Cerebellar Ataxia: Cause, Symptoms, Diagnosis, Treatment, Exercise
Table of Contents
Definition of Cerebellar Ataxia:
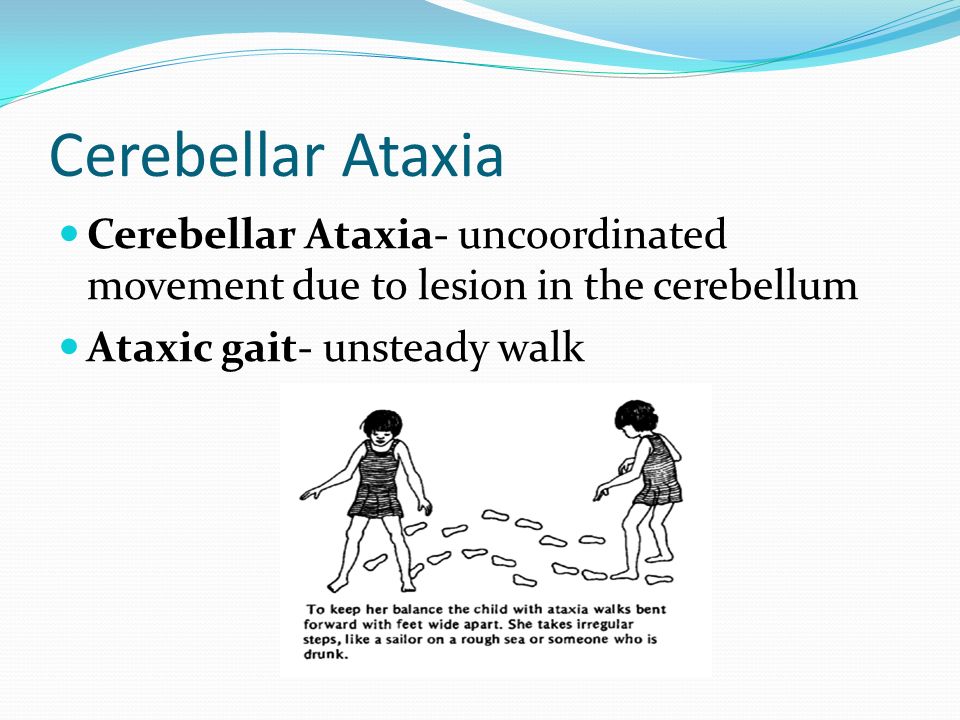
Cerebellar ataxia is an uncoordinated muscle movement with loss of Balance mainly due to lesions in the cerebellum. This is the part of the brain that can control muscle movement.
- cerebellar ataxia means delays in movement initiation, dysdiadochokinesia, dyskinesia, dysmetria, tremor, and disturbances in motor learning.
Cerebellum Anatomy:
- The cerebellum is a very important area in the human brain that plays a role in motor movement regulation and balance control.
Anatomical Position:-
-The cerebellum is the largest part of the hindbrain. It is located at the back of the brain, in the posterior cranial fossa behind the pons and medulla oblongata. It is separated from these lobes by the cavity of the fourth ventricle,
The cerebellum is attached to the brainstem by three fiber tracts called cerebellar peduncles.
Structure
The cerebellum consists of two hemispheres, Grey matter and White matter, which are connected by a narrow midline area called a vermis.
1)Grey matter – situated on the surface of the cerebellum. grey matter is tightly folded and forms the cerebellar cortex.
2) White matter – situated below the cerebellar cortex, fixed firmly in the white matter are the four cerebellar nuclei.
Nerves
-The cerebellum attaches to the brainstem by three groups of nerve fibers.
1) the superior
2) the middle
3) the inferior cerebellar peduncles
efferent and afferent fibers pass through these nerve fibers and connect with the rest of the nervous system.
Blood Supply
The cerebellum receives vascular supply from three paired arteries (originate from the vertebrobasilar anterior system).
1)Superior cerebellar artery (SCA)
2)Anterior inferior cerebellar artery (AICA)
3)Posterior inferior cerebellar artery (PICA)
Causes of Cerebellar Ataxia:
-cerebellar ataxia occurs due to brain damage, loss of nerve cells, or degeneration in the brain that controls muscle coordination (cerebellum).
