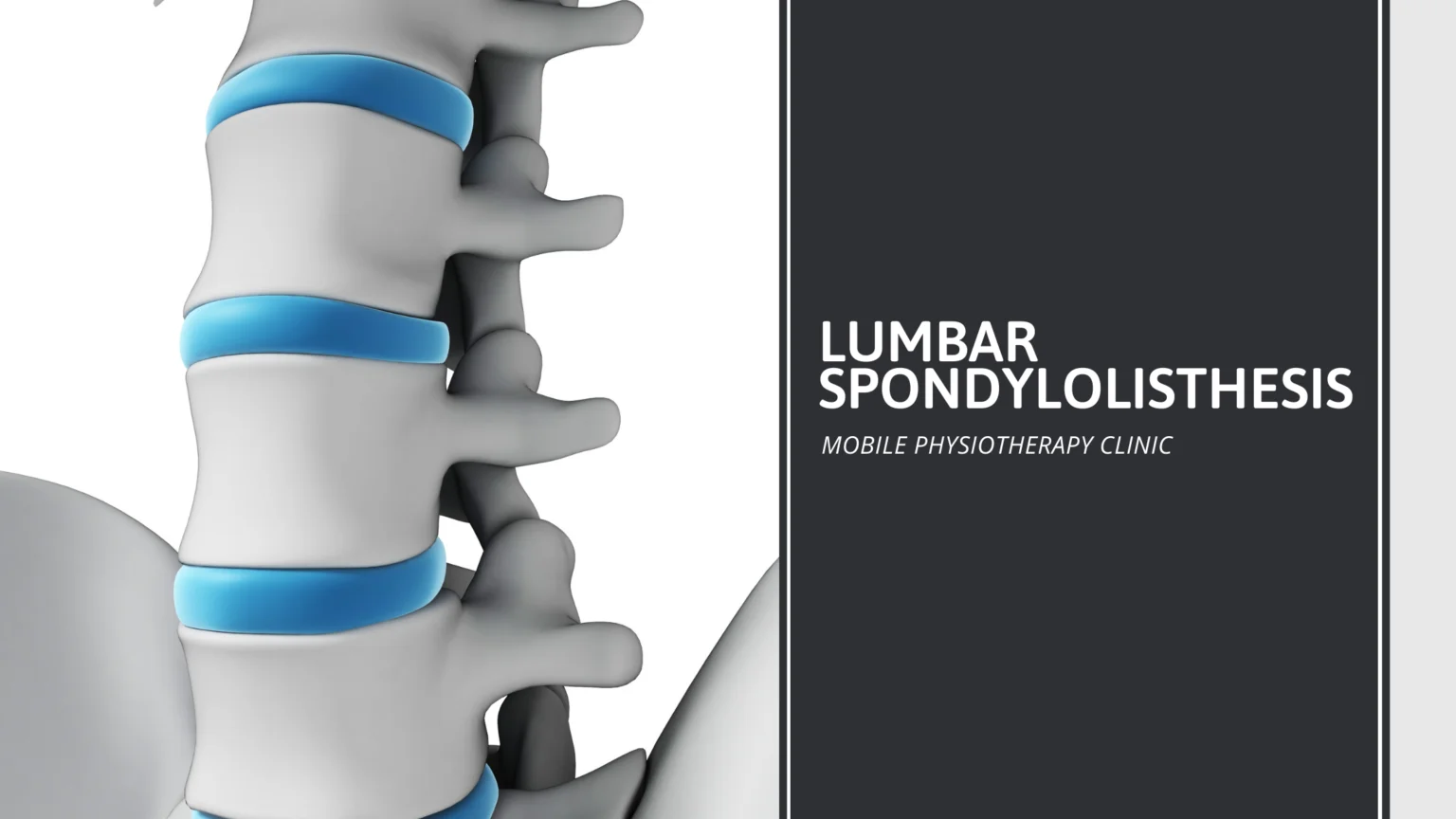
Lumbar Spondylolisthesis
Table of Contents
What is a Lumbar Spondylolisthesis?
Lumbar Spondylolisthesis is a condition involving spine instability, which means the vertebrae move more than they should. A vertebra slips out of place onto the vertebra below. It may put pressure on a nerve, which could cause lower back pain or leg pain.
The word spondylolisthesis (pronounced spohn-di-low-less-THEE-sis) comes from the Greek words spondylos, which means “spine” or “vertebra,” and listhesis, which means “slipping, sliding or movement.”
Is Spondylolisthesis and Spondylolysis same?
Both spondylolysis and spondylolisthesis cause low back pain. They are related but not the same.
- Spondylolysis: This spine defect is a stress fracture or crack in spine bones. It’s common in young athletes.
- Spondylolisthesis: This condition is when a vertebra slips out of place, resting on the bone below it. Spondylolysis may cause spondylolisthesis when a stress fracture causes the slipping. Or the vertebra may slip out of place due to a degenerative condition. The disks between vertebrae and the facet joints (the two back parts of each vertebrae that link the vertebrae together) can wear down. Bone of the facet joints actually grows back and overgrows, causing an uneven and unstable surface area, which makes the vertebrae less able to stay in place. No matter what the cause, when the vertebra slips out of place, it puts pressure on the bone below it. Most cases of spondylolisthesis do not cause symptoms. If you feel leg pain, it can also be caused by compression or a “pinching” of the nerve roots that exit the spinal canal (the tunnel created by the interlocking vertebrae of the spine). The compression or pinching is due to the vertebrae slipping out of position and narrowing the needed space for the nerves.
Symptoms of Lumbar Spondylolisthesis
A person may have had spondylolisthesis since birth and never experienced any symptoms from it, however it is common for a person to develop symptoms as they age.
Symptoms can range in severity from non-existent to a loss of urination and bowel movement control in more severe cases.
Some of the most common symptoms include:
- difficulty walking or running
- pain in the lower back or buttocks
- pain that travels from the back down one or both legs
- weakness in one or both legs
- pain in lower back and legs that is aggravated by movement or twisting
- tight hamstrings
- increased inward curve of the spine, known as lordosis
Causes of Lumbar Spondylolisthesis
There are six main types of Lumbar Spondylolisthesis. The type you have is determined by the cause. The types include:
- Congenital spondylolisthesis: A vertebra is defective from the time a person is born
- Isthmic spondylolisthesis: This is caused by another condition called spondylolysis. In spondylolysis, a fracture, or crack, in the thin part of a vertebra can result in vertebrae slipping backward, forward, or over a bone below
- Degenerative spondylolisthesis: Over time, the disks that cushion vertebrae dry out and get thinner. This thinning makes it easier for a vertebra to slip out of place
- Traumatic spondylolisthesis: An injury or trauma causes a vertebra to slip out of place
- Pathological spondylolisthesis: Another condition such as osteoporosis or cancