic”.
Damage to the pyramidal tracts
The pyramidal tracts in the brain are the roots of communication between the cerebral cortex and the nucleus in the spinal cord. If pyramidal tracts are discorticated, the motor cortex is unable to send proper signals to the spinal cord. The spinal column is one half of the central nervous system, with the other half is the brain and brain stem. These parts of the brain are essential for sensory functions such as vision, touch and movement.
The cerebral cortex and pyramidal tracts may be damaged by:
Prenatal brain hemorrhage or infection due to exposure to toxins.
Lack of oxygen (hypoxia) to the brain during birth
Head trauma or infection after birth
Several risk factors may increase the chances of a developmental brain injury occurring. Poor maternal health and a reduced birth weight are just some of the risk factors for any type of cerebral palsy.
How to measure Spasticity?
The derivation to the diagnosis of spasticity in children with CP requires a whole physical examination, with ancillary testing as needed. The physical examination should be focused on motor control and power, muscle tone, passive and active range of motion of joints, sensation which includes proprioception, steriognosis, graphesthesia, kinesthesia, deep tendon reflexes, station (pelvic and leg alignment while standing, if there is a possibility), presence of upper limbs and lower limbs deformity, spinal stability.
Mechanical electromyography and nerve conducttechniques can also be used to assess spasticity. Mechanical instruments measuring the resistance of the muscle to passive stretch and electrophysiological measures showing the hyper excitability of the stretch reflex. One of most important tests in rehabilitation for physical examination of spasticity is the ashworth scale. Always test the patient while he or she is in a relaxed supine position.
Modified Ashworth Scale Degree of Muscle Tone
| Grade | Description |
| 0 | No increase in tone |
| 1 | Slight increase in muscle tone, manifested by a “catch” and release or by minimal resistance at the end of the range of motion when affected parts are moved in flexion or extension. |
| 1+ | Slight increase in tone,manifested by catch followed by minimal resistance throughout the remainder of range of motion. |
| 2 | More marked increase in muscle tone through most of the range of motion but affected part moves easily. |
| 3 | Considerable increase in muscle tone , passive movement difficult. |
| 4 | Affected parts rigid in passive flexion or extension. |
Treatment of Spastic Cerebral Palsy:
There are several medication available which has significant effects on spasticity and helps to reduce spasticity .
- (Neurontin) – Reduces the excitability of nerve cells in the brain, which play a role in seizures and the transmission of pain signals. It also minors the effects of GABA calming excited neurons. Reduces stretch pain and helps to gain control over involuntary muscle contraction.
- Baclofen – Relaxes muscles by acting on the central nervous system. It can reduce muscle spasms, tightness, and pain and improve range of motion. Side effects may be confusion or hallucinations, slight sedation compared to other treatments , loss of muscle tone or coordination, and weakness in unaffected muscles.
- Tizanidine – Reduces spasticity by blocking nerve impulses. However, it does not lessen muscle strength. As it lasts for a short time, tizanidine is best used only when you need it for relief or to be able to complete certain activities. Side effects may include low blood pressure, dry mouth, and sleepiness.
- Dantrolene sodium- Blocks signals that make muscles contract. This may reduce muscle tone. Side effects may be weakness, drowsiness, nausea, vomiting, dizziness, diarrhea, and rarely liver failure.
- Diazepam (Valium)- Used along with other medications to control muscle spasticity . It is also used along with other medications to control seizures. It is in a class of medications called benzodiazepines. It works by calming abnormal over activity in the brain.
- Clonazepam (Klonopin) – It controls involuntary muscle spasms, panic disorder and sometimes restless legs syndrome.
- Gabapentin (Neurontin) – Reduces the excitability of nerve cells in the brain, which play a role in seizures and the transmission of pain signals. It also minors the effects of GABA calming excited neurons. Reduces stretch pain and helps to gain control over involuntary muscle contraction.
All these medications are used to relax a large number of muscles.
