Antiphospholipid Syndrome (APS)
Table of Contents
What is an Antiphospholipid syndrome (APS)?
- Antiphospholipid syndrome (APS) is a systemic autoimmune disorder characterized by the presence of antiphospholipid antibodies in the blood. These antibodies target phospholipid proteins and cell membranes, leading to a hypercoagulable state, which means the blood is more prone to forming clots.
- This condition can result in various clinical manifestations, including blood clots in arteries and veins, recurrent miscarriages in pregnant women, and other pregnancy complications. APS is often diagnosed through blood tests for antiphospholipid antibodies and is managed with anticoagulant medications to prevent clot formation.
Cause of antiphospholipid syndrome (APS)
The exact cause of antiphospholipid syndrome (APS) is not fully understood, but it is considered an autoimmune disorder. Here are some factors believed to contribute to its development:
- Autoimmune Reaction: APS occurs when the body’s immune system mistakenly produces antibodies, known as antiphospholipid antibodies, that target phospholipid proteins. These antibodies can then trigger abnormal clotting.
- Genetics: There may be a genetic predisposition to developing APS. Some individuals may be more genetically susceptible to autoimmune conditions.
- Infections: In some cases, infections, particularly viral infections, may trigger the development of antiphospholipid antibodies and subsequently APS.
- Medications: Certain medications, such as hydralazine and procainamide, have been associated with drug-induced APS. These medications can trigger the production of antiphospholipid antibodies in susceptible individuals.
- Other Autoimmune Diseases: APS can occur on its own (primary APS) or in conjunction with other autoimmune diseases, such as systemic lupus erythematosus (SLE). When it occurs in the presence of another autoimmune disease, it is called secondary APS.
- Hormonal Changes: Some evidence suggests that hormonal changes, such as those that occur during pregnancy or with the use of hormonal contraceptives, may influence the development or exacerbation of APS.
- Environmental Factors: Exposure to certain environmental factors or toxins may play a role in triggering or exacerbating autoimmune conditions like APS, although specific links are not always clear.
- Thrombophilic Conditions: APS is often associated with a prothrombotic (increased clotting) state. Conditions like hyperhomocysteinemia or deficiencies in natural anticoagulants (e.g., protein C or protein S) can increase the risk of clot formation and may be present alongside APS.
- Endothelial Damage: Damage to the inner lining of blood vessels (endothelium) can trigger clot formation. Conditions like infections, trauma, or inflammation can contribute to endothelial damage, potentially worsening the risk of clotting in individuals with APS.
- Lifestyle Factors: Smoking and obesity are known risk factors for cardiovascular disease and can exacerbate the clotting tendencies in APS.
- Stress: While the exact relationship is not fully understood, chronic stress may contribute to the development or worsening of autoimmune conditions, including APS, through its effects on the immune system.
- Reproductive Factors: APS is associated with pregnancy complications, such as recurrent miscarriages and preeclampsia. The exact mechanisms involved in these complications are still being studied.
Risk factors
Several risk factors can increase an individual’s likelihood of developing antiphospholipid syndrome (APS) or experiencing complications associated with APS. These risk factors include:
- Autoimmune Diseases: People with other autoimmune disorders, such as systemic lupus erythematosus (SLE), rheumatoid arthritis, or Sjögren’s syndrome, are at an increased risk of developing APS. APS can occur secondary to these conditions.
- Gender: APS is more common in women than in men. This gender disparity may be due to hormonal influences.
- Age: APS can develop at any age, but it is most commonly diagnosed in individuals between their 20s and 50s.
- Genetics: A family history of autoimmune diseases or a genetic predisposition to autoimmune conditions may increase the risk of developing APS.
- Hormonal Factors: Hormonal changes associated with pregnancy, the use of oral contraceptives, or hormone replacement therapy can influence the development or exacerbation of APS, particularly in susceptible individuals.
- Infections: Certain infections, such as viral infections like HIV or hepatitis C, can trigger the production of antiphospholipid antibodies and potentially lead to APS.
- Medications: Some medications, including hydralazine and procainamide, have been linked to drug-induced APS. These medications can induce the production of antiphospholipid antibodies in some individuals.
