Trigger Point Injection
Table of Contents
Introduction
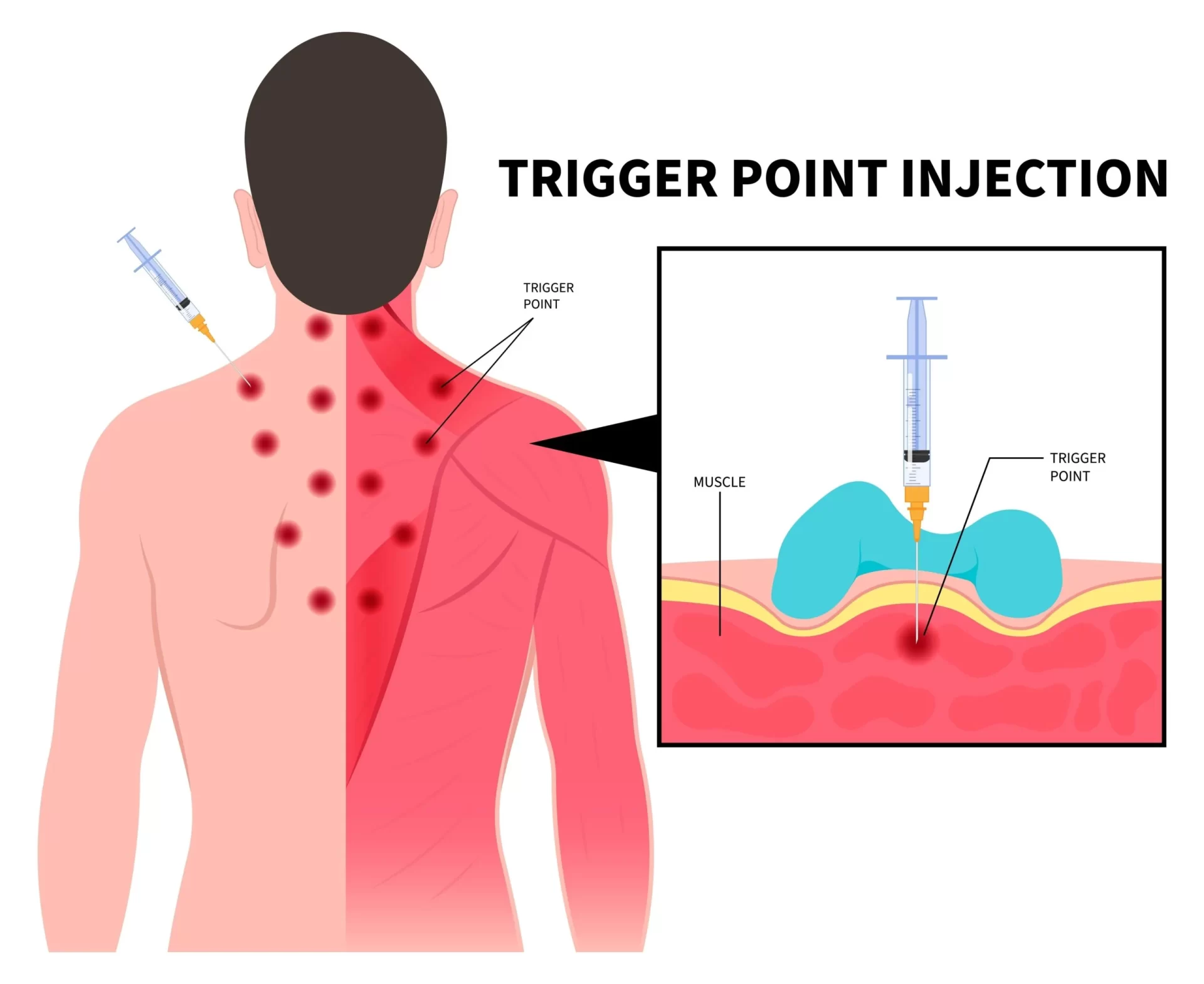
In skeletal muscle, trigger points are concentrated regions of inflammation and spasm. Trigger points are frequently seen in the rhomboid and trapezius back muscles, which are situated in the upper back and behind the shoulder regions. These regions may have trigger points that result in headaches, shoulder pain, and neck pain. Trigger points can also develop in the low back and, less frequently, in the extremities, in addition to the upper spine.
In most cases, the muscle containing the trigger point has a palpable nodule. The region is sensitive, and when pressed, pain often spreads to the surrounding area from the trigger point. Chronic musculoskeletal conditions like fibromyalgia, myofascial pain syndrome, neck pain, and low back pain frequently have trigger points associated with them. Additionally, TMJ discomfort and tension headaches may cause them. Trigger points can arise from acute trauma or from recurrent mild injuries.
What is a trigger point?
In order to relax muscles and reduce pain, trigger point injections work by injecting a local anesthetic—sometimes in conjunction with a steroid medication—into a trigger point. A trigger point is a sore spot on the muscle caused by the fascia (also known as myofascia), the surrounding tissue, contracting and adhering to itself.
A “knot,” or protrusion under the skin that can produce pain in the affected location, is a common identification for trigger points. Referred pain is the term for the situation where a trigger point affects a nearby nerve and thus produces pain in a different part of the body.
In order to deactivate trigger points and quickly alleviate myofascial pain syndrome symptoms, trigger point injections are a useful therapy option.
There are other techniques to address trigger points, such as spray and stretch, ultrasound, manipulative therapy, and trigger point injection.
Not every trigger point needs to be injected or needled. Physical therapy is effective in treating many active trigger points, particularly in the early phases of trigger point production. Nonetheless, trigger point injection and needling work well for treating persistent trigger points.
What is a trigger point injection?
Injections of trigger points, particularly in the neck, shoulder, arms, legs, and lower back, can help relieve myofascial pain.
Your muscles may have uncomfortable “knots” in them that are extremely sensitive to pressure or touch. They can develop as a result of repeated microtrauma or acute trauma that stresses the muscle fibres. It results in the contraction of the muscle fibres becoming trapped. When you rub a muscle, these knots may occasionally be felt.
A tender place and a trigger point are not the same thing. Injections into trigger points are usually limited to locations that are both tight and refer to pain. Referred pain occurs when a body part induces pain in another part of the body, such as down a limb.
Wet needling is another term for trigger point injections. Frequently, anesthetics like lidocaine are used to numb the region, or a corticosteroid to help with pain relief.
Local anaesthetic injections with or without corticosteroids, botulinum toxin, or no injection material are frequently used in trigger point injection procedures.
A mixture of anesthetics, a corticosteroid (cortisone medicine) alone or combined with lidocaine, or an anesthetic such bupivacaine (Marcaine) or lidocaine (Xylocaine) may be injected. At times, the trigger point is simply punctured with a needle; no medication is given. This is called “dry needling,” and it might be beneficial. The trigger point is rendered dormant by the injection, which also relieves discomfort.
For certain patients, trigger point injections (TPI) may be an effective method for managing pain. Trigger point injections (TPI) are used to treat painful muscular locations that include knots in the muscle caused by the muscle refusing to relax. Often, these knots are felt beneath the epidermis. Referred pain, or pain perceived in a different area of the body, can result from trigger points irritating the nearby nerves.
Signs and symptoms
Patients with symptoms and examination results compatible with active trigger points may consider trigger point injections. Clinically asymptomatic, latent trigger sites don’t need to be treated. There should only be a certain number of trigger locations that are suitable for injection.
Injections are not appropriate for treating conditions like endocrine disorders or fibromyalgia that cause widespread pain complaints. Trigger-point injections should not be considered until treatment is recommended for fibromyalgia or endocrine disorders. Furthermore, since people with fibromyalgia may also have trigger points for myofascial pain, the presence of discomfort on its own is not a sign that a patient needs a trigger point injection.
When considering indications for injections, it is not always required to have the standard clinical examination findings of a taut band with local twitch response and referral pain pattern. To support trigger point injections in the overall clinical setting, tender spots found in typical trigger point locations that correspond with the patient’s symptoms and a “jump sign” are sufficient.