The dosage of oral medicines is easily adjusted.
Oral medications may be stopped at any time.
Moreover, soon after medication physiotherapy treatment should be started and ballistic self stretching should be given so that with the help of medicine effect spastic muscles can be loosen easily. Adding to that this kind of practice has long lasting effects.
Technique to release spasticity:-
Botulinum Toxin
Botulinum toxin injection is now widely used as first-line treatment for focal spasticity. Botulinum toxin produces dose-related weakness of skeletal muscle by undermining the release of acetylcholine at the end of neuromuscular junction. This partially disturbs muscle contraction making the muscle temporarily weaker. Muscles usually treated with Botulinum toxin include the gastrocnemius-soleus muscle to allow planter flexion and hamstrings for knee extension ,hip adductors and flexor synergy muscles of the upper extremity to allow full range of motion.Intramuscular injections can be identified by surface landmarks, electromyography stimulation, or ultrasound. Following injection, muscle relaxation is evident within 48 to 72 hours and lasts for a period of 3 to 6 months. Botox injection can help improve a child’s ability to walk or use hands and room for a better fitting orthotics by reducing spasticity. Therapists can take advantage of the time when an overly tight muscle (agonist) is weakened to work on strengthening the muscle site side of the joint (antagonist). Sometimes, casting of the involved extremity is done after the injection to increase the stretch of the tight muscle
Physiotherapy treatment
Physical therapy consists of traditional exercises like passive range of motion to the hips and lower extremity joints and practice of gross motor skills at a level as age-appropriate for possible. The therapist also should emphasize active trunk extension and increased trunk and pelvic mobility. lead to improved posture and balance.
All traditional therapeutic approaches should be supplemented by neuromuscular facilitation techniques, of which there are a large number.”The most frequently used technique for the spastic diaplegic child is neurodevelopmental therapy, which aims at reduction of abnormal reflexes and postures and at helping the child to attain more normal movement patterns Traditional and neurodevelopmental exercises can be learned by most caretakers and are readily accepted by patients.These programs, supplemented by a reasonable amount of home therapy, appear to be beneficial.
Fixed deformities of the lower extremity joints and dislocation of the hips often can be prevented in rapidly growing ambulatory children or in those with ambulation potential. Effective physiotherapy is especially more important in the preschool and early school years.Physiotherapy can minimize or postpone orthopedic surgery and thus reduce the number of surgical treatments .Other effective therapies include aqua therapy, using reciprocal movement of the lower extremities,s7 and therapeutic horseback riding. The latter requires sitting in a desired position with abducted externally rotated hips and a balanced trunk. The warmth of the animal may also be beneficial to spastic hip adductors, but the main benefit to the child maybe emotional.”
Regular physiotherapy is important in early childhood and after orthopedic surgical procedures. However, in early adolescence and adulthood, it should be supplemented, if not replaced, by recreational activities, spesifically for children with mild to moderate physical impairment. Many spastic diaplegic children can become good swimmers and bikers; some can participate in team sports like soccer. The older patient may also find many suitable exercises in the special setting, mostly those aimed at relaxing spastic limbs.
Physical therapy (PT) is a fundamental part of spasticity management. Muscle over activity induce muscle shortening and muscle shortening increases spindle sensitivity. Muscle contracture and stretch sensitive muscle over activity are intertwined, Thus rehabilitation and physical treatments aimed at lengthening the overactive and tight muscles are fundamental.
Address both shortening and over activity . There are a number of different dynamic Physical therapy approaches, including the Bobath technique, Sensory integration therapy, poprioceptive neuromuscular facilitation and bobath, the Brunnstrom technique. Consider applying various techniques such as ice (cold), heat, positioning, stretching tight muscles and use of orthotic devices for these purposes.
Cold inhibits spastic muscles, but its effect is short-lived, perhaps outlasting the application of the cold by about half an hour.Apparently, heat is also used for relaxation of a spastic muscle. Position the child to stretch the spastic muscles and decrease the sensitivity of the stretch reflex and the brain stem reflexes that targets spasticity.
