Flexor Pollicis Longus Muscle
Table of Contents
Flexor pollicis longusMuscle Anatomy
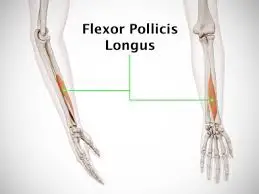
The flexor pollicis longus is a long muscle of the forearm. It belongs to the deep flexors of the forearm, along with the flexor digitorum profundus and pronator quadratus. Since it lies in the forearm but is inserted in the hand, it is also classified as an extrinsic muscle of the hand.
Origin
It originates from the middle anterior surface of the radius and the interosseous membrane.
Insertion
It inserts into the palmar aspect of the base of the distal phalanx of the thumb.
Blood Supply
The Anterior Interosseous artery supplies blood to the muscle.
A branch of the ulnar artery, the anterior interosseous artery supplies blood to the flexor pollicis longus. The common interosseous artery splits off as the ulnar artery passes beneath the ulnar head of the pronator teres muscle. It travels laterally and deeply before abruptly bifurcating into the anterior and posterior interosseous arteries. Between the flexor pollicis longus and flexor digitorum profundus, the anterior interosseous artery and anterior interosseous nerve (AIN) run distally along the interosseous membrane.
Lymphatic drainage
Both deep channels that run beside arteries and superficial channels that run alongside the basilic and cephalic veins are used for the lymphatic drainage of the hand and forearm. Before primarily draining into the axillary or infraclavicular lymph nodes, the lymphatics drain to lymph nodes located within the elbow, such as the cubital and epitrochlear lymph nodes.
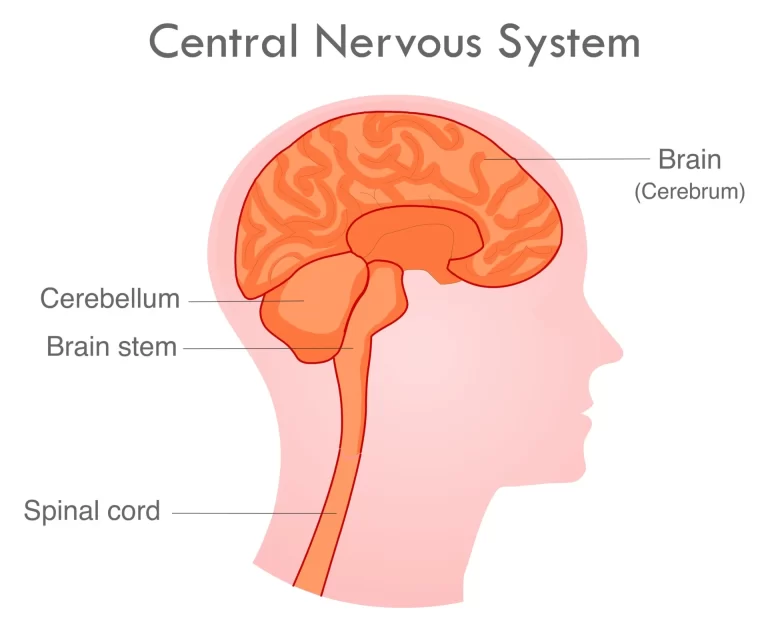
Nerve supply
The anterior interosseous nerve (AIN), a branch of the median nerve, supplies innervation to the FPL muscle. Just proximal to the point where the median nerve crosses over the two heads of the pronator teres muscle, the anterolateral portion of the median nerve gives origin to the AIN. The anterior interosseous artery and the AIN run distally along the interosseous membrane between the FPL and FDP.
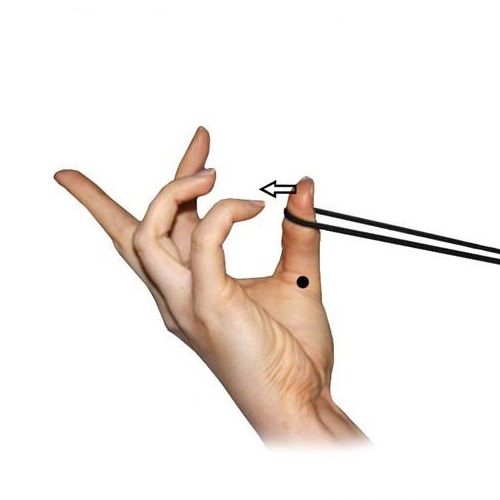
Pronator quadratus, FPL, and FDP are the three deep flexors innervated by the AIN, which also supply sensory innervation to the volar wrist capsule. The patient can be asked to sign “OK” with the thumb and index finger to determine the AIN. The patient will exhibit the inability to flex at the thumb IP joint and the index finger DIP joint in the context of AIN dysfunction, hence “flattening” the typical circular structure of these two digits.