What Takes Place When You Inject a Trigger Point?
In the TPI process, a tiny needle is inserted by a medical expert into the patient’s trigger point. In addition to saline or a local anaesthetic, the injection could also contain a corticosteroid. The injection also lessens discomfort by normalizing the trigger site.
It is frequently possible to provide sustained relief with a brief course of therapy. Injections usually take a few minutes to administer at a physician’s office. In a single visit, multiple sites could be injected. In cases where a patient is allergic to a particular drug, a medication-free dry-needle approach may be employed.
Which physicians perform trigger point injections?
Physicians who specialize in physical medicine and rehabilitation, rheumatologists, and pain management routinely perform trigger point injections. Trigger-point injections are administered by certain internists, family practitioners, general practitioners, and neurologists.
Certain types of chronic muscle discomfort may be treated with trigger point injections. You could feel a little tender or sore after your injections, but you can immediately resume your regular activities.
Trigger points are tight spots of muscle beneath the skin that can be released with an injection. This brief process is usually carried out at a physician’s office.
Following trigger point injections, you can get right back to your regular activities. The majority of medical experts give an anesthetic during the injection, although there may still be some soreness at the injection site after your visit. The anaesthetic’s tingly, numb sensation can last for several hours.
Injections at trigger points are secure and efficient. They can provide more durable pain relief for some people, and last for several weeks or months.
Injections of trigger points can alleviate pain associated with a variety of trigger point-related diseases. Among them are:
- Tension headache
- Tinnitus
- Myofascial pain syndrome
- persistent musculoskeletal pain
- Decreased range of motion in the affected limbs
- low back pain
- Joint pain
- The process is also applied to long-term musculoskeletal disorders.
What is the purpose of trigger point injections?
The injections of trigger points are used by medical professionals to treat myofascial pain. Muscle is referred to as “myo,” and fascia as “fascial.” The thin, white connective tissue that envelops each muscle in your body is called fascia.
One or more trigger points are typically the source of pain and discomfort in myofascial pain. Trigger points are little lumps, nodules, or knots in your muscles that feel rough to the touch.
Although trigger points can form in any muscle, the following are the most often treated muscle groups with trigger point injections:
- Masseter (a muscle in the jaw).
- Levator scapulae (a muscle on the sides of the neck).
- Gluteus medius (a muscle in the hip).
- Quadratus lumborum (a deep muscle present in the lower back).
- Trapezius (the muscle extending over the back of the neck and shoulders).
- Sternocleidomastoid (a muscle placed near the front of the neck).
- Temporalis (a muscle on both sides of the head).
- Certain kinds of discomfort or problems can be brought on by trigger points. For example, tension headaches may be brought on by trigger points that impact your trapezius muscle. The piriformis muscle, which is located in your buttocks, can impinge on your sciatic nerve and result in piriformis syndrome, which a trigger point can bring on. It hurts your buttocks and sends numbness down the back of your leg.
For whom is a trigger point injection necessary?
In case your trigger point pain has not improved after trying heat therapy, myofascial release, massage therapy, over-the-counter pain medication, or physical therapy, you might need to consider a trigger point injection.
To relieve the discomfort, doctors usually combine physical therapy and stretching exercises with trigger point injections.
This approach can be especially helpful for patients whose severe pain prevents them from doing physical therapy or stretching after a trigger point injection. Injection of trigger points may enhance the efficacy of physical therapy.
Before recommending a trigger point injection, your doctor must conduct a comprehensive physical examination and rule out any further potential reasons for your discomfort, such as:
- Straining of muscles.
- Structural causes of pain.
- Back pain is brought on by problems with your spine, such as spinal stenosis, Herniated disks, or degenerative arthritis.
- Radiculopathy refers to pinched nerve discomfort.
To what extent do trigger point injections occur?
About 85% of people will have trigger points and myofascial pain at some point in their lives.
Regular diagnosis and treatment of myofascial pain by numerous primary healthcare physicians and pain specialists may involve trigger point injections, physical therapy, and stretching exercises.
