Amputation Of Upper Limb: Indication, Treatment, Prosthesis
Table of Contents
Definition Of Upper Limb Amputation:
- Upper limb amputation is the removal of any part of the upper limb by surgery, trauma, or pathology.
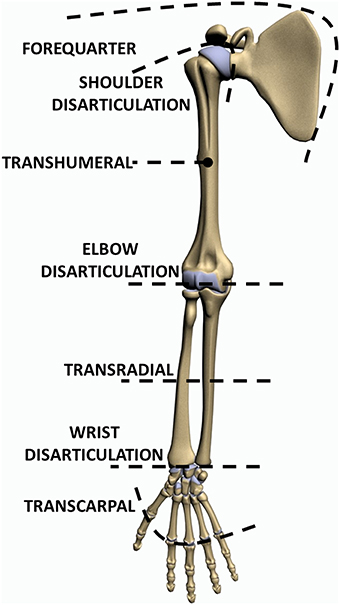
Level Of Upper Limb Amputation:
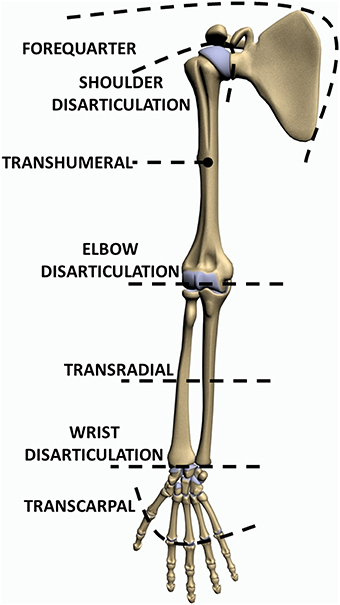
Forequarter Amputation:
- Forequarter Amputation, amputation is carried out proximal to the shoulder joint. It is indicated for malignant bone tumors of the upper end of the humerus. In this, part of the scapula and clavicle are removed along with the muscles of the shoulder girdle.

Disarticulation :
- Disarticulation is generally not so popular in the upper limb except at the shoulder. Even in disarticulation of the shoulder, the head of the humerus is preserved, wherever possible, to maintain the contour of the shoulder for cosmesis.

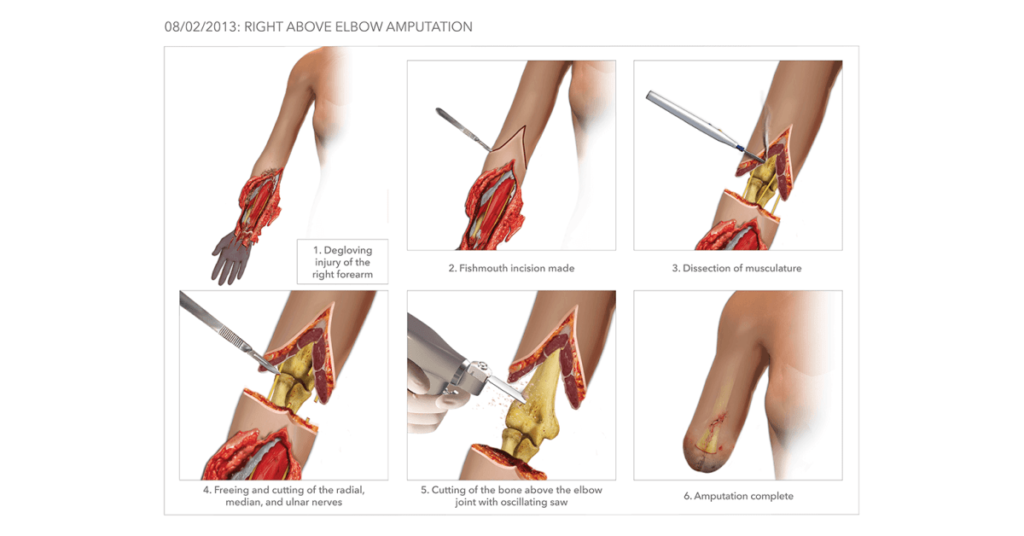
Above Elbow Amputation :
- An above amputation of the elbow is the removal of the arm above the elbow joint.
- A 20 cm long stump is measured from the tip of the acromion is ideal.
Below elbow amputation :
- A below-elbow amputation of the elbow is the removal of the arm below the elbow joint.
- The optimal length of a below-elbow stump is 20 cm as measured from the tip of the olecranon, with a minimum length of 7.5 cm.