Also, the therapists should teach these positions to the family so that the child lies and sits this way most of the time at home. Massage and stretching muscles may stop contractures from progression and initiate muscle growth. Spasticity decreases with slow, continuous and sustained stretching.
This effect lasts from 30 minutes to an hour. Use stretching exercises before bracing casting to obtain the necessary joint position. Moreover, Orthoses are generally used in conjunction with physical therapy with the aims of increasing muscle length (through providing a sustained and static stretch), breaking up synergy patterns of movement and improving bio mechanics and stability. Muscle relaxation after stretching exercises lasts for a short period up to 15 minutes. For longer duration the stretch on the muscle should be maintained for several hours each day. This is achievable with the use of rigid splints or serial casting.
Exercise to improve child’s mobility
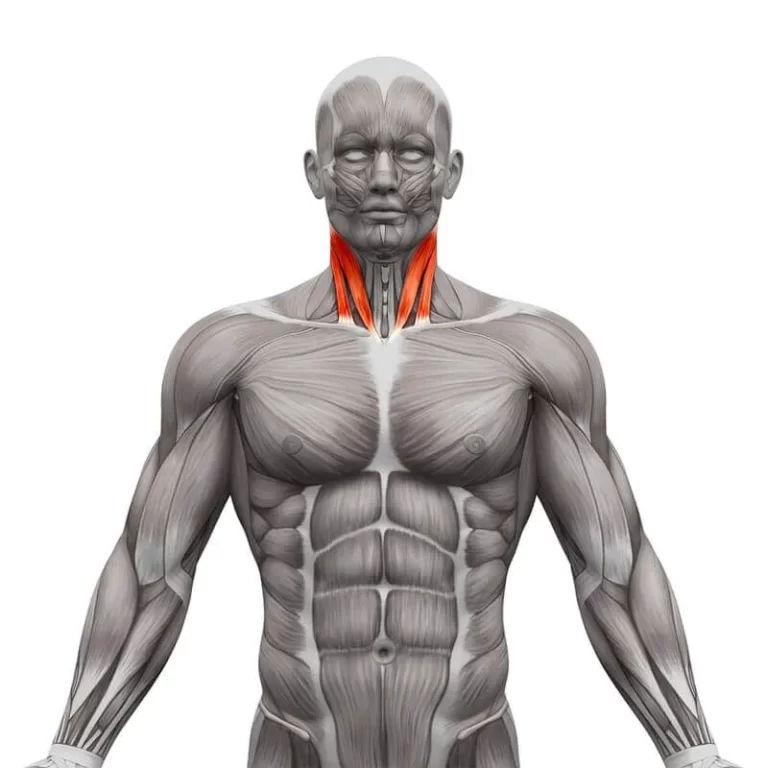
Neck range of motion movements (rotate the head in circles clockwise and counterclockwise)
Head turns (turning the head side to side)
Shoulder retraction and protection are also known as shoulder shrugging (raise and lower your shoulders)
Arm circles (spread baby’s arms to the sides so that the body makes a T shape and then move the arms in circles forward and backward)
Elbow extensions and flexion (bend and straighten your elbows)
Wrist rotations and stretch(hold forearm with another hand to stabilize it and then move the hand in circles)
Finger clenching or clawing (make a fist so that all fingers curl in and then straighten them back )
Finger abduction and adduction (join fingers together so that they touch on the sides and then spread them out as far as you can and make a fan-like structure)
Lateral leg raises (lie on the side, raise top leg up as far as the child can bare, then lower it)
Knee flexion and extensions (sit on a chair and repeatedly bend and straighten the knees with appropriate holds)
Ankle rotations, planter stretch, and dorsiflexion stretch (rotate the ankles in circles)
Positions to reduce spasticity:-
There are several positions that helps in reducing spasticity, further in physiotherapy treatment some prolong position are suggested to patient to maintain and practice regularly .