When is the trigger point injection used?
Numerous muscle groups, particularly those in the arms, legs, lower back, and neck, can be treated with TPI. TPI is also useful in the treatment of fibromyalgia and tension headaches. The method is also used to treat myofascial pain syndrome, which is a persistent pain that affects the tissue around muscles and is not relieved by other means. Studies are still being conducted to determine whether TPI is beneficial in treating myofascial pain.
Trigger point injections are a medical treatment used by doctors to address musculoskeletal disorders and chronic muscle discomfort. They may have adverse consequences, such as transient vertigo and numbness.
Numerous things might cause muscular pain, such as sleeping in the incorrect position or injuring big muscle groups after a strenuous weightlifting session.
A few days of rest will often alleviate many types of muscular discomfort, but those with chronic or severe pain may need to see a doctor.
The quality of life and an individual’s capacity to operate can both be significantly impacted by chronic muscle discomfort. Injectable trigger points may provide instant relief for those with chronic pain in the muscles.
Uses:
As with the illnesses listed below, trigger point injections can help reduce pain brought on by disorders affecting the musculoskeletal and neurological systems.
Myofascial pain syndrome:
Injections into trigger points may be able to alleviate the symptoms of myofascial pain syndrome, a persistent pain disorder affecting the surrounding tissue and muscles.
Trigger points in myofascial pain syndrome cause pain perception in seemingly unrelated body areas. We refer to this occurrence as referred-to pain.
By relaxing the afflicted muscles, trigger point injections help lessen localized muscular pain. According to research, the injections also disrupt the nerve communication pathways that lead to referral pain.
Myofascial trigger points may result from the following causes:
- damage or stress to a muscle
- repeated movements
- poor posture
- psychological stress
A patient with myofascial pain may also feel as follows in addition to referred pain:
- Discomfort in particular areas of a muscle
- Pain that gets worse when the afflicted muscle is moved or stretched
- A muscle knot that the person can feel with their touch
- Muscle weakness or stiffness
- A restricted range of motion
- Fibromyalgia:
- Similar in some ways to arthritis, fibromyalgia is a chronic pain syndrome that affects the soft tissues rather than the joints.
- Fibromyalgia’s precise etiology is yet unknown; however, potential risk factors include:
- A medical or psychological trauma history; an autoimmune disease history, such as lupus or rheumatoid arthritis
- physical or mental stress
- a history of fibromyalgia infections in the female family
- infections
- Female
- Symptoms of fibromyalgia include:
- Pain and stiffness throughout the body
- Headaches
- The hands and feet are numb or tingling.
- Digestive problems
- Poor sleep and daytime fatigue
- Difficulty concentrating
- Symptoms of depression or anxiety
In the past, physicians identified fibromyalgia in patients who complained of pain or soreness in particular body trigger points.
Fibromyalgia is characterized by broad, or systemic, pain as opposed to the localized muscle pain that myofascial pain syndrome generates.
This implies that neurological issues affecting the brain’s processing of sensory data are the source of fibromyalgia discomfort.
Having said that, there are similarities in the pain profiles caused by myofascial trigger points and fibromyalgia, and some researchers think that myofascial trigger points are a factor in fibromyalgia pain.
Headaches:
The American Migraine Foundation states that trigger points in the head, neck, and shoulders can aggravate tension-type headache conditions as well as migraines.
Researchers compared the presence of myofascial trigger points in 20 healthy individuals without migraine versus 20 physiotherapy students with episodic migraine in a 2014 paper.
In the migraineurs, the researchers discovered a notably greater quantity of myofascial trigger sites.
In a 2016 study, the authors looked at the connection between pressure pain sensitivity and myofascial trigger points in patients with tension-type headaches, either episodic or chronic.
Pressure pain sensitivity was higher in those with more myofascial trigger points than in those with less points. The results imply that the strength of certain kinds of headaches is influenced by myofascial trigger points.