- Smoking: Smoking is a known risk factor for cardiovascular disease and can exacerbate the prothrombotic tendencies in APS.
- Obesity: Obesity is associated with an increased risk of cardiovascular problems, including clot formation, which can compound the clotting risk in APS.
- Prior Thrombotic Events: Individuals who have previously experienced blood clots or thrombotic events are at a higher risk of recurrent clots if they have APS.
- Pregnancy: Women with APS are at an increased risk of pregnancy-related complications, including recurrent miscarriages, preeclampsia, and fetal growth restriction.
- Other Thrombophilic Conditions: Coexisting conditions that promote blood clotting, such as deficiencies in natural anticoagulants or high levels of homocysteine, can increase the risk of clot formation in individuals with APS.
Symptoms of antiphospholipid syndrome (APS)
The symptoms of antiphospholipid syndrome (APS) can vary widely from person to person, and some individuals may not experience noticeable symptoms until a blood clot or other complications occur.
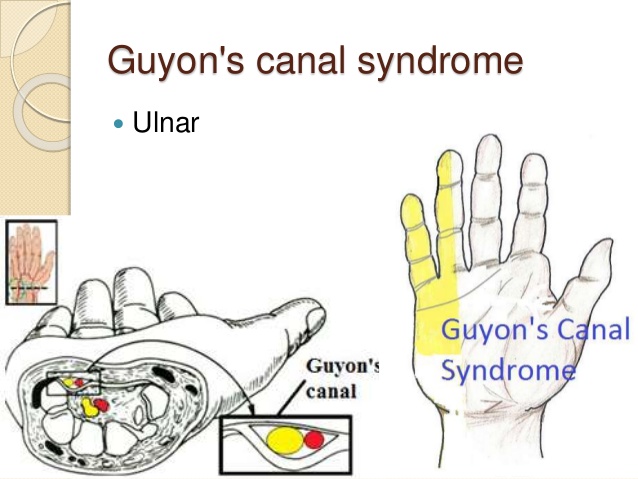
- Blood Clots: APS often leads to an increased risk of blood clots, which can occur in veins (deep vein thrombosis) or arteries (arterial thrombosis). Symptoms of clotting may include pain, swelling, and redness in the affected area.
- Recurrent Miscarriages: Women with APS may experience multiple miscarriages or fetal losses during pregnancy, typically in the second or third trimester. Other pregnancy complications like preeclampsia and fetal growth restriction can also occur.
- Neurological Symptoms: APS can affect the nervous system, leading to symptoms such as headaches, migraines, seizures, memory problems, and even strokes.
- Skin Conditions: Some individuals with APS may develop skin manifestations, including livedo reticularis (mottled discoloration of the skin) and skin ulcers.
- Cardiovascular Symptoms: APS can contribute to heart problems, including chest pain (angina) and heart valve abnormalities.
- Lung Problems: Pulmonary embolism (a blood clot in the lung) can occur, leading to symptoms like shortness of breath, chest pain, and coughing up blood.
- Kidney Issues: APS may affect the kidneys, leading to kidney dysfunction or kidney failure.
- Gastrointestinal Symptoms: In some cases, APS can cause abdominal pain, nausea, and other gastrointestinal symptoms, although these are less common.
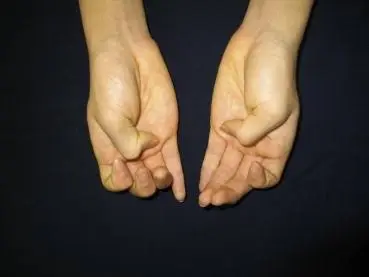
- Joint Pain: Joint pain and inflammation, similar to arthritis, can occur in some individuals with APS.
- Low Platelet Count: APS can occasionally lead to low platelet levels (thrombocytopenia), increasing the risk of bleeding.
Diagnosis
Diagnosing antiphospholipid syndrome (APS) involves a combination of clinical evaluation and laboratory tests. Here are the key steps and criteria typically used to diagnose APS:
Clinical Evaluation: A healthcare provider will start by assessing your medical history and conducting a physical examination. They will ask about any symptoms you may be experiencing, as well as any previous blood clots, miscarriages, or pregnancy complications.