Krukenberg amputation :
- Krukenberg amputation is performed in patients, usually with bilateral below elbow amputation, who have a sufficiently long below-elbow stump. In this operation, the forearm is split between the ulna and the radius to provide the pincer grip. The patient can hold the spoon or such lighter objects with this “fork”. For cosmetic purposes and for lifting heavy objects a below-elbow prosthesis or a “hook” prosthesis, respectively, can be put over this stump.

Amputation through the hand :
- Amputation through the hand is designed to preserve as much length as possible to contribute to overall function. The exception to this dictum is traumatic amputation through the proximal phalanx of a finger. Here the short stump is of no use and in fact, it hinders the function of the hand, as things keep falling through the gap.
Ray amputation :
- ray amputation is an amputation through the neck of the metacarpal.
- ray amputation through the neck of the metacarpal is also done in the index and little finders for cosmetic reasons.

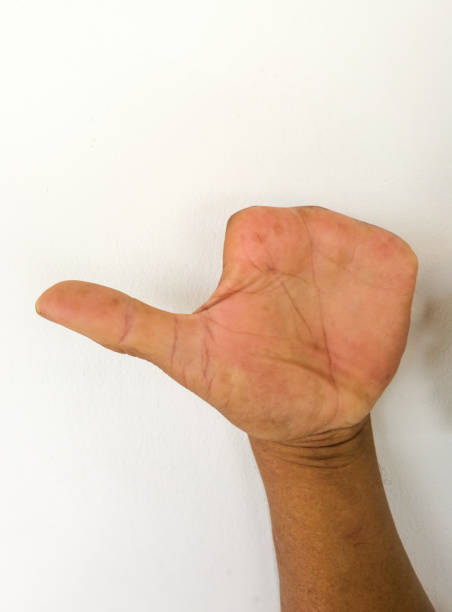
Thumb amputation :
- In thumb amputation, the maximum subsequent reconstructive procedures, such as metacarpal lengthening or composite bone grafts or toe transfer, are performed for a thumb with a short stump.

Indication Of Upper limb Amputation:
- Trauma
- Malignant tumors
- Nerve injuries and infections
- Extreme heat and cold
- Peripheral Vascular Insufficiency
- Congenital absence of limbs or malformations
- severe infections like gas gangrene, osteomyelitis
Multidisciplinary team :
- diabetologist
- podiatrist
- microbiologist
- nurse
- orthopedic surgeon
- vascular surgeon
- Physiotherapist
- occupational therapist
- Psychologist
What are the responsibilities of the team?
- Evaluate the patient
- Ensure medical stability of the patient
- Prepare the patient for life as an amputee
- Prescribe prosthesis (if appropriate)
- Fabricate prosthesis
- Evaluate fit of the prosthesis Educate the patient about the use of and care of the prosthesis
- Follow-Up care for the patient
Physiotherapy treatment for upper limb amputation :
- Psychological counselling to the patient
- Psychological support
- Providing information is important
- to reduce the patients and the family’s anxiety,
- obtain cooperation in the treatment program
- to help the person with an amputation to adjust for his new condition.
- Feeling of a complete change in reality due to
- ack of function
- alteration of limb sensation
- change in body image
- lack of understanding of medical treatments
- Psychological counseling to the patient
- Breathing exercise :
- to prevent accumulation of fluid
- to prevent chances of infections
- Postural advice during sitting, standing and walking
- Maintain proximal joint Range Of Motion
- maintain the strength of muscles proximal to joint: Strengthening exercise can be given manually, with the sandbag or thera band.
- Encourage early active movement of all proximal joints from 1st day after amputation
- The resisted exercise started as soon as pain allows
- Active ROM
- Cervical spine:
- Flexion
- Extention
- Right side rotation
- Left side rotation
- Right side flexion
- Left side flexion
- Glenohumaral joint :
- Flexion
- Extention
- Abduction
- Adduction
- Internal Rotation
- External Rotation
- Scapula:
- elevation
- depression
- protraction
- retraction
- Elbow :
- flexion
- Extention
- Forearm:
- Supination
- pronation
Principles of bandaging the stump:
- The pressure of the elastic bandage should be moderately firm and distributed evenly.
- Extra pressure is necessary at corners to obtain the proper shape(conical shape) of the stump. pressure should be decreased proximally.
- diagonal, oblique, or spiral turns should be used during bandaging.
Treatment for stump edema:
Electrical stimulation with limb elevation helps to reduced edema
Elastic Bandage
Intermittent variable air pressure machine existed
Resisted exercise of the stump and other joints of the upper limb.
stump bandaging and conditioning:
stump conditioning :
- An ideal stump is well healed, firm, conical, and with slight flabby tissue.
- Bandaging: During bandaging, pressure and application of bandage should be proper.
- Exercise: Isometric exercise of muscles of the stump.
Prosthesis for upper-limb amputation:
There are six types of prosthetic designs available for upper limb amputation depending upon the level of amputation :
- Forequarter Amputation
- Shoulder Disarticulation
- Above Elbow Amputation
- Belove Elbow Amputation
- Wrist disarticulation
- Mechanical terminal devices
Prosthesis for Forequarter Amputation :
The whole arm is removed along with the scapula and clavicle. A plastazote cap, padded with foam and retaining straps, can be provided. Only a sleeve fitter cosmetic prosthesis may be supplied.

