Superior Rectus Muscle
Table of Contents
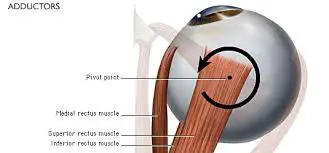
Superior Rectus Muscle Anatomy
The superior rectus (SR) muscle is one of six extraocular muscles that control eye movement. It is also known as the elevator oculi muscle. This muscle is innervated by the superior division of the oculomotor nerve (CN III). The SR originates from the common tendinous ring (annulus of Zinn) and inserts into the superior surface of the sclera, about 8 mm posterior to the limbus.
- Superior rectus muscle is a muscle in the orbit.
- It is one of the extraocular muscles. This group of muscles helps in the movement of the eyes within the orbit. Extraocular muscles are the superior rectus, inferior rectus, medial rectus, lateral rectus, superior oblique, and inferior oblique muscles. All these muscles can be divided into four recti and two oblique muscles.
- All four recti muscles arise from a connective tissue ring called the annulus of Zin (common tendinous ring). This is located at the apex of the orbit, surrounding the optic canal.
- This muscle nerve is supplied by the superior division of the oculomotor nerve (Cranial Nerve III).
- In the primary position (looking straight ahead), the superior rectus muscle’s primary function is elevation, while it also helps in intorsion and adduction.
Origin
- The superior rectus originates from the common tendinous ring (annulus of Zinn) to the superior aspect of the eyeball, just posterior to the corneal limbus (corneoscleral junction) and The largest part of the superior rectus originates from the superior portion of the common tendinous ring or superolaterally to the optic canal and smaller portion arises from the dura mater that surrounds the optic nerve (CN II).
Insertion
- Superior rectus muscle insertion is anterolateral, crossing over the eyeball equator to reach and insert onto the anterior half of the sclera superiorly.
Nerve Supply
- Oculomotor nerve
Blood Supply
- The superior rectus muscle is vascularized by the ophthalmic artery and its supraorbital branch.
- The lacrimal artery, infraorbital artery, and muscular branches of the ophthalmic artery serve as the main sources of blood supply for all of the extraocular muscles.
- The ophthalmic artery has two muscular branches:
- Superior Branch
- Inferior branches.
- Similar to the artery system, venous drainage empties into the superior and inferior orbital veins. The four vortex veins are usually found on the lateral and medial sides of the superior and inferior rectus muscles.
- The orbital venous system receives the drain from these vortex veins.
Actions:
- Superior rectus muscle movement in several planes like elevation in the transverse plane, adduction in the vertical plane, and internal rotation (intorsion) in the anteroposterior plane.
- These contrasting movements are achieved because the muscle fibers course obliquely at a 23-degree angle with the median plane of the eye.
- when shifting the gaze upwards, the eyeball can elevate without the movements of adduction and internal rotation because the superior rectus usually contracts together with the inferior oblique muscle.
- whose fibers and pull are oriented in a way to oppose the adduction and internal rotation produced by the superior rectus and decrease them to a minimum. Thus, the end result is an elevation of the eyeball.
superior rectus muscle Video
Relations:
- The superior rectus muscle is located inferolaterally to the superior oblique and inferomedially to the levator palpebrae superioris muscle.
- The most distal part of the superior rectus muscle runs superficially to the tendon of the superior oblique muscle and the superior branch of the oculomotor nerve (CN III) courses over the proximal third of the muscle inferior surface before it pierces the muscle belly to provide innervation.
- After the insertion of the superior rectus muscle penetrates the fascial sheath of the eyeball (Tenon’s capsule), which in turn reflects back on the muscle’s tendon and creates a thin fascial sleeve.
The muscles of the vertical rectus are the superior and inferior rectus. The horizontal rectus muscles are the medial rectus muscle and lateral rectus muscles. The anterior path of the rectus muscles is initiated posteriorly at the annulus of Zinn.