-there are several causes that damage the peripheral nerve and the spinal cord which connect the cerebellum to the muscles. Ataxia causes include:-
1) Head trauma:- such as in a car accident, can cause acute cerebellar ataxia that comes on immediately.
2) Stroke:- When the blood supply to an area of the brain is interrupted or reduced due to a blockage or bleeding in the brain that prevents oxygen and nutrient supply to brain tissue and brain cells die.
3) Cerebral palsy:- It is a group of disorders caused during early development before, during, or shortly after birth which can affect the child’s ability to coordinate body movements.
5) Autoimmune diseases:-such as Multiple sclerosis, sarcoidosis, celiac disease, and other autoimmune conditions
6) Infections:- chickenpox, HIV, Lyme disease, and other viral infection.
7) Paraneoplastic syndromes:- degenerative diseases caused by the immune system’s response to a cancerous tumor from lung, ovarian, breast, or lymphatic cancer.
8) Abnormalities in the brain:- An abscess in the brain cause ataxia. Abnormal growth in the brain causes malignant or benign tumors that can also damage the cerebellum.
9) Toxic reaction:- Ataxia can occur due to side effects of such medications, mainly barbiturates, sedatives, Vitamin B-6 toxicity, antiepileptic drugs, and some types of chemotherapy.
10) Alcohol and drug intoxication:- heavy metal poisoning, such as lead or mercury; and solvent poisoning, such as paint thinner.
10) Vitamin E, vitamin B-12, or thiamine deficiency:- due to lack of these nutrients, because of the inability to absorb it.
11) Thyroid problems:- Hypothyroidism and hypoparathyroidism
Sign and Symptoms:
- Poor limb coordination:-impaired coordination in the torso or arms and legs
- Deterioration of fine motor skills
- an unsteady gait (Trouble walking, Wide gait, in severe cases, the patient may need a wheelchair.)
- uncontrolled or repetitive eye movements
- Dysarthria – slurred and slow speech. The patient may have difficulties in controlling volume, rhythm, and pitch.
- headaches
- dizziness
- Swallowing difficulties, which result in choking or coughing.
- Facial expressions become less apparent.
- Tremors – parts of the body shake or tremble unintentionally.
- Nystagmus – involuntary, rapid, rhythmic, repetitive eye movement. Movements may be vertical, horizontal, or circular.
- Cold feet – a lack of muscle activity.
- Hearing problems.
- Depression – patients having problem to live and cope with the symptoms.
Clinical Presentation:
1)Early onset cerebellar ataxia occurs between the ages of 4 and 26.
2) Late-onset ataxia occurs after the age of 20. Late-onset ataxia has less severe symptoms as compared to early-onset ataxia.
- Head posture: Upright and sometimes fixed.
- Trunk posture: Stooped leans forward.
- Stance: wide base of support
- Initiation of gait: Normal.
- Postural reflexes: positive or negative
- Steps: Stagger-lurching.
- Stride length: Irregular.
- Leg movement: Variable, ataxic.
- Speed of movement: Normal-slow.
- Arm swing: Normal, exaggerated.
- Turning corners: Veers away.
- Heel-toe test: Unable.
- Romberg’s test: +ve/-ve
- Heel-shin test: Usually abnormal.
- Falls: Uncommon.
Symptoms associated with cerebellar ataxia:
1) Dysmetria: This refers to inaccuracy in achieving distance in muscular acts; (hypermetria is overstepping; hypometria is under stepping. It is demonstrated while the patient attempting the finger-nose test.
2) Tremor: involuntary, rhythmic tremor, which is an oscillation that occurs during the movement of a body part.
-Intention tremor:- which increases in tremor towards the end of the movement.
-Postural tremor:- which occurs when holding a limb in one position.
-Titubation:- which is uncontrollable, rhythmic shaking affecting the head and upper trunk after lesion of the vermis.
-Postural truncal tremor:-which affects truncal instability, is seen in midline cerebellar lesions
4) Dysynergia: is uncoordinated and abrupt movements. This may have several reasons: agonist-antagonist and synergistic muscles may have disturbance in coordination during voluntary movement, or antagonist muscle may be failing to control eccentric contraction during the concentric contraction of agonist’s muscle.
With these two factors, the limb undergoes a sudden velocity resulting in inappropriate and uncontrolled motor movement.
5) Dysdiadockokinesia: This is the inability to be tested by rapidly alternating movements such as tapping the index finger on the thumb crease. The rhythm is irregular and the amplitude of each tap is variable.