Flexor spasticity :-The hips and knees are maintained in a bended position with hips turned inward. Less frequently, hips and knees are rotated outward. Knees are bent in a flexed position and feet tend to point in a downward direction.
• Extensor spasticity :-The hips and knees are maintained in a straight position and the legs are very closed together or crossed over, with the foot in a downward position.
Lying on your stomach:- (prone position) This is an best position to try if you have spastic hip and knee flexors. Remember, give a few minutes to allow your hip muscles to relax in this new position. If able, let toes and foot hang over the edge of the bed to allow a neutral ankle position. As your hips relax, so will your calf muscles.
• Lying face up or in 3/4 position :- If knees tend to roll inward, try placing a rolled pillow or towel between your knees. Again, allow time for legs to accommodate and relax into the new position for a few minutes. Pillows under the knees only reinforce the knee flexion and should be avoided.
• Lying on side:- (side-lying) This is an best position if patient’s hips and knees are prone to extensor spasticity. Bend the knee of your top leg and let the knee of your bottom leg be straight. Patient can also put a rolled pillow or towel between your legs.
Correcting hip turn out:- If your hips and knees assume a “frog like” position due to spasticity, try lying on back. Place the end of a pillow, or a large beach towel, under patient’s upper thigh (hip to knee). Roll the towel or pillow so that patient’s hips and knees align themselves. Knees should be pointed toward the ceiling.
Correcting foot turn down :-If ankles and foot turn in a downward position, try to position patient’s ankles and feet in a neutral position, with toes pointed up toward the ceiling. The easiest way to achieve this is to place patient’s feet against a padded footboard. If the bed does not have a footboard, bracing or other orthotic measures may be needed.
Splinting, Casting and Orthoses:-
Casts, splints, and orthoses are the devices that are manufactured to keep the body in a certain position. These devices are used to prevent and correct deformities in the spastic extremity and to help children with cerebral palsy overcome daily activity limitations, such as challenges with standing and walking and serial casting or splinting can improvise the range of movement in a joint that is already contracted.
Serial casting is based on the premise that tightened muscles maintain the plasticity for lengthening. Providing a prolonged stretch gives bio mechanical benefits and inhibits spasticity. But there is a minor difference between inhibitive casting and serial casting, in inhibition casting only a single static cast is used and the aim is to reduce tone rather than lengthen muscle, thus improving function.
The most common type of orthosis is the ankle-foot orthosis also known as AFO. AFOs are technically designed to limit unwanted ankle movements, specially ankle plantar flexion (foot pointed toward the ground) . AFOs can be immobilized (to block ankle movement) or articulating (to allow for some movement of the ankle). Preventing plantar flexion through the use of AFOs has been found to bring betterment at walking efficiency in children with spastic diaplegic cerebral palsy and in children with hemiplegic cerebral palsy. When AFO use is compared to barefoot walking, the children’s walking patterns are improvised when wearing AFOs. For patient cerebral palsy who have tendency to walk on the toes, AFOs has shown to bring better ability to move from sit to stand. However, children with cerebral palsy who are able to stand on a pes planus foot do not benefit from AFOs for moving from sit to stand as the AFOs tended to slow down their speed to do work.
Surgical repair:-
If any treatment mentioned above does not show positive effect only then surgery is selected as option.Selective dorsal rhizotomy (SDR) comes from late 19th century procedures for spasticity. SDR is a neurosurgical procedure that includes partial sensory deafferentation at the levels of L1 through S2 in spinal nerve rootlets. After a continuation of tone management with rehabilitation punctuated with botulinum toxin injections, the child would probably be around 4 to 5 years old and SDR can be initiated. A suitable patient for selective dorsal rhizotomy is typified by:
1) If spasticity is still a problem
2) Grade 4 or 5 in strength of lower limbs and trunk muscles
3) Child is able to stand straight with good alignment
4) If intellectually good enough for carrying out training and understanding tasks.