Distal Muscular Dystrophy: Cause, Type, Symptoms, Treatment
Table of Contents
Introduction
Distal muscular dystrophy is also known as distal myopathy.
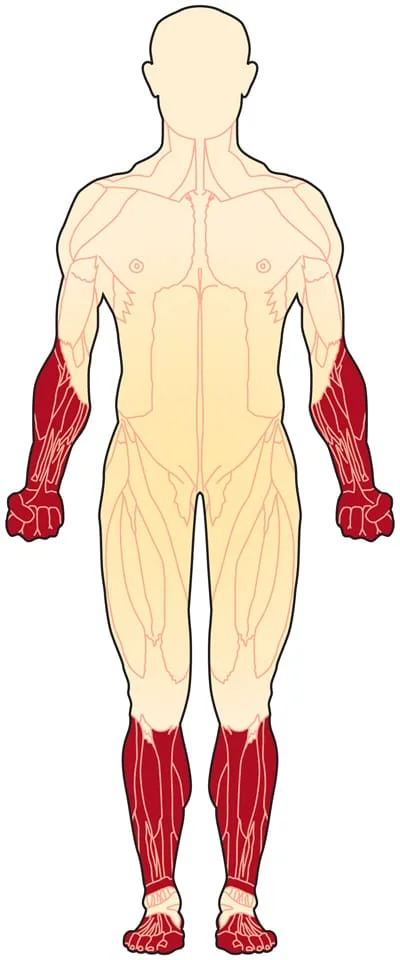
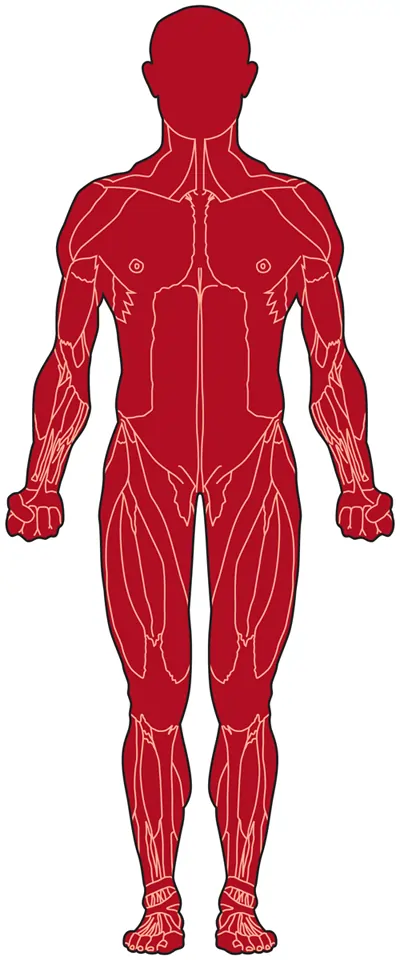
Distal muscular dystrophy (DD) is a group of rare, genetic, degenerative diseases that affect the voluntary muscles of patients. Distal muscular dystrophy causes weakness and atrophy preferentially that starts in the forearms, hands, legs, feet means the distal muscles of UL and LL. After then it may spread to affect other parts of the body. The muscles shrink, known as atrophy. DD affects both men and women, while usually appears between ages 40 and 60.
Causes
All forms of DD are inherited and caused by changes like mutations in certain genes. Our genes are located in our chromosomes and are made up of DNA. Each gene has the ‘recipe’ for a different protein and its variations, which are necessary for our bodies to function properly.
Changes in some different genes can cause various types of distal muscular dystrophy. While a gene has a mutation, it can make a defective protein or none at all. Most commonly, defective or missing proteins in the muscles prevent muscle cells from working correctly, which leads to symptoms of muscular dystrophy, including wasting and muscle weakness over time.
Muscles are made up of bundles of long muscle fibers or muscle cells. These fibers contract when nerve signals from the brain go to the specific spot in the junction, where the nerve activates the muscle. In some cases, the mutations that cause distal muscular dystrophy are in genes that make certain molecules in muscle cells.
The various types of DD are caused by ample genetic defects, not all of which are yet known. Some of the distal muscular dystrophies have been given different names based on various symptoms but in reality, it may be caused by defects in the same gene. The cause of this myopathy is very hard to recognize because it can be a mutation in any of at least eight genes and not all are known yet. These mutations can be inherited from autosomal dominant, one parent, or from both parents, autosomal recessive. There are eight types of distal myopathy that are known to us.