6) Hypotonia: it is rarely seen in chronic cerebellar lesions. muscles are never fully relaxed in which a certain amount of tension and stiffness can be felt as resistance to movement. it is distinct particularly in proximal and antigravity muscles.
7) Weakness and fatigue: cerebellar dysfunction is impaired regulation of coordinated movements which leads to increased fatigue. Muscle needs to expend more effort to perform activities. This occurs more often with extensive and deep lesions and is most apparent in the proximal musculature. Fatigue has also been noted as a common symptoms of cerebellar dysfunction.
8) Dysarthria: This occurs due to in-coordination between tongue and lip muscles. The patient’s speech is irregular and slow, speaks like he is drunk.
9) Nystagmus: repetitive, uncontrolled eye movements that develop in horizontal and vertical directions mainly as nystagmus at the endpoint. It may cause reduced vision and depth perception which can affect balance and coordination.
10) Ataxia telangiectasia: It is a rare inherited disorder that affects the nervous system, immune system, and other body systems in which the ATM gene involved in detecting DNA damage, plays role in cell cycle progression.
-Small veins are seen near the corner of the eyes, cheeks, and ears.
-Physical and sexual development is usually delayed.
11) Oculocutaneous telangectasias: It usually appears at the age of 3–7 years. first seen in the interpalpebral bulbar conjunctiva away from the limbus.
12) Immune deficiency: It may lead to Recurrent sinopulmonary infections in the ataxia.
13) Pulmonary disease: Major cause of death – recurrent infections, interstitial lung disease, neuromuscular abnormalities (dysphagia, aspiration, resp muscle weakness).
14) Malignancy: 10-20% will develop cancer.
Diagnosis of Ataxia:
-MRI or CT scan: can show whether there is damage to the cerebellum and other brain structures.
-Genetic tests: It is used in the diagnosis of rare movement disorders to determine whether the patient has inherited ataxia.
-Blood tests: determine any underlying causes for the condition, Some types of ataxia affect the make-up of blood.
-Urine tests: Urinalysis suggests systemic abnormalities like urinary incontinence to some forms of ataxia.
Physiotherapy Treatment and Rehabilitation of Ataxia:
-The main aim of the physiotherapist in the whole exercise training program of ataxia which affects neurological structures and effecting the functions of the patient, is to improve the functional Re-education level of the patient through exercise. the therapist makes use of different strategies to make the patient functionally independent.
-Exercises should progress from simple to complex in both upper extremity and lower extremity
-Activities should be practiced first with the eyes open and later with the eyes closed for Improving balance and postural reactions against external stimuli and gravitational changes.
-Improving and increasing postural stabilization with the use of Compensation methods and supportive aids for the development of joint stabilization.
-Through developing independent and functional gait, improving the life quality of the patient by home exercise and sports activities.
Measurement and assessment:
-It can be achieved through the use of measurement and assessment methods and positive findings. On the basis of Measurement and assessment, the therapist can prepare a suitable treatment program but also changes in the treatment plan according to the patient’s condition over progress noted and it also depends upon the results of the treatment plan.
-All the observational methods and scales are mostly performed to assess balance.
The individual item scores are as follows:
-Gait (0 to 8)
-Stance (0 to 6)
-Sitting (0 to 4)
-Speech disturbance(0 to 6)
-Finger chase (0 to 4)
-Nose-finger test (0 to 4)
-Fast alternating hand movements (0 to 4)
-Heel-shin slide (0 to 4)
*Romberg test
-The patient can remove his shoes and stand with his two feet together. The arms should be held next to the body. The Therapist asks the patient to stand with eyes open, and subsequently with eyes closed. The patient tries to maintain his balance. If the patient has a loss of balance with their eyes closed, The Rhomberg test is positive. it occurs due to abnormal proprioception in the joints.
*test for Dysdiadochokinesia
-Rapidly alternating movement performed by the patient in which place the patient in a seated position with palm rest on the thigh. Ask the patient to turn their hands so their palms face upwards. Instruct the patient to alternate this movement as fast as possible. The test is positive when the movement is slow or awkward.
*the heel to shin test
- For the lower extremities, the examiner places the patient in a supine position and asks the patient to place the heel of one foot just below their other kneecap, move their heel across the shin in a proximal to distal motion. Ask them to repeat this procedure on the other leg. In a hemispheric cerebellar lesion, the patient will not be able to complete the movement smoothly in a straight motion.