Antiphospholipid Antibody Testing: The hallmark of APS diagnosis is the presence of antiphospholipid antibodies in the blood. These antibodies are detected through specific laboratory tests, including:
- Lupus Anticoagulant Test: This measures the presence of lupus anticoagulant, which is one of the main antiphospholipid antibodies. It’s important to note that the name “lupus anticoagulant” is somewhat misleading, as it can be present in people without systemic lupus erythematosus (SLE).
- Anticardiolipin Antibody Test: This measures the levels of anticardiolipin antibodies in the blood.
- Anti-β2 Glycoprotein I Antibody Test: This measures antibodies against β2 glycoprotein Criteria for Diagnosis: To be diagnosed with APS, certain criteria must be met. These criteria include:
- Presence of at least one clinical event associated with APS, such as a blood clot, recurrent miscarriages, or certain pregnancy complications.
- Detection of antiphospholipid antibodies (lupus anticoagulant, anticardiolipin antibodies, or anti-β2 glycoprotein I antibodies) on two or more occasions at least 12 weeks apart.
Exclusion of Other Conditions: It’s important to rule out other possible causes of the clinical symptoms, as some other medical conditions can mimic APS.
Imaging Studies: Depending on the clinical presentation, imaging studies such as ultrasound, Doppler studies, or imaging of the affected organs (e.g., brain imaging for stroke evaluation) may be performed to assess the extent of any blood clots or damage.
Medical treatment for Antiphospholipid syndrome (APS)
Medical treatment for antiphospholipid syndrome (APS) primarily aims to manage the increased risk of blood clots and prevent complications associated with the condition. The mainstay of treatment typically involves the use of anticoagulant medications. Here are key aspects of medical treatment for APS:
Anticoagulant Therapy: Anticoagulants, also known as blood thinners, are medications that help prevent the formation of blood clots. The choice of anticoagulant and the duration of treatment depend on the individual’s clinical presentation and risk factors. Common anticoagulants used in APS management include:
- Warfarin: This oral anticoagulant is often used for long-term treatment of APS. Regular blood monitoring is necessary to adjust the dosage.
- Low Molecular Weight Heparin (LMWH): LMWH, such as enoxaparin, is often used in the early stages of treatment, during pregnancy, or when warfarin is not suitable.
- Direct Oral Anticoagulants (DOACs): In some cases, DOACs like apixaban or rivaroxaban may be considered, although they are not the first-line treatment for APS.
Monitoring: Regular blood tests to monitor clotting parameters, such as the International Normalized Ratio (INR), are crucial, especially for individuals on warfarin therapy. Monitoring helps ensure that the anticoagulant medication is at the appropriate level to prevent clotting.
Treatment of Acute Clots: If a person with APS develops an acute blood clot, immediate treatment with anticoagulants and, in some cases, additional therapies such as thrombolytics or surgery may be necessary.
Additional Medications: Depending on the clinical presentation, other medications may be prescribed. For example, individuals with APS-related autoimmune disorders like systemic lupus erythematosus (SLE) may receive immunosuppressive drugs to manage their underlying condition.
Pregnancy Management: Pregnant women with APS require specialized care. Treatment may include aspirin, heparin (either LMWH or unfractionated heparin), and close monitoring to reduce the risk of pregnancy complications.
Lifestyle Modifications: Encouraging a healthy lifestyle, including smoking cessation, weight management, and regular physical activity, can help reduce cardiovascular risk in individuals with APS.
Management of Associated Conditions: Managing comorbid conditions and risk factors, such as hypertension, diabetes, and hyperlipidemia, is essential for overall health and minimizing additional cardiovascular risk.
Thromboprophylaxis: In certain situations, individuals with APS may receive prophylactic anticoagulation to prevent blood clots during high-risk periods, such as major surgery or prolonged immobilization.