Action
It acts as a flexor of the thumb.
Function
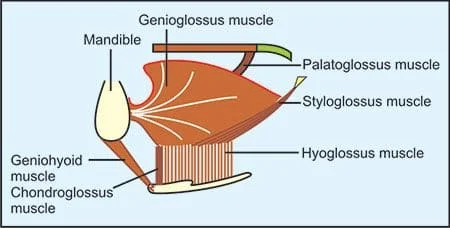
The main function of the flexor pollicis longus is the flexion of the thumb at the interphalangeal joint. Flexor pollicis longus is the only muscle that flexes the interphalangeal joint of the thumb, which makes it vital for activities that require hand gripping.
Flexor pollicis longus also flexes the thumb at the metacarpophalangeal joint and contributes to the flexion of the wrist. This muscle can be easily palpated in the lower third of the forearm when you flex your thumb.
Structure and Function
The thumb’s major flexor, the FPL muscle, provides flexion at the interphalangeal (IP) and metacarpophalangeal (MCP) joints. Furthermore, FPL contributes minimally to wrist flexion and radial deviation.
Just distal to the radial tuberosity, on the volar face of the radius and the surrounding interosseous membrane, FPL develops. Its proximal attachment is located deep and radially to the radial head of the flexor digitorum superficialis (FDS), and distal to the supinator muscle. The muscle tapers into a long, flat tendon that runs straight lateral to the FDS index finger tendon and superficial to the pronator quadratus muscle.
The muscle tapers into a long, flat tendon that runs straight lateral to the FDS index finger tendon and superficial to the pronator quadratus muscle. The FPL tendon passes deep into the transverse carpal ligament (flexor retinaculum) in the carpal tunnel after being covered by the radial bursa’s synovial sheath.
FPL continues between the two sesamoid bones that are located on the volar face of the thumb MCP joint as it travels along the first metacarpal. Before inserting at the volar base of the distal thumb phalanx, the FPL tendon and synovial sheath pass deep to the A1 pulley overlying the thumb MCP joint, the annular variable ligament and oblique ligament of the thumb’s proximal phalanx, and the A2 pulley overlying the IP joint.
The three annular ligaments (A1, Av, and A2) and one oblique ligament make up the thumb’s flexor pulley system. Ligaments are arranged proximally to distally as follows: A1, Av, oblique, A2. The FPL tendon’s most significant pulley is the oblique ligament. A1 and oblique ligament damage will result in the FPL tendon bowstringing. Av ligament absence occurs in 7% of people. Trigger thumb is caused by a dysfunctional excursion of the FPL tendon through the pulley system.
Embryology
Apical ectodermal ridge (AER), zone of polarizing activity (ZPA), and nonridged ectoderm are the three main signaling centers that work in concert to guide the creation of the upper extremity’s proper developmental axis. Four limb buds emerge from the developing embryo’s ventrolateral surface by the end of the fourth week of embryonic development. The limb buds are made up of cuboidal ectoderm that encloses somites and mesenchyme that are derived from the lateral plate mesoderm. Eventually, the lateral plate mesoderm cells will develop into the connective tissue of the extremity. The paraxial mesoderm cells of the somites that have moved into the limb buds are the source of the limb musculature. From somites, muscle progenitor cells move in a certain segmental pattern.
The AER eventually forms when the ectoderm layer at the distal tip of the growing limb enlarges. While more proximal limb cells farther away from the AER start to develop into connective tissue and muscle cells, the AER causes nearby mesenchymal cells to stay undifferentiated and to proliferate.