*tandem gait testing
-To test tandem gait, Ask the patient to walk in a straight line by placing one foot directly in front of the other, heel-to-toe. patients with ataxia are not able to walk correctly in tandem gait.
*External Perturbation Test – Push and Release test, Purpose of static balance in ataxia. Following balance perturbations, fast and accurate stepping is an essential strategy to prevent falling. The latest literature reviews showed that perturbation-based balance exercise is effective to reduce fall risk in both normal older adults and in people with Cerebellar disease.
*Single Leg Stance Test: Purpose of static balance.
-Functional Reach Test: Purpose of functional static and dynamic balance. The Functional Reach Test is a single item test developed as a quick screen for balance problems in older adults. Interpretation: A score of 6 or less indicates a significantly increased risk for falls. A score around 6-10 inches shows a moderate risk for falls.
*Berg Balance Scale: Purpose of functional static and dynamic balance.
The Berg Balance Scale (BBS) is a 14-item objective that assesses static balance and fall risk in adults.
*Five Times Sit to Stand Test: The Purpose of this test is for functional dynamic balance.
*Measurements of gait duration, step length, step width can be used for gait training. Balance Confident Scale and scales for daily living activities such as FIM and Barthel Index can help to assist in assessment methods.
Physiotherapy exercise
1] Relaxed passive motion
2] General rocking movement
3] Relaxed positioning
4] Deep breathing exercise
5] PNF technique
6] Relaxation techniques
7] A ROM exercise & other free exercises
8] Frankle’s Coordination Exercise
9] balance training
10] Gait training :
-Lengthen stride length
-focus on the heel to toe pattern, Improve arm swing
-Parallel bar activities
-Walk on printed footprints
-Marching on spot with an arm swing
-Walking in a straight line
-Walking in a circle
-Walking sideways with an outstretched hand
*some points that are important while doing exercises:
-The recommended position should be maintained by the patient.
-The positioning should be comfortable.
-How many sets of exercises are generally required is decided according to the severity of the case because it can vary from patient to patient.
-Mostly, the number of sessions is two times a day is beneficial.
-mostly 2 to 3 sets of exercises with an interval of 5-6 minutes in between the sets.
-Progression can be like, starting with 2-3 exercises per session with repetition of 8-10, and when the task became easy therapist can increase the repetition to 10-20 or can add a variety of exercises to the program.
Ataxia Treatment :
1] Relax passive movement:-These are movements performed accurately and rhythmically by the physiotherapist through a full range of motion of all joints of the upper and lower extremities. The joint is moved in the pain-free range.
2] general rocking exercise:-This exercise strengthens your back, hip, and abdomen muscles.
- Lunges
-It is Challenging your balance and also increases strength in your legs and glutes.
-standing with your feet shoulder-width apart and arms down at your sides.
-Take a step forward with your right leg and bend your right knee, stop bending when your thigh is parallel to the ground.
-Push up off the right foot and return to the starting position. Repeat it with the left leg. Complete 10 reps for 3 sets. - Pushups
-In this exercise number of muscles are recruited to perform a movement.
-Start in a plank position. The core should be contracted, shoulders pulled down and back, and keep your neck neutral position.
-Gradually Bend your elbows and start to lower your body down to the floor. When your chest grazes it, extend your elbows and return to the start. Focus on keeping your elbows close to your body during the movement.
-Complete two sets of exercises as gradually increase repetitions as possible.
If you are not able to do this exercise, you can drop down to a modified stance on your knees — you’ll still reap many of the benefits from this exercise while building strength. - Squats
Squats increase lower body and core strength, as well as flexibility in your lower back and hips. Because they contract some of the big muscles in the body.
You can start by standing straight, with your feet slightly apart than shoulder-width, and while keeping your arms at your sides.
Brace your core and, keeping your chest and chin up, push your hips back and bend your knees as if you’re going to sit in a chair.
Try to keep your knees don’t bow inward or outward, gradually lower your body until your thighs are parallel to the ground, bringing your arms out in front of you in a comfortable position. Hold for 5 to 10 seconds, then gradually extend your legs and return to the first position.
Complete 2 sets of 10 repetitions.
- Standing overhead dumbbell presses
Compound exercises, which utilize multiple joints and muscles are perfect for busy bees as they work several parts of your body at once. A standing overhead press isn’t only one of the best exercises you can do for your shoulders, but it also strengthens your upper back and core muscles.