Prosthesis for Shoulder disarticulation :
It incorporates an extended shoulder cap to hold the prosthesis in shoulder disarticulation. The elbow joint of the prosthesis can be flexed by strong protraction of the shoulder which puts tension on the flexion cord. Handpieces can be purely split hook types or cosmetic.

Prosthesis for Above elbow amputation :
The prosthesis is the same as shoulder disarticulation. In this, flexion of the elbow joint, achieved by the combined action of scapular protraction and arm flexion, is comparatively stronger. Automatic functional locking can be attained by the reverse movement of combined depression and extension of the arm.

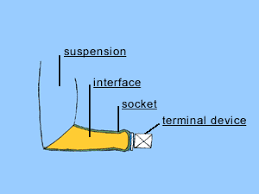
Prosthesis for Below elbow amputation :
(a)A cup socket, harnessing with an operational cord, can be given to activate the terminal device. (b)The terminal device is operated by a loop harness attached to a self suspending supracondylar socket.
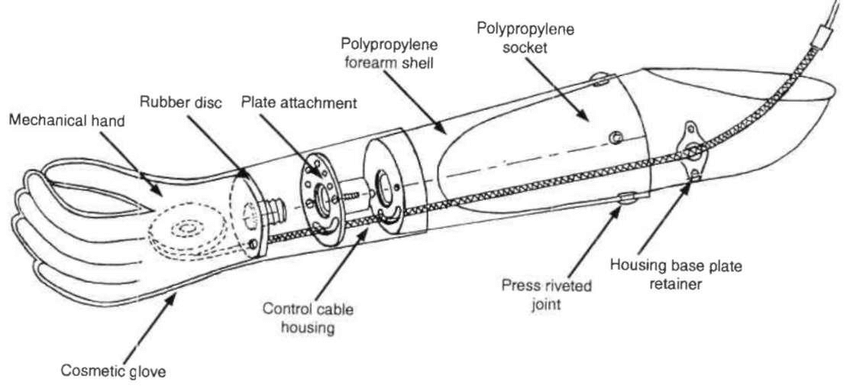
Prosthesis for Wrist Disarticulation :
For wrist disarticulation or below elbow stump, a split socket forearm with a wrist rotation unit can be given. A locking device can be provided for pronation and supination.
Terminal device :
- 1)Mechanical thumb abduction for grasp can be attained by tension on the operation cord.
- 2)Mechanical hand allowing grippy flexion of the index and middle finger with the thumb are available.
- 3)Split hook: A popular terminal device with one fixed and the other movable jaw operated by the power of the shoulder girdle muscles is used as a working strong hand.
- 4) Battery-operated myoelectric devices for specific tasks are also available or can be fabricated.