Physiotherapy Treatment
Physiotherapy also known as physical therapy, can play a supportive role in the management of certain aspects of antiphospholipid syndrome (APS). While physiotherapy doesn’t directly treat the underlying autoimmune condition, it can address specific symptoms and issues associated with APS. The following are some advantages of physical therapy:
- Deep Vein Thrombosis (DVT) Management: Physiotherapists can provide guidance on exercises and activities that promote blood circulation in individuals at risk of DVT. This may involve techniques to improve calf muscle pumping action and reduce the risk of clot formation, especially during periods of immobility.
- Pulmonary Rehabilitation: In cases where APS has led to pulmonary embolism or lung involvement, physiotherapists can assist with breathing exercises, chest physiotherapy, and techniques to improve lung function and reduce breathlessness.
- Mobility and Joint Health: APS can lead to joint pain and inflammation. Physiotherapists can design exercise programs to help maintain joint mobility, reduce pain, and improve overall physical function.
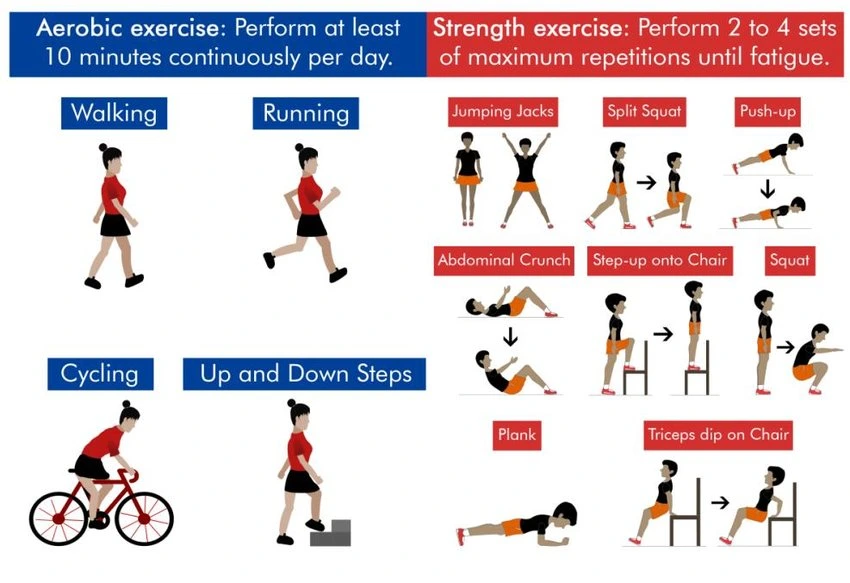
- Strength and Conditioning: For individuals with APS, especially those on long-term anticoagulant therapy, maintaining overall physical fitness and strength is essential. Physiotherapists can create customized exercise programs to improve muscle strength and cardiovascular fitness while considering individual health needs.
- Pain Management: Physiotherapists can employ various modalities, such as heat or cold therapy, manual techniques, and therapeutic exercises, to help manage pain associated with APS.
- Balance and Fall Prevention: Some individuals with APS may experience neurological symptoms or take medications that affect balance. Physiotherapists can work on balance training and fall prevention strategies to reduce the risk of accidents.
- Education: Physiotherapists can educate individuals with APS on lifestyle modifications, proper body mechanics, and exercises that can support their overall well-being and reduce the risk of complications.
Exercise
Exercise is an important component of maintaining overall health and well-being, but it’s crucial to approach exercise with caution if you have antiphospholipid syndrome (APS) due to the increased risk of blood clots. Here are some exercise guidelines for individuals with APS:
- Consult Your Healthcare Provider: Before starting any exercise program, consult your healthcare provider, preferably one familiar with APS or a physiotherapist.
- Low-Impact Activities: Choose low-impact exercises that are gentle on your joints and reduce the risk of injury. Examples include walking, swimming activity, stationary cycling, and water aerobics. These activities can help improve cardiovascular fitness and joint mobility without putting excessive strain on your body.
- Warm-Up and Cool Down: Always warm up your muscles with light stretching or gentle movements before starting any exercise routine. Likewise, cool down with stretching exercises to prevent muscle stiffness.
- Strength Training: Incorporate strength-training exercises using light weights or resistance bands. Focus on all major muscle groups, but avoid heavy lifting that may strain your muscles or increase the risk of injury.
- Flexibility Exercises: Stretching exercises can improve joint flexibility and reduce the risk of joint pain. Perform gentle stretching for various muscle groups, holding each stretch for 20-30 seconds.
- Balance Exercises: Balance training can be essential, especially if you have neurological symptoms or take medications that affect your balance. Simple balance exercises, such as standing on one leg or using a balance board, can help improve stability.
- Avoid Prolonged Immobility: If you need to sit or stand for extended periods due to work or travel, take frequent breaks to move around and promote circulation.
- Hydration: Stay well-hydrated during exercise to prevent dehydration, which can increase the risk of blood clot formation.
- Listen to Your Body: Pay close attention to how your body responds during exercise. If you experience unusual pain, shortness of breath, or other concerning symptoms, stop exercising and seek medical attention.
- Medication Considerations: If you are on anticoagulant therapy, take your medications as prescribed and follow your healthcare provider’s recommendations regarding exercise and potential interactions.
- Timing of Medications: If you are taking blood thinners, be mindful of the timing of your medications in relation to exercise. You may need to adjust your schedule to ensure the medication’s effectiveness during your workout.
- Avoid High-Risk Activities: Steer clear of high-impact activities, contact sports, and exercises that involve abrupt, jerky movements, as these can increase the risk of injury and clot formation.
- Swimming: Provides a full-body workout while being gentle on the joint area.
- Stationary Cycling: Low-impact cardiovascular exercise that can be done indoors.
- Water Aerobics: Combines cardiovascular exercise with the buoyancy of water for added joint protection.
- Walking: A simple and effective way to improve cardiovascular fitness; consider walking on flat terrain or using a treadmill.
Strength Training: – Bodyweight Exercises: Include exercises like squats, lunges, push-ups, and modified planks.
- Resistance Bands: Use resistance bands for light resistance exercises targeting different muscle groups.
- Yoga: Incorporate yoga poses that focus on building strength and flexibility.
Flexibility and Stretching:

- Yoga: Offers a wide range of gentle stretches that can improve flexibility.
- Tai Chi: A low-impact martial art that incorporates slow, flowing movements and stretches.
- Pilates: Includes exercises that enhance flexibility and core strength.
Balance and Coordination: – Tai Chi is known for its balance-enhancing benefits.
- Standing on One Leg: A simple exercise you can do anywhere to improve balance.
- Balance Board Exercises: Using a balance board or wobble board can challenge your balance and stability.
Breathing Exercises:
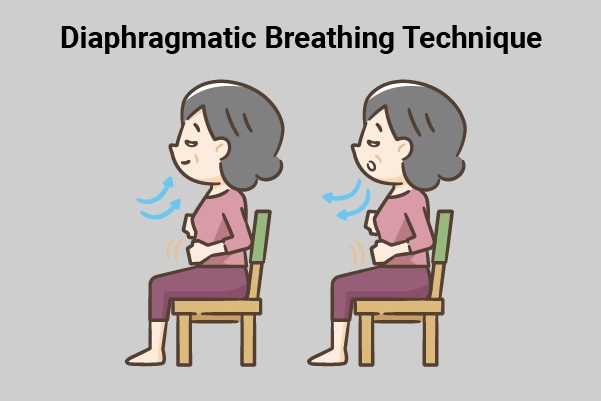
- Deep Breathing: Practice deep, diaphragmatic breathing to improve lung capacity and relaxation.
- Breathing Exercises for Relaxation: Techniques like the “4-7-8” breathing pattern can help manage stress and anxiety.
Mind-Body Activities: – Meditation: Aids in body relaxation and stress reduction.
- Mindfulness: Focuses on being present in the moment and can help manage pain and improve mental well-being.
Low-Impact Group Fitness Classes:
- Look for classes like low-impact aerobics, gentle dance, or chair-based exercise classes, which are often available at fitness centers and community centers.
Chair Exercises:
- Seated leg lifts: Sit in a sturdy chair and lift your legs one at a time, straightening them as much as possible.
- Seated marching: While seated, lift your knees one at a time as if you’re marching in place.
Stability Ball Exercises:
- Seated stability ball exercises: Perform gentle exercises while seated on a stability ball to improve core strength and balance.
- Wall squats: Stand with the stability ball against a wall, lean against it, and perform partial squats for leg strength.
Resistance Band Exercises:
- Seated rows: Attach a resistance band to a secure anchor and perform seated rowing motions to strengthen the upper back and shoulders.
- Seated leg extensions: Secure one end of the resistance band to a chair leg and loop the other end around your ankle for seated leg extensions.
Low-Impact Dance:
- Low-impact dance classes or dance-style workouts, such as Zumba Gold or ballet-inspired workouts, can be enjoyable and provide cardiovascular exercise without high-impact movements.

- Water walking: In a pool, walk forward and backward in chest-deep water for a low-impact cardiovascular workout.
- Water resistance exercises: Use water resistance for gentle strength training by performing movements like leg lifts or arm curls in the pool.
Gentle Stretching:
- Chair yoga: Engage in yoga exercises adapted for seated positions and gentle stretches that can be done while sitting.
- Tai Chi for Arthritis: Tai Chi routines designed for arthritis are slow and gentle, promoting flexibility and balance.
Recumbent Cycling: – Use a recumbent exercise bike, which provides back support and allows for a comfortable seated position while cycling.
Breathing and Relaxation: – Deep breathing exercises and progressive muscle relaxation techniques can help manage stress and improve relaxation.
Mindful Walking:
- Take short walks outdoors or indoors while focusing on your breathing and surroundings, which can have a calming effect.
Stationary Arm Bike:
- Consider using a stationary arm bike for upper-body cardiovascular exercise, which is gentler on the legs.
Surgery
surgery for individuals with antiphospholipid syndrome (APS) requires careful consideration and coordination with a healthcare team due to the increased risk of blood clots and other complications associated with the condition. Here are some important points to keep in mind regarding surgery and APS:
- Preoperative Evaluation: If you have APS and require surgery, your healthcare provider will conduct a thorough preoperative evaluation to assess your overall health and the specific risks associated with surgery. This evaluation may include blood tests to check clotting parameters and antiphospholipid antibody levels.
- Medication Management: If you are taking anticoagulant medications (blood thinners) for APS, your healthcare provider will discuss the management of these medications leading up to and during surgery. In some cases, anticoagulants may need to be temporarily discontinued or adjusted to reduce the risk of excessive bleeding during surgery.
- Prophylactic Measures: Depending on your individual risk factors and the type of surgery, your healthcare team may recommend prophylactic measures to prevent blood clots during and after surgery. This could include the use of compression stockings or intermittent pneumatic compression devices.
- Thromboprophylaxis: In certain high-risk situations, such as major orthopedic surgeries or surgeries with a high risk of clotting complications, your healthcare provider may consider more aggressive thromboprophylaxis, which involves the use of blood thinners during and after surgery.
- Consultation with Specialists: For complex surgeries or individuals with multiple medical conditions, a team of specialists, including hematologists, rheumatologists, and surgeons, may collaborate to develop a comprehensive surgical plan that takes APS and its associated risks into account.
- Postoperative Monitoring: After surgery, close monitoring for clotting complications is essential. This may involve frequent assessment of clotting parameters, such as the International Normalized Ratio (INR), and vigilant observation for signs of deep vein thrombosis (DVT) or pulmonary embolism (PE).
- Recovery and Rehabilitation: Following surgery, individuals with APS may have specific needs for rehabilitation and recovery. This may include measures to prevent joint stiffness, deep breathing exercises to reduce the risk of lung complications, and gradual reintroduction of physical activity under medical guidance.
Prevention
Preventing complications and managing antiphospholipid syndrome (APS) primarily involves a combination of medical interventions, lifestyle modifications, and regular monitoring. Here are key strategies for prevention:
Anticoagulant Therapy: The cornerstone of preventing blood clots in individuals with APS is the use of anticoagulant medications, often prescribed by a healthcare provider. These medications, such as warfarin or low molecular weight heparin (LMWH), help reduce the risk of clot formation.