Equipment: 2 to 5 kg dumbbells
Pick a light set of dumbbells, we recommend 2 to 5 kg dumbbells to start and start by taking a standing position, either with your feet shoulder-width apart or staggered. Move the weights overhead so your upper arms are parallel to the floor.
By contracting your core muscles, start to push up until your arms are fully extended above your head. Keep your head and neck in a neutral position.
Hold for 5 to 10 seconds, gradually bend your elbows and lower the weight back down until your triceps muscle is parallel to the floor again.
Complete 2 sets of 10 reps.
- Dumbbell rows
This compound exercise strengthens multiple muscles in your upper body. Choose a moderate-weight dumbbell and ensure that you’re contracting at the top of the movement.
Equipment: 2 to 5 kg dumbbells
Start with a dumbbell in each hand. We recommend no more than 5 kg for beginners.
Bend forward at the waist so your back is at a nearly 45-degree angle to the ground. Be certain not to arch your back. Let your arms hang straight down. Ensure your neck is in line with your back and your core is contracted.
Starting with your right arm, gradually bend your elbow and pull the weight straight up toward your chest, making sure to contract your latissimus dorsi muscle, and stop just below your chest.
Return to the first position and repeat with the left arm. This is one rep. Repeat 5 to 10 times for 2 sets.
- Single-leg deadlifts
This is the best exercise that helps to improve your balance. Single-leg deadlifts require stability and leg strength. Grab a light to moderate dumbbell to complete this exercise.
Equipment: 2 to 5 kg dumbbell
You can start with a standing position with a dumbbell in your right hand while keeping your knees slightly bent.
Hinging at the hips, start to kick your left leg straight back behind you, lowering the dumbbell down toward the ground.
When you reach a comfortable height with your left leg, slowly return to the first position in a controlled motion, contracting your right gluteal. Ensure that your pelvis stays square to the ground during the movement.
Repeat 8 to 10 reps before moving the weight to your left hand and repeating the same steps on the left leg.
- Burpees: It is the best exercise to improve balance, stability of the trunk, and whole bodywork to develop endurance and muscle strength.
How to Do Burpees?
You can begin by standing upright with your feet shoulder-width apart while your arms are down at your sides.
With your hands out in front of you, start to gradually squat down. When your hands reach the ground, pop your legs straight back into a pushup position.
Jump your feet up to your palms by hinging at the waist. Get your feet as close to your hands as you can get, landing them outside your hands if necessary.
Stand up straight, bring your arms above your head, and jump.
This is one repetition. Complete 2-3 sets of 10 reps as per your stamina
- Side planks: It is the best exercise to improve the balance and stability of the trunk. This exercise helps to strengthen your core muscles.
You should control movements to ensure you’re completing this exercise effectively.
You can start with a Side-Lying position on your right side while your left leg and foot supported on top of your right leg and foot. Support your upper body up by keeping your right forearm on the ground, elbow directly under your shoulder.
Contract your core muscles to keep your spine straight and gradually lift your hips and knees off the ground, forming a straight line with your body.
Return to starting position in a controlled manner. Repeat 2 to 3 sets of 8–10 reps on one side, then switch to another side.
- Planks:
This exercise is an effective way to strengthen both your abdominal muscles and your whole body. Plank helps to stabilize your core without extra strain on your back.
You can start in a pushup position while keeping your hand and toes firmly placed on the ground, keeping your back straight, and your core contracted.
Keep your chin slightly tucked and your look just in front of your hands.
Take deep breaths while maintaining tension throughout your entire body, so your abs, shoulders, triceps, glutes, and quads are all contracted.
Complete 2-3 sets of 20-30 second holds depending on your stamina.
- Glute bridging exercise:
Bridging is also important to exercise to improve the stability and balance of the trunk.
You can start by lying on the soft mat while keeping your knees flexed, feet flat on the ground, and arms straight at your sides while your palms facing down.
Pushing through your heels, gradually raise your hips off the ground by squeezing your core, glutes, and hamstrings muscles. Your upper back and shoulders should still be in contact with the ground, and your core down to your knees should form a straight line.
Hold for 5 to 10 seconds at the top and return to the first position.
Complete 10–15 reps for 2-3 sets.