The rectus muscles insert on the globe at different distances from the limbus. The rectus spiral of Tillaux is formed by drawing a curving line along the insertion locations of the muscles. The medial rectus, inferior rectus, lateral rectus, and superior rectus all insert at different distances from the limbus, starting at the medial aspect of the globe and ending at 5.5 mm, 6.5 mm, 6.9 mm, and 7.7 mm, respectively. Whereas the inferior and superior recti insert along the vertical meridian, the medial and lateral recti insert along the horizontal meridian.
The width of the superior rectus at its globe insertion is 10.6 mm. 5.8 mm is the tendon’s measured length from the origin. The muscle is 41.8 mm long overall.
The proportion of nerve fibers to skeletal muscle fibers is high in extraocular muscles. Other skeletal muscles are 1:50 to 1:125; the ratio is 1:3 to 1:5. Muscle fibers that are both saccadic (fast) and slow tonic (which withstand fatigue) kinds can be found in extraocular muscles, which are specialized forms of skeletal muscle.
Embryology
The primary source of the mesenchyme of the head, which includes the orbit and its structures, is the neural crest and mesoderm cells. While the satellite and connective tissue of the muscles are derived from neural crest cells, the extraocular muscles are derived from the mesoderm. Neural crest cells are also the source of the majority of the orbit’s remaining connective tissue.
Variations
A person may differ greatly in the size of the superior rectus muscle, its insertion location on the globe from the limbus, and other anatomical measures. The distances listed in this article’s descriptions are averages. Ocular misalignment may be caused by congenital variations in the extraocular muscles.
Assessment of Superior Rectus Muscle
During the clinical examination, the superior rectus muscle’s function can be evaluated in addition to that of the other extraocular muscles. The patient can be asked to stare in nine different directions to gauge the movement of the extraocular muscles. The primary gaze comes first, then the secondary positions (up, down, left, and right), and finally the tertiary positions (up and left, up and left, down and right, down and left). By having the patient trace a wide “H” in the air by following the doctor’s finger, the clinician can test these places. To isolate the superior rectus muscle, urge the patient to raise their eye to full abduction.
Additional techniques for testing ocular alignment include dissimilar target tests, corneal light reflexes, cover tests, and dissimilar image tests. Many patients with extraocular muscle anomalies are young children, so the doctor may need to use a variety of cunning techniques to get the youngster to cooperate, like using toys or other things.
Clinical Importance
Superior rectus paralysis
- The decussation of fibers to the superior rectus muscle takes place within the oculomotor nuclear complex, the lesions affecting the nucleus may simultaneously involve the ipsilateral superior rectus subnucleus, as well as the crossing fibers, resulting in bilateral superior rectus palsy.

Neuromuscular control anomalies or abnormalities in binocular vision can lead to strabismus or eye misalignment. Strabismus may be caused by weakness, damage, or paralysis of the superior rectus muscle.
FAQ
The main function of the superior rectus is to raise the eye, which moves the cornea superiorly. The superior rectus forms a 23-degree angle with the visual axis as it runs anteriorly and superiorly over the globe, starting with the annulus of Zinn.
Oculomotor Nerve
One muscle in the orbit is the superior rectus muscle. It is a muscle located outside the eye. The superior division of the oculomotor nerve (III) innervates it. While it also aids in intorsion and adduction, its main purpose in the primary position—looking straight ahead—is elevation.
Here are the steps on how to test the superior rectus muscle:
Have the patient sit upright with their head still.
Request that the patient look directly at your finger.
Slowly move your finger up and out, asking the patient to follow it with their eyes.
Observe the patient’s eye movement. The eye should move smoothly up and out without any hesitation or restriction.
Repeat the test on the other eye.
A number of visual disorders, such as eye discomfort, proptosis (abnormal protrusion of the eye), vertical diplopia (double vision), weakness of elevation, and strabismus (eye turning), are associated with damage to the superior rectus muscle. An issue with the superior rectus muscle may or may not impair visual acuity.
Causes of superior rectus weakness are:
A contralateral midbrain lesion that specifically crosses superior rectus nerve fibers may be the cause of isolated superior rectus palsy.
One of the eye’s extrinsic muscles is the superior rectus. It is a member of the extraocular muscles, situated within the orbit but outside the eyeball. The eyes are moved inside the orbit by this set of muscles.


One Comment