Chondrocytes generate a basic build of hyaline cartilage by the end of the sixth week of embryonic development. This construct will eventually ossify into the upper extremity bones through a process known as endochondral ossification. The growth of extremity muscles starts in week six and lasts until week eight. All of the extremity’s skeletal structures and muscle groups are developed by the end of the eighth week.
Physiologic Variantions
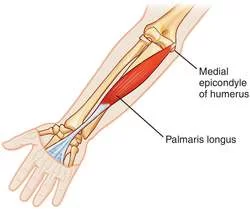
The coronoid process of the ulna, the medial epicondyle of the humerus, or the FDS muscle can all serve as the source of an auxiliary FPL muscle head. The ulnar aspect of the FPL or FDP muscles is where the accessory head is then inserted. Once thought to be an anatomical variation, Gantzer’s muscle is now present in up to two-thirds of the population, according to numerous recent studies. The Gantzer muscle has a number of clinical consequences. The accessory head may compress the median nerve or AIN, depending on its anatomical placement.
The FPL, FDP, and pronator quadratus can all experience symptoms from weakening to paralysis when the AIN is compressed. Numerous thenar and intrinsic hand muscles will become paralyzed in the event of median nerve compression, and sensory deficiencies will also result.
A tendinous relationship between FPL and the FDP of the second digit is known as the Linburg-Comstock phenomenon. The thumb IP joint and the index finger distal interphalangeal joint cannot be separately flexed due to the existence of this tendon slip. Usually, though, this aberration does not cause any symptoms to appear.
Strengthening exercise
To strengthen and hone the function of flexor pollicis longus, sit in a comfortable chair with your hand and palm facing you. Place a band around your thumb, and then move your thumb towards your little finger. Then touch your thumb to each of your fingers in turn while focusing on the flexion of your thumb. Between each finger touch, you should extend your fingers and thumb fully. Repeat this ten times then switch to your other hand.
Stretching Exercise
- Start with your fingers pointing up and your thumb out to one side, then use your other hand to pull your thumb down.
- The palm and thumb comprise a multitude of small muscles, tendons, and ligaments. Do not overstretch this area by applying too much force too quickly.
Related pathology
Trigger thumb is an inability of the FPL tendon to smoothly glide through the pulley system de to pulley stenosis resulting from tenosynovitis, and most commonly involves the A1 pulley.
The presence of the accessory head of FPL has several clinical implications. It can compress the median nerve and anterior interosseus nerve; the later may result in paresis or paralysis of the FDP, FPL, and pronator quadratus, and the former leads to paralysis of some muscles in the thenar compartment as well as sensory deficits.
Volkmann’s contracture, a secondary complication compartment syndrome. that causes muscle and nerve ischemia and or eventual necrosis; as the necrotic tissue recovers, scar tissue contraction results in a shortening of the affected tissue. Flexor digitorum profundus and FPL muscles are usually affected; their noticeable shortening through fibrosis explains the classic flexion deformity of Volkmann’s Ischaemic contracture.
Treatment of acute compartment syndrome and early diagnosis are crucial in preventing Volkmann’s contracture. When evaluating individuals who have injuries that put them at high risk of developing compartment syndrome, the “Six Ps” system can be useful. Among the “Six Ps” are:
Excessive pain during physical examination; pain with passive stretching of the affected compartment
Paresthesia
Paresis
Pallor
Pulselessness
Poikilothermia
Although the diagnosis of compartment syndrome is usually made clinically, it can also be made by measuring the intra-compartmental pressure in certain cases, contingent on the patient’s cognitive state. Revascularization and an immediate open fasciotomy are necessary if the intra-compartmental pressure and diastolic blood pressure differ by less than 30 mm Hg. Untreated acute compartment syndrome causes irreversible damage after 12 hours and nerve ischemia in 30 minutes. Within the first four hours, muscle function will start to decline, and over the following six to twelve hours, permanent muscle damage will occur.
Volkmann’s contracture is classified using two systems: the Tsuge classification system (Mild, Moderate, and Severe based on muscles and nerves involvement as well as presentation) and the Seddon classification system (Grades I–III based on contracture severity).
For mild to grade I contractures, conservative therapy with splinting and stretching is the first line of treatment. For mild contractures, surgery is an option; however, for moderate and severe contractures, surgery is necessary. Muscle slides, free functional muscle transfers, and tendon lengthening are the surgical interventions.
Surgical Considerations
Knife, glass shard, or sharp metal slice injuries are the most common causes of flexor tendon lacerations, including FPL. The complete reconnecting of the severed tendon is referred to as primary tendon repair.
Hand flexor tendon injuries are classified into many zones. Three zones start distally in the thumb: T1 connects the A2 pulley to the FPL tendon insertion, T2 connects the A2 pulley to the A1 pulley, and T3 connects the A1 pulley to the carpometacarpal joint. Zones 4 and 5 cover the area above the wrist and also deal with digit tendon issues.
A whole or partial laceration may occur from damage to the FPL tendon.
Depending on the proportion of the tendon diameter that is damaged, different treatments are used for partial flexor tendon lacerations[12]:
Nonoperative Treatment
suggested when there are just minor lacerations, or when only 50% to 60% of the tendon breadth is involved.
Indications for surgical repair
Over 75% to 80% of the tendon has lacerations in it.
More than 50% to 60% of the tendon has trigger-related lacerations.
The proximal tendon may regress proximally after a full FPL tendon laceration, complicating tendon retrieval.
Primary tendon repair is an option for zone I injuries if the distal tendon stump measures more than 1 cm. To allow for proper healing, the proximal tendon needs to be attached to the cancellous bone if the distal tendon stump is less than 1 cm. Either button anchors or suture anchors are used for the fixing. Direct, end-to-end repair is used in surgical management of zones II through V.
The two tendon ends are anastomosed using a variety of suture techniques. The strength of the tendon after surgery is directly correlated with the number of stitches inside the tendon. To guarantee a solid bond and seamless passage through the flexor tendon pulley system, many strands of epitendinous suture are employed in the most popular core suture repair approaches. As of yet, no research has produced a multi-strand core suture technique that is universally accepted.
The first two weeks following surgery carry the highest risk of tendon re-rupture. It has been demonstrated that using a post-operative splint and early active mobilization can increase range of motion without appreciably raising the risk of re-rupture. The zone of the injury, the amount of time between the injury and operation, postoperative care, and the existence of tendon retraction are some of the variables that can affect the outcome of an FPL tendon surgical repair.
A particular kind of FPL rupture known as a Mannerfelt’s lesion develops in the carpal tunnel as a result of persistent tendon attrition. This gradual weakening is caused by abrasion following the scaphoid’s volar displacement. The most frequent cause of Mannerfelt’s lesion is rheumatoid arthritis, a chronic systemic inflammatory illness that typically results in chronic synovitis, which can cause carpal dislocation. Because it is the most radial tendon in the carpal tunnel, the FPL tendon is the one that is most frequently impacted.
All of the tendons in the carpal tunnel, though, may be impacted. Patients with FPL rupture will have passive thumb flexion but not active IP joint flexion, which helps to distinguish them from trigger thumb patients. Tendon grafting may be utilized to restore the FPL tendon if the rupture is discovered within four to six weeks. A tendon transfer is the required surgical procedure if the issue is not resolved within this time frame, as the muscle would experience myostatic contraction.
FAQ
Flexion of the thumb at the interphalangeal joint is the primary purpose of the flexor pollicis longus. Because it is the only muscle that can bend the thumb’s interphalangeal joint, the flexor pollicis longus is essential for tasks requiring hand gripping.
A branch of the ulnar artery, the anterior interosseous artery supplies blood to the flexor pollicis longus.
Muscle anatomic variations are widespread and can involve slips of connective tissue originating from the flexor digitorum profundus, flexor digitorum superficialis, or pronator teres. The flexor pollicis longus is used in hand-gripping tasks, like picking up or moving objects.
The anterior interosseous nerve (7th and 8th cervical nerve roots) innervates it through the median nerve.
The inability to oppose the tips of the thumb and index finger (as in making an OK sign) is an indication of weakness in the FPL and FDP muscles, but this weakness may only be seen in cases of acute compression.
To test the flexor pollicis longus, ask the patient to flex the tip of their thumb while keeping the other fingers extended. Resistance can be applied against the distal phalanx of the thumb.
References
Benson, D. C. (2023, July 24). Anatomy, Shoulder and Upper Limb, Hand Flexor Pollicis Longus Muscle. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK538490/


5 Comments