11. Double-Leg Foam Balance Activity: To do this exercise, stands on a soft foam surface with both feet on the ground. The therapist helps the patient balance in a random fashion.
Exercise dosage/progression: The duration of the activity is approximately 10 to 30 seconds. The difficulty is progressed as the subject improves by progressing to ball catching while the therapist helps the patient’s balance while standing on foam and progressing to single-leg support if tolerated without knee pain, swelling, or buckling.
Tilt board Balance Training: To do this exercise, the patient stands on a tilt board or balance board while keep patient both feet on the board. The therapist supports the tilt board in forwarding and backward and side-to-side directions for approximately 20 to 30 seconds each.
Exercise dosage/progression: The difficulty of the activity is gradually progressed by adding ball catching activity and progressing to single-limb support perturbations if the patient maintains single-limb weight-bearing activity without knee pain, swelling, or buckling.
Roller board and Platform Perturbations: The patient stands with one limb on a stationary platform and the other limb on a roller board. The therapist unsettles the roller board in multiple directions, at random, and the patient tries to resist this disturbance. The activity lasts approximately 20 seconds. The activity is repeated by changing the limbs on the platform and the roller board.
Exercise dosage/progression: The activity may start with the patient in the semi-seated position, with hips resting on the plinth if the patient has difficulty doing the activity in full standing. The exercise is gradually progressed to the full standing position when the patient is able to tolerate this position without pain.
Motivate patient to do accuracy of limb movements by using aids, cues & feedback
Combined activities of the trunk & limbs to improve coordination, balance & automaticity of movement
Frenkel’s exercise
Small weight cuffs, thera-bands can be used during activities to increase awareness of the limbs
Weight-bearing exercise of Upper Limb & Lower Limb
Rehabilitation
-Physiotherapy treatment can improve gait, balance, and trunk control for people with cerebellar ataxia, can reduce activity limitations, and support increased participation.
-The risk of falls is high and preventive measure are important to consider in patients with progressive ataxia given their high frequency and fall-related injuries also commonly seen.
-Careful assessment mainly balance is important to avoid falls.
-For people with cerebellar dysfunction, dynamic task practice that improves balance, stability, reduces stability limits, and aims to reduce upper-limb weight-bearing seems an important intervention to improve gait and balance.
-Strength and flexibility training may be indicated.
-Therapeutic equipment is often provided to support function.
-Intensity of training seems to be important as studies have shown that higher training intensities are associated with greater improvements in clinical outcomes.
-There is few evidence shows that improvement is highly in people with less severe ataxia and it is also related to the ability to learn the task.
-Targeted coordination exercise and gait training over a four-week period resulted in improvements in patient with cerebellar ataxia as measured by the Scale for the Assessment and Rating of Ataxia (SARA ) that was maintained after one year. Daily training session improved performances. This regular training session showed a more sustained improvement in patient with cerebellar syndrome as compared to people with afferent ataxias such as Friedreich’s ataxia and sensory ataxic neuropathy.
-Balance training exercises are undertaken in front of standardized moving visual images resulting in improvements in balance scores in some patients with SCA6 (pure cerebellar ataxia) in a pilot trial but results were mixed.
Specific Interventions to improve Balance and Gait
I. Video-game based coordinative training
eg. Intensive coordination training using whole-body controlled videogames can be useful and motivational therapy for children with cerebellar ataxia
II. Treadmill training
Treadmill training can be an useful exercise for patient with cerebellar ataxia due to brain injury. Intensity and duration of session seem to be important factors. Regular intensive exercise over many days associated with over-ground training may be helpful. Treadmill training has not been tested in people with progressive ataxias.
III. Visually guided stepping
Oculomotor and locomotor control systems in the brain interact during visually guided step training in that the locomotor system also depends on information from the oculomotor system during functional training for accurate foot placement. Very good improvements seen in oculomotor and locomotor performance have been seen following eye movement rehearsal in a small study done in patients with mild cerebellar syndrome.
Training of guided steps through eye movement alone, i.e. looking at foot for exact placement for each step, before negotiating a cluttered room, might improve performance and safety. This simple exercise, however task-specific and short-lived in nature, is promising and relatively quick, and easy to do in a functional setting.
IV. Balance and mobility aids
the role of balancing exercise and supportive mobility aids for patient with ataxia have an important role. Clinical experience shows suggests walking aids advice should be depends on a case-by-case basis.