The genes usually occur in pairs in your body. Patients inherit a copy of the gene from each parent. A change or mutation in only one copy of the gene is enough to cause most forms of distal muscular dystrophy. This means the disease (Dystrophy) passes down in a dominant manner in patients. In some other types of Distal muscular dystrophy, the disease occurs only if a person has changed in both copies of the gene. These recessive forms of distal myopathies include Miyoshi muscular dystrophy and Nonaka distal myopathy.
In Finnish distal myopathy, people with 1 copy of the changed gene have a weakness in the muscles in tibial muscles means in the front of the lower legs after age 40. People with Finnish DD who inherit 2 changed genes have muscle problems in childhood age and they may need a wheelchair by age 30 years.
Symptoms
Typically, the first and main symptom of distal muscular dystrophy (DD) is muscle weakness. DD affects mainly the muscles of the lower legs and arms in the distal muscles. These muscles lose strength and mass. This may affect how well you can use a pen, grip things, or type. It may also cause walking problems. Due to this, Some forms of distal muscular dystrophy (DD) cause foot drop, which means difficulty in lifting the foot. With foot drop, the patient may drag his feet or lift his knees to walk with high steps. Intellect isn’t affected by this distal muscular dystrophy (DD).
In some cases, distal muscular dystrophy (DD) may affect other muscles. Depending on the form of DD, the weakness may also affect the muscles in the hips, trunk, neck, hands, or even the heart. Sometimes it affects the thighs. But in other cases, the upper legs stay strong. Certain types of DD cause difficulty with speaking or swallowing others may affect the heart.
Most forms of distal muscular dystrophy are progressive, but the rate of progression and age of onset can vary widely from one type to the other.
In most cases, the muscle mass of the affected regions may become visibly wasted means decrease in size. In some cases, trunk, arms, or legs, muscles may weaken, where the range of motion and mobility is limited. The different forms of DD tend to get worse in various ways.
Some examples include:
- Distal myopathy with the throat (pharyngeal) and vocal cord weakness affects the legs, hands, and voice. It may cause problems in swallowing, which is usually happening between ages 35 and 60.
- Finnish (tibial) distal myopathy affects the legs, especially, the muscles which are near the shin of the tibia. It usually shows up after age 40, and most people with this Distal myopathy (DD) can still walk throughout their lifetime. People who inherit 2 copies of the defective gene may have more severe weakness beginning in their childhood. They may not be able to walk later on. The heart may also be affected.
- Hereditary inclusion-body myopathy type 2 is seen between ages 25 and 40, which usually weakens the foot and thigh.
- Miyoshi distal myopathy causes weakness that starts in the calf muscles of the leg which is seen between ages 15 and 30. Some people with this form of distal myopathy(DD) may be unable to walk.
- Nonaka distal myopathy affects the muscles near the shin early, then affects muscle groups in the upper leg, upper arm, and neck. The thigh muscle means the quadriceps usually stays healthy and normal.
- Welander distal myopathy generally affects the arms in the beginning and then the legs. It is seen in individuals between ages 40 and 50.
Types of Distal Muscular Dystrophy
Distal muscular dystrophies or DDs are caused by many various genetic defects, but not all of them are known yet.
Many of these diseases can vary from one person to the other.
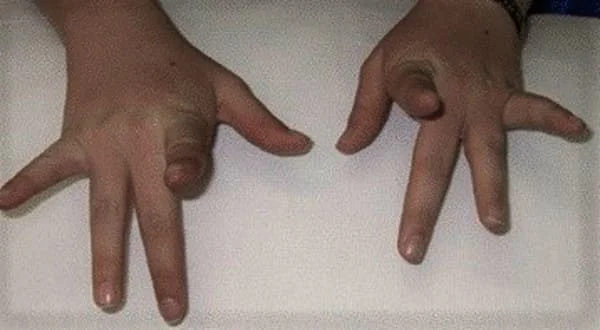
(1) Laing Distal Myopathy ( Distal Myopathy 1; Laing Early-Onset Distal Myopathy; MPD1) Mostly, Laing distal myopathy onset occurs before 5 years of age and has a clear pattern of degeneration muscle and weakness. primarily, specific muscles of the great toes and ankles are affected. Finger muscles also are affected along with the third and fourth fingers affected most severely. Additional findings include mild weakness of certain facial muscles and weakness of neck flexion muscles. Progression of Distal Myopathy 1 is extremely slow and affected individuals do not require a wheelchair even into their sixties.
(2) Inclusion Body Myopathy Type 2; IBM2; Distal Myopathy with Rimmed Vacuoles (DMRV); Nonaka Myopathy It is characterized by degeneration and progressive weakness of the distal muscles of the legs. Onset occurs between 10 to 40 years of age. Affected persons may experience foot drop and gait disturbances. Muscle weakness spreads to affect the hands and certain proximal muscles of the upper legs including hamstrings and the thigh. The shoulders muscles and neck muscles may be involved in some cases.
(3) Distal myopathy with vocal cord and pharyngeal Signs (MPD2; Distal Myopathy 2)
Symptoms are seen between about 35 and 60 years of age and It is characterized by degeneration and weakness of the distal muscles of the feet and hands. Sometimes, muscles of the shoulder may be involved. Weakness of the vocal cord muscles and muscles of the throat means pharyngeal muscle may also occur danger resulting in the ingestion of food or liquids into the lungs means aspiration or difficulty swallowing, known as dysphagia. Lower leg braces can support weak muscles.
(4) Finnish tibial distal myopathy
Finnish muscular dystrophy features weakness initiating after age 40 in the lower extremities particularly the muscles over the tibia which is a bone in the lower leg and progressing slowly to the trunk and muscles of upper extremities. Cardiac problems can occur. Patients with only one defective gene experience mild weakness of the tibial leg muscles in the front of the calf sometime after age 40. Patients with two defective genes have progressive muscle weakness starting from childhood and may not walk by age 30. It can be severe or benign.
(5) Gowers-Laing distal myopathy
Gowers-Laing distal myopathy results from mutations in the MYH7 gene, which instructs for myosin, a protein that participates in muscle contraction. Its onset occurs from childhood to 25 years of age, weakness starts in the neck and leg muscles and progresses slowly to hands, upper leg muscles, and more neck muscles.
(6) Miyoshi Myopathy
This type is caused by mutations of the dysferlin gene. Onset is generally between 15 to 30 years of age. patients experience degeneration and weakness of the leg muscles, the calves, which may appear bulky or abnormally large means pseudohypertrophy in starting. Initially, patients may be unable to stand on their toes. Eventually, muscle weakness spreads to affect the proximal muscles of the upper legs often causing difficulties in standing, climbing stairs, or walking. Muscles in the shoulder area, forearms, and, hands, may also be affected. As the disease progresses, patients have significant difficulty walking and require a wheelchair.
(7) Welander distal myopathy
The onset of this type occurs between 40 and 50 years of age and the cause is unknown. Muscles of the hands and feet include intrinsic muscles and long extensors and certain muscles of the fingers and toes extensors are predominantly affected. Muscles in the upper extremities are affected first with the muscles in the lower extremities becoming involved later on or not at all. The degree of muscle weakness may range from mild to severe.
(8) VCP Myopathy / IBMPFD
VCP Disease is caused by a mutation in a gene named, the Valosin Containing Protein (p97 or VCP). When the VCP gene is mutated, mitochondrial function and cell division are disturbed, which leads to several possible symptoms and disorders.
VCP Disease identifies the three primary disorders associated with the disease: Paget’s Disease of Bone, Inclusion Body Myopathy, and Frontotemporal Dementia. A person with VCP Myopathy may have one, two, or all of these disorders.
(9) Hereditary inclusion-body myositis (myopathy) type 1 (HIBM1)
It usually starts between the ages of 25 and 40, first involving the thigh muscles and the muscles that lift the front of the foot. Under the microscope, muscle cells show vacuoles, which are cellular bubbles, and inclusion bodies, which are abnormal clumps of cellular material. The cause is not known.
(10) UDD Distal Myopathy (Tibial Distal Myopathy)
It is characterized by muscle weakness that affects the ankles and may spread to affect the muscles of the tibia (shinbone). It starts usually after 35 years of age and progression is slow. Eventually, the extensors of the toes may be involved resulting in clumsiness and unable to turn the toes and feet upward, known as foot drop, which may make it problematic to pick up the front of the foot while walking.
(11) Distal Myopathy 3 (MPD3)
This extremely rare form of distal myopathy is characterized by atrophy and muscle weakness that can begin in the distal muscles of the legs or arms. An affected person may be clumsy with their hands or experience gait abnormalities like frequent stumbling. Mild contractures of the hands may be seen. Onset occurs between 32-45 years of age. The disease will progress to affect extra muscles such as the proximal muscles of the upper legs.
Diagnosis of Distal Muscular Dystrophy
A doctor or healthcare provider usually starts by taking a patient and family history, asking about recent symptoms, and past health conditions, and performing a physical examination. The doctor wants to determine whether the patient’s weakness results from a problem in the muscles or in the nerves that control them.
Special tests called electromyography (EMG) and nerve conduction studies (NCV) are done. In these tests, electricity and needle electrodes are used to stimulate and assess the muscles or nerves individually to see where the problem is. Electromyography is uncomfortable but not usually very painful.
Blood tests may find elevated levels of creatine kinase (CK), an enzyme that is frequently found in abnormally high levels while a muscle is damaged. Elevated CK levels occur in some, but not in all cases of distal myopathy, except Miyoshi myopathy where it is vitally elevated. The detection of rising CK levels can confirm that muscle is inflamed or damaged, but cannot confirm a diagnosis of distal myopathy.
To determine the cause of CK elevation, a doctor advised muscle biopsy, which is the surgical removal of a small sample of muscle from the patient. By examining samples, doctors can tell about what’s actually happening inside the muscles. Biopsy of affected muscle tissue may find characteristic changes like increased fat and connective tissue. In some forms of distal myopathy, numerous sub-cellular compartments namely rimmed vacuoles can be found on muscle biopsy. Modern techniques can use the biopsy to distinguish muscular dystrophies from inflammatory disorders, infections, and other problems.
Genetic or DNA tests, by using a blood sample can analyze the patient’s genes for particular defects that cause DD, help families assess the risk of passing on the disease to the next generation, and help predict the course of a disease.
MRIs of muscle tissue may reveal a distinct or specific pattern of muscle or involvement damage. Distinct patterns have been identified in patients with UDD, Welander, and other distal muscular dystrophies.
Treatment of Distal muscular dystrophy (DD)
Patients with distal muscular dystrophy (DD) should be monitored regularly throughout their lives. Treatment options include physiotherapy treatment and occupational therapy, medications, and surgical and other procedures. Assessments of breathing, swallowing, walking, and hand function enable the team to adjust treatments as the disease progresses.
Unfortunately, there is no cure for distal muscular dystrophy (DD). However, the right treatment or supportive care may help reduce symptoms of patients. One essential treatment option is physical therapy, which may increase the range of motion and help keep joints and muscles strong and flexible. Occupational therapy is quite the same treatment, but it mainly focuses on certain tasks that will be useful in a patient’s daily life such as eating, bathing, walking, or computer use.
Lower leg and foot weakness
The weakness of these muscles can make it difficult to walk. In some cases, an ankle-foot orthosis (AFO), a brace that can wear over the lower leg and shoe can help.
AFOs are mostly useful when muscles in the front of the lower leg aren’t strong enough to pick up the front of the foot while walking, which is known as foot drop. in that, an AFO can prevent the foot from flopping down and tripping the person.
Forearm and hand weakness
An occupational therapist can help patients get the most out of their forearm and hand muscles in performing day-to-day activities. The therapist can recommend devices that may be useful in improving grip strength or help support arms for eating or using a keyboard.
Swallowing and heart problems
Some forms of distal muscular dystrophy usually affect the muscles, which are used for swallowing purposes, for that precautions must be taken while drinking or eating so that food can not aspirate into the lungs.
Other forms of DD affect the heart, and special precautions must be taken to monitor heart function regularly.
Physiotherapy Treatment:
Several types of therapy including exercises and assistive devices can improve the quality and the length of life in patients who have distal muscular dystrophy (DD).
stretching and Range-of-motion exercises of affected joints. Muscular dystrophy can restrict the mobility and flexibility of joints. Limbs generally draw inward sides and become fixed in that position only. Range-of-motion exercises can help to keep joints as flexible and mobile as possible. It includes passive, active-assisted, active, and resisted exercises in progression. Some strengthening exercises might be helpful in this. But it’s important to talk with the doctor first as some types of exercise might be harmful.
Exercise such as Low-impact aerobic exercises, including swimming and walking, can help maintain mobility, strength, and overall health.
Braces can help keep tendons and muscles flexible and stretched, which slows the progression of contractures. Braces can also help in function and mobility by providing support for weakened muscles of limbs.
Mobility aids like walkers, Canes, and wheelchairs can help maintain mobility and independence.
lightweight leg braces for support
an ankle-foot orthosis (a brace worn over the foot and lower leg)to treat foot drop
keyboard and mouse alternatives
Handwriting devices
Cuffs, openers, braces, and other adaptive devices
If respiratory or heart problems occur, devices like respirators and pacemakers may be used