Advantages:
Trigger point injections are a typically safe option for those who have been experiencing pain associated with trigger points and have not found relief with more conservative therapies, such as over-the-counter pain medication or physical therapy. Additionally, depending on which muscle is affected, trigger point injections can significantly increase muscle functioning and range of motion.
Contraindications
In the event of a localized or systemic infection, trigger sites should not be injected. Patients on anticoagulation or with bleeding issues need to have their injections administered under strict medical supervision. Even while some patients may bleed more frequently, there is still extremely little chance of dangerous haemorrhage.
Avoid administering injections to people who are pregnant or who seem unwell. Patients who are susceptible to infection, such as those who are ill, have diabetes, or are using steroids, should be treated with greater care.
Side effects:
Injecting trigger points may result in a number of short- and long-term adverse effects, such as:
Discomfort or transient numbness in the vicinity of the injection location
skin dimpling or discolouration close to the injection site
feeling faint or lightheaded
hemorrhage
Furthermore, trigger point injections based on anaesthesia may result in myonecrosis, a serious type of muscle injury. It might heal in three to four weeks.
It normally takes a few hours for the injection site’s pain, swelling, and soreness to subside. See your doctor if any adverse effects do not go away within a few weeks.
Risks:
Trigger point injections are generally risk-free and unlikely to have negative effects. The most frequent adverse effect is transient soreness or numbness at the injection site. Your doctor might advise using ibuprofen or acetaminophen to address this. Additionally, ice packs can be applied to injection sites to lessen the possibility of bruises.
Although they are uncommon, trigger point injection complications can include the following:
Bleeding.
Infection at the injection location
Injury to muscles or nerves
Bruises
Reaction to the anaesthetic agent that is allergic.
Harm to a vein or artery
Rarely, gas or air buildup in the area between the lungs and the chest wall can result in the collapse of one or both lungs.
Ultrasound imaging can help minimize a significant trigger point injection issue.
Procedure:
Consent and Patient Education:
After the injections, patients should give their afflicted areas a day or two of rest. At least during the initial phase of muscular discomfort following an injection, strenuous activities should be avoided. Instead of holding the muscle in a fixed, shortened position, the patient is advised to use it to its maximum potential.
The patient needs to learn to identify the actions and postures that cause excessive muscle strain and cause pain. If you want to get long-lasting relief from myofascial pain, you should avoid or modify such activities. Patients need to understand their individual muscle limitations and practice good body mechanics and alignment. Overenthusiasm, continuing to exercise in spite of fatigue or pain, and employing the wrong form are common issues with exercise.
Preprocedural Planning:
To ensure a perfect injection, the needle size matters. For superficial muscles, a 3.8-cm (1.5 in.) needle with a 22 gauge is utilized. If bleeding capillary fragility is a concern, a thinner 25-gauge needle would be better. It takes at least a 21-gauge, 5-cm (2-in.) needle to penetrate dense subcutaneous muscles.
The possibility of the needle breaking off makes it impossible to insert the needle all the way through. In most cases, a 7.6-cm (3-in.) 21-gauge spinal needle can reach trigger points in the deepest muscles; but, on rare occasions, an 8.9-cm (3.5-in.) 22-gauge spinal needle is required. The spinal needle is quite flexible, thus it’s critical to maintain the needle’s straightness.
Equipment:
The following, while not exclusively, is included in the basic equipment needed for trigger point injections:
- Needles and syringes of various sizes
- Povidone-iodine solution or alcohol
- Sterile gauze pads
- Gloves (need not be sterile)
- Lidocaine
- Isotonic saline
- Vapocoolant spray
- Bandages
The following needles may be used:
- Withdrawal of anesthetic solution: :(16-gauge) 1.5-in. needle
- Sternocleidomastoid, Interossei, and Scalenus: 22–25 gauge, 1.5-inch needle
- Temporomandibular joint muscles: 25-gauge 1.5-in. needle
- 22-gauge, 1.5-inch needle for the cervical and suboccipital regions, upper extremities, and ankle and foot
- Extremities: 21 gauge 2.0-in. needle
- Areas of the glutes and back: 20 to 21 gauge, 3-in needle
- Gastrocnemius: 25-gauge: 2.0-in. needle
Patient Preparation
Anesthesia:
Isotonic saline, 1% lidocaine, and 0.5% procaine are injectable solutions. Patients who are allergic to local anesthetics may benefit from dry needling or isotonic saline therapy. In the case of ligamentous trigger points, steroids may be utilized. Additionally, long-acting anesthetics such as bupivacaine have been employed.