To improve postural control, somatosensory cues from the fingertips – using light touch contact or a walking aid that helps to maintain or improve balance – can provide a supportive confidence orientation even when support levels are inadequate to provide physical support for the patient’s body. Some patient with cerebellar ataxia find light support- contact more effective as a strategy than a regular walking aid.
Walking aids also have the potential to compromise the ability to respond to balance disturbances through impeding lateral compensatory stepping and can thus affect safety, hence ensuring the appropriate walking aid is recommended for each patient.
Specific Interventions for Spasticity:
Physiotherapy treatment and exercise have an important role to play in educating patients and carers about incorrect posture, muscle use, and the avoidance of spasticity triggers such as pain and infection.
Regular Muscle stretching exercise help to maintain and improve the range of movement and prevent the formation of contractures. eg physical exercises which antagonize the overactive spastic muscle and also improve muscle strength; passive stretching by the therapist or carer; or physical positioning exercise. Active exercise is more effective than passive exercise if the patient is able; increased fitness can also reduce fatigue and improve further exercises.
Positioning with splinting, casting, orthosis, standing or also the use of weights, resistive devices, wedges, cushions, or T-rolls. If you advice prolonged splinting can require firm materials such as metal or plastic, with softer supportive materials such as foam or sheepskin, This can reduce the risk of skin damage. Orthoses should be made with high quality, well-fitted, and prepared by a specialist such as by orthotist or prosthetist.
- Hydrotherapy Pool Exercises
Mostly patient with cerebellar ataxia should be encouraged to exercise as part of overall health promotion (as long as risk factors and health and safety precautions have been necessory). Exercise should be planned according to what benefits most to the patient and may involve exploring several other options as well as building motivation and sustainability into the exercise program such as hydrotherapy, general fitness training.
Treatment and Exercises are planned to improve the coordination and balance of the patient that also help to recover over time.
Here are few tips that are important while doing exercises:
- The recommended position should be maintained by the patient for few seconds.
- The positioning should be comfortable and pain free however might some difficulties to hold the position.
- How many sets of the exercises are generally depends according to the severity of each case and patient’s condition because it can vary from patient to patient.
- Generally, the number of sessions is mostly two times a day.
- Two to three sets of exercises with an interval of 5-6 minutes rest in between the sets, in a controlled manner, are helpful.
- Gradual Progression can be like, starting with 2-3 exercises per session with repetition of 8-10, and when the exercise became easy one can increase the repetition to 12-15 or can add a few more exercises to the program and you can also increases difficulty level as per patient stamina.
Following are a few exercises that can be added to one’s treatment plan:
Lying bent knee rotation: this exercise focuses on the segmental movement of the lower limb and will help in bed movement and transfers. To do this exercise take a supine lying position with face up with both the knees bent, hip-width apart, and feet flat, arms can be positioned out wide away from the body. Now gradually start to let both the knees rotate from one side of the body to the other side. (trying to keep the upper body and back flat).
Kneeling press up: to do this exercise, you can start with an upright kneeling position with knees in the line of the hip and with arms at the sides, you can do gradual movement from a high kneeling position to keep your hip straight body upright, to gradual low kneeling position hip movement down to rest on heels.
–Quadruped weight shifting: to do this exercise keep your hand under kneeling and knees under hips and the back is a neutral position. gradually reach an arm forward to shoulder level, then start to extend the opposite-side leg backward to hip level. try to balance for a few seconds then gradually lowering both the arm and leg to the ground.
–Vestibular ball:
the vestibular ball is mostly used to improve balance, the external support of the Physiotherapist or the person helping to exercise, the patient is sitting upright on an exercise ball with feet apart, the legs are then locked by the therapist in order to avoid the risk of fall as the patient has poor balance. smoothly starts to move the upper body to the right and then to the left, allowing the weight of the trunk to shift from one side to another.
Standing heel to toe balance exercise: standing upright positions one foot in front of the other so the heel of the front foot is touching the toes of the back foot as if standing on a tightrope.
*Wheelchair Seating-
-Wheelchair mobility used when walking is difficult or impossible due to disability in rehabilitation. The pelvis mainly helps to maintain correct posture as it should be level and your spine should be straight. wheelchair mobility with appropriate postural support is provide independent mobility to people with ataxia. A physiotherapist trained progressive ataxia patients on how to use a wheelchair to perform day-to-day activities.







4 Comments