Compliance with Medications: It’s crucial to take prescribed anticoagulant medications as directed by your healthcare provider. Regularly monitoring and adjusting the dosage, typically indicated by the International Normalized Ratio (INR), is essential when taking warfarin.
Consultation with a Specialist: Work closely with healthcare specialists, such as hematologists, rheumatologists, and obstetricians, who are experienced in managing APS. They can provide guidance on medication management and preventive measures.
Regular Monitoring: Maintain regular follow-up appointments with your healthcare provider to monitor your condition and medication effectiveness. Blood tests may be necessary to assess clotting parameters and antibody levels.
Lifestyle Modifications: Adopt a healthy lifestyle to reduce cardiovascular risk factors:
- Quit Smoking: Smoking is a significant risk factor for clot formation. Seek support to quit smoking if the patient is a smoker.
- Maintain a Healthy Weight: Obesity is associated with an increased risk of clotting and cardiovascular problems. To achieve a healthy weight, combine exercise and proper eating.
- Exercise Regularly: Engage in regular, low-impact exercises to improve cardiovascular health and maintain muscle strength. Consult your healthcare provider or a physiotherapist for guidance on appropriate exercises.
- Balanced Diet: Consume a balanced diet rich in vegetables, fruits, whole grains, and lean proteins. Limit saturated fats and sodium.
Pregnancy Management: If you are pregnant or planning to become pregnant, consult with an obstetrician experienced in APS management. Specialized care, including the use of anticoagulants and antiplatelet medications, may be required to reduce the risk of pregnancy complications.
Avoid High-Risk Situations: Be cautious in situations that may increase the risk of clot formation, such as prolonged immobilization, long-distance travel, and major surgeries. If you need to undergo surgery or an extended period of immobility, consult with your healthcare provider for appropriate preventive measures.
Medication Interactions: Be aware of potential interactions between anticoagulant medications and other drugs, including over-the-counter medications and herbal supplements. Always inform healthcare providers about all medications you are taking.
Patient Education: Educate yourself about APS, its symptoms, and potential complications. Knowing the signs of clot formation or other APS-related problems can enable you to seek prompt medical attention.
Psychosocial Support: Managing a chronic condition like APS can be challenging. Seek emotional support from family members, best friends, or support groups. Managing stress through relaxation techniques and mindfulness can also be helpful.
Complications
Antiphospholipid syndrome (APS) can lead to various complications due to its primary effect of increasing the risk of blood clot formation. These complications can be serious and impact various parts of the body. Here are some common complications associated with APS:
- Deep Vein Thrombosis (DVT): DVT is the formation of blood clots in deep veins, often in the legs. These clots can block blood flow and lead to pain, swelling, and even pulmonary embolism (a clot that travels to the lungs).
- Pulmonary Embolism (PE): PE occurs when a clot from another part of the body, often a DVT, travels to the lungs, causing symptoms like chest pain, shortness of breath, and coughing up blood.
- Stroke: APS can increase the risk of clot formation in the arteries supplying the brain, potentially leading to a stroke. This can result in neurological deficits, such as paralysis or speech problems.
- Myocardial Infarction (Heart Attack): APS can lead to blood clots in the coronary arteries, causing reduced blood flow to the heart muscle and a heart attack.
- Recurrent Miscarriages: APS is a common cause of recurrent miscarriages, particularly in the second or third trimester of pregnancy. It can also lead to other pregnancy complications like preeclampsia and fetal growth restriction.
- Kidney Damage: Clot formation in the blood vessels of the kidneys can lead to kidney dysfunction or even kidney failure.
- Arterial Thrombosis: APS can cause clots to form in arteries throughout the body, potentially affecting various organs and tissues, including the skin, eyes, and extremities.
- Neurological Symptoms: APS-related clotting in smaller blood vessels of the brain can result in neurological symptoms such as headaches, migraines, memory problems, and cognitive impairment.
- Skin Manifestations: Livedo reticularis, a mottled discoloration of the skin, is a common skin condition associated with APS. Skin ulcers may also develop.
- Heart Valve Abnormalities: APS can lead to heart valve disease, which may require surgical intervention to repair or replace affected valves.