Trigger point injections have also been performed using several different drugs, such as corticosteroids, onabotulinum toxin A, and diclofenac. These drugs do, however, have a considerable myotoxic history. Out of all the local injectable anaesthetics, procaine has the lowest myotoxicity.
Positioning:
If at all possible, have the patient lie down (either supine or prone). It is also possible to administer injections while seated. The patient might be put in a reclining position to prevent psychological syncope and promote relaxation so that the trigger points are simpler to locate.
Techniques:
Location of trigger point:
When muscles are palpated for trigger points, a taut band or cord of tense muscle fibers, around 1-4 mm in diameter, may be felt. To find the location designated as the trigger point, the examiner should palpate along this band until they find the site of maximal tenderness. The referred pain pattern is elicited by applying strong pressure.
A “jump sign” or local twitch reaction is frequently elicited upon palpation of an activated trigger point. A jump sign is an involuntary reflex-like movement or leap that the patient exhibits that is consistent, out of proportion to the force applied, and may indicate how irritable the trigger site is.
When a needle is put into the trigger area or the trigger point is rolled under the fingers, a localized twitch reaction occurs in a specific location of the muscle. The muscle fibers in the taut band may jerk or contract noticeably as a result of this twitch, which could last for up to a second.
Injection:
The clinician should isolate the trigger point by pinching between the thumb and index finger or between the index and middle finger with stabilizing pressure to keep the trigger point from rolling away from the advancing needle after locating it and cleaning the surrounding skin with alcohol.
After being implanted 1-2 centimeters away from the trigger point, the needle is advanced into it at a sharp angle of 30º with respect to the skin. Refer to the picture below. The doctor should alert the patient to the likelihood of sudden, intense pain or twitching muscles when the needle makes contact with the trigger point before moving the needle closer to it. In order to prevent intravascular injection, aspirate before injection.
Injection of the trigger point:
A little (0.2 mL) of anesthesia is administered after the needle is inside the trigger point. After withdrawing the needle to the level of the subcutaneous tissue, it is redirected medially, laterally, superiorly, and inferiorly. Until the local twitch reaction is eliminated or the muscle relaxes, the needling and injection procedure is repeated in each direction without removing the needle. [5] The injection locations need to be under pressure.
Postprocedural Care
Stretching:
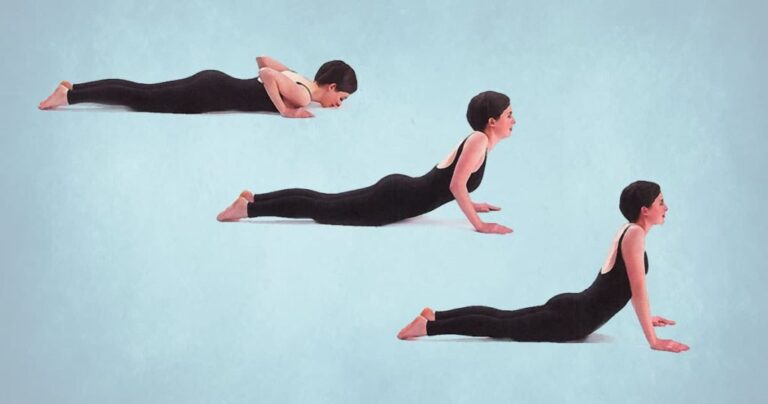
An essential component of treatment is stretching following trigger point injection. The physician should stretch the involved muscles to try to obtain full length.
Before stretching, it may be helpful to apply a few sweeps of vapocoolant spray in a parallel direction over the muscle and its referred pain pattern to relax the remaining tense fibers. After that, all of the injected trigger locations should be covered with a heated pack.