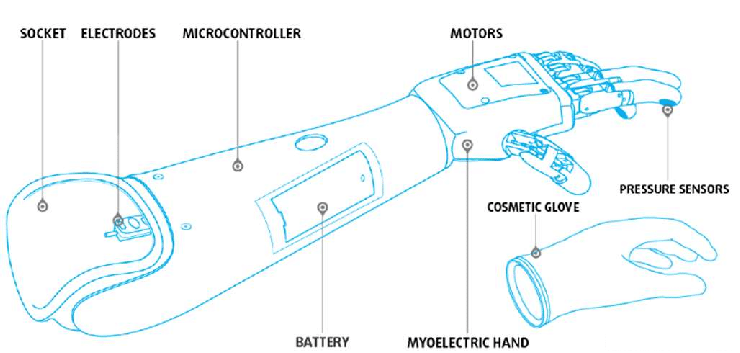
Myoelectric Prosthesis:
- Effective hand function has been reported by a myoelectrical controlled prosthesis in adults as well as in children.
- The prosthesis has a self-suspending socket with pick-up electrodes placed over the flexion and extension respectively.
- These electrodes pick up the myopotentials generated by the contractions in the respective muscle groups. The electrical potentials are amplified by microcircuitry.
- The motion power is obtained from compact 6-volt batteries.
- The thought and the voluntary effort producing flexion contractions will switch on flexion or grasping motion of pinch grip at the hand.
- Reversing the process to the extensor group initiates extension of the hand or the release of grasp. The main advantage is the combination of function and cosmesis.
A complication of upper limb amputation :
Phantom limb pain: A feeling of pain or sensations in the “missing limb” may occur Phantom limb; is likely to be neuropathic pain. treatment is generally with neuropathic pain is medication such as gabapentin and pregabalin.
Residual limb pain: This is likely to be musculoskeletal and localized in nature due to the remodeling of scar tissues, muscles, and fascias. Treatment includes care of the wound and systemic medications such as NSAIDs, acetaminophen, opioids, and in some cases muscle relaxants. techniques like desensitization may also be used such as compression, tapping, massage, and other modalities.
Edema: Localized swelling is a complication that is very common to occur in amputations and has the best outcome when control is started soon after surgery, with an immediate postoperative rigid dressing (IPROD). In the weeks following amputation, edema can further be controlled by compressive bandaging, massage, elevation, and in patients who have co-morbidities affecting fluid balance, use of diuretics.
Contracture formation: Contractures are a musculoskeletal condition causing rigidity or hardening of muscles, tendons, or other tissues which leads to deformity and rigidity of joints; this complication is long-term that arises through mechanisms that are not completely clear. It is thought that reduced neural activation, protracted placement of a joint with the muscle in the short position, and muscle atrophy are all contributing risk factors for formation. the management of this complication involves stretching maneuvers to preserve the range of motion and strengthening to preserve muscle strength.
Body Asymmetry: An amputation causes changes in weight distribution and can modify the center of gravity (COG) leading to compensatory mechanisms in function and gait, which can lead to pain, muscles spasms, or discomfort in other areas of the body.
Skin Breakdown: skin breakdown at the site of surgery can occur for a variety of reasons including poor wound healing due to co-morbidities, excessive bleeding, infection, edema, and poor dressing techniques. In the long term, this complication may occur due to assistive devices or prostheses that a patient may use. skin breakdown complications decrease with the help of shaping the residual limb into a proper cylindrical or conical shape with smooth edges so that it is useful during prosthetics.
Cosmetic acceptability: Cosmetic acceptability patients have emotional and mental side effects after amputation. Using an artistically appealing surgical technique, fitting the patient with a skin tone matched prosthesis, and minimal bracing may help with this concern.
Deep vein thrombosis (DVT)
we can prevent deep vein thrombosis (DVT) by the mobility of limbs. To prevent deep vein thrombosis in the lower limb we can give ankle-toe movement.
Excess bleeding
Blood clots
Poor healing
wound infection
pneumonia
Stump ulceration
Flap necrosis
Joint stiffness
Osteomyelitis
Osteoporosis