- Gastrointestinal Issues: Rarely, APS can cause abdominal pain, bowel infarction (loss of blood supply to the intestines), and other gastrointestinal complications.
- Thrombocytopenia: Some individuals with APS may experience a low platelet count, increasing the risk of bleeding.
Home advice
Managing antiphospholipid syndrome (APS) often involves a combination of medical treatments and lifestyle adjustments. Here are some home advice and self-care strategies that can complement your overall APS management:
- Medication Adherence: Ensure you take your prescribed medications, such as anticoagulants (blood thinners), as directed by your healthcare provider. Follow the recommended dosages and monitoring schedules closely.
- Regular Monitoring: If you are taking anticoagulant medications like warfarin, stay committed to regular monitoring of clotting parameters, such as INR (International Normalized Ratio), to maintain therapeutic levels and minimize risks.
- Stay Informed: Educate yourself about APS, its symptoms, and potential complications. Being informed enables you to recognize warning signs and seek prompt medical attention when necessary.
- Healthy Diet: Adopt a healthy diet that emphasizes lean meats, whole grains, fruits, vegetables, and low-fat dairy. Limit saturated fats, sodium, and processed foods. A heart-healthy diet can help reduce cardiovascular risks associated with APS.
- Hydration: Drink enough water to maintain proper hydration throughout the day. Proper hydration is essential for maintaining circulation and preventing blood clots.
- Physical Activity: Engage in regular, low-impact exercise as recommended by your healthcare provider or physiotherapist. Activities like walking, swimming, and gentle yoga can help improve cardiovascular fitness and joint mobility.
- Smoking Cessation: If you smoke, stop immediately. Smoking is a significant risk factor for clot formation and cardiovascular disease.
- Stress Management: Practice stress-reduction techniques such as deep breathing exercises, meditation, mindfulness, or relaxation exercises. Chronic stress can potentially worsen autoimmune conditions like APS.
- Compression Stockings: If advised by your healthcare provider, wear compression stockings to improve circulation and reduce the risk of deep vein thrombosis (DVT) if you have mobility restrictions or travel long distances.
- Avoid Prolonged Immobility: If you need to sit or stand for extended periods, take breaks to move around and prevent blood from pooling in your legs.
- Medication Interactions: Be cautious with over-the-counter medications and supplements, as they can interact with anticoagulant medications. Always inform healthcare providers about all medications and supplements you are taking.
- Pregnancy Planning: If you are planning to become pregnant or are already pregnant, consult with an obstetrician experienced in managing APS. Specialized care and medications may be necessary to reduce pregnancy-related risks.
- Support Groups: Consider joining APS support groups or seeking emotional support from family and friends. Managing a chronic condition can be challenging, and sharing experiences with others can be beneficial.
- Regular Check-Ups: Continue with regular follow-up appointments and monitoring with your healthcare provider to assess your APS status and medication effectiveness.
FAQ
APS is an autoimmune disorder in which the immune system mistakenly produces antibodies that attack phospholipids, a type of fat found in cell membranes and in the blood.
Antiphospholipid antibodies are autoantibodies that target phospholipids. They are a hallmark of APS and contribute to increased blood clotting and other symptoms.
Symptoms can vary but often include blood clots, recurrent miscarriages, neurological symptoms, skin conditions, and cardiovascular issues.
The exact cause is not fully understood, but it is considered an autoimmune disorder where the immune system mistakenly attacks phospholipids. It can occur on its own (primary APS) or in conjunction with other autoimmune conditions (secondary APS).
Yes, APS can lead to recurrent miscarriages, stillbirths, and other pregnancy complications. Pregnant women with APS require specialized care and often receive blood-thinning medications.
Yes, lifestyle modifications such as maintaining a healthy diet, regular exercise, and smoking cessation can reduce cardiovascular risks associated with APS.
Yes, APS can affect various organs, including the brain (leading to stroke or cognitive issues), heart (increasing the risk of heart attack), kidneys (causing kidney dysfunction), and skin (resulting in skin conditions like livedo reticularis).
There may be a genetic component to APS, but it is not typically inherited in a straightforward manner like some other genetic disorders.