After heat has been applied topically for several minutes, the patient should perform the full active range of motion of the muscle several times to relieve residual stiffness, assess the procedure’s efficacy, and regain awareness of regular muscular activity.
At least during the initial phase of muscular discomfort following an injection, strenuous activities should be avoided. Instead of holding the muscle in a fixed, shortened position, the patient is urged to use it to its full potential.
Exercise:
An essential component of the treatment plan, exercise will ascertain the efficacy of trigger point injection therapy. Muscle conditioning, strengthening, and stretching can all be the focus of an exercise program.
The secret to treating myofascial pain is to get involved in exercises that target and lengthen the affected muscles. Enhancing strength and conditioning lessens the chance of trigger point development.
The patient can move on to strengthening activities once they can tolerate a certain amount of stretch. These can be isometric or isotonic, with isotonic workouts typically being more tolerable. Exercises for strengthening the body should be recommended with a specific amount of repetitions. They must be performed smoothly, gradually, and with breaks in between each repeat.
Exercises for conditioning should be added and performed at least twice a week once tolerated. Swimming, riding, tennis, jogging, and jumping rope are some of these exercises.
Are trigger point injections effective?
For those with persistent muscle pain, trigger point injections may provide faster pain relief and increased range of motion.
But not everyone is affected by these injections in the same manner. After receiving the injections, some patients report significant pain relief right away, while others discover that it may take a few days or weeks for their discomfort to subside.
Injections of trigger points cause no benefit at all for certain individuals.
Investigators of a minor 2019 research on the effects of these injections on patients experiencing pain in their abdominal muscles were examined. Two years following the initial injection, the subjects reported significantly less pain. Five of the subjects needed a second injection, while one did not respond to the medication.
While some patients may benefit greatly from trigger point injections, other experts have discovered that this treatment may not always work.
Complications
Complications may include the following:
- Vasovagal syncope
- Skin infection
- Pneumothorax
- Needle breakage
- Hematoma formation
- The use of sterile procedures usually results in the prevention of infection. In order to prevent complications from pneumothorax, never point a needle towards an intercostal gap. It is best to avoid breaking needles by never inserting them all the way to the hub. Direct pressure should be applied for at least two minutes following injection to prevent hematoma formation.
Summary
Certain types of persistent muscle discomfort may be treated with trigger point injections. You could feel a little tender or sore after your injections, but you can immediately resume your regular activities.
Trigger points are tight spots of muscle beneath the skin that can be released with an injection. Usually, a doctor’s office performs this brief treatment.
Following trigger point injections, you can get right back to your regular activities. The majority of medical experts give an anesthetic during the injection, although there may still be some soreness at the injection site after your visit. The anaesthetic’s tingly, numb sensation may linger for several hours.
Injections at trigger points are secure and efficient. They can provide more durable pain relief for some people. It takes a few weeks or months to complete.
FAQs
After your injection, give the trigger point area one to two days of rest. Steer clear of strenuous tasks like standing for extended periods of time. engaging in vigorous physical activity (such as jogging, running, or aerobics).
For chronic pain problems such as myofascial pain syndrome, fibromyalgia, and tension-type headaches, trigger point injections may be a safe therapy option. Injections into the afflicted muscle are directly administered by a physician or other healthcare professional.
The majority of patients report feeling less pain 24 to 72 hours following trigger point injection therapy. Pain relief often lasts for around one month. Your doctor can suggest further injections if the pain persists after this period to provide long-term pain relief.
When combined with Botox, trigger point injections can guarantee up to 90% alleviation from neck pain. The success rate for pelvic discomfort is about 75%. Patients who have discomfort from myofascial difficulties, spasms related to pinched nerves, and fibromyalgia related to muscular issues are quite satisfied with this therapy approach.
Injections of trigger points can also be utilized to treat fibromyalgia and tension headaches. A TPI might be a long-term fix for your trigger point, or it might merely provide pain relief for several weeks or months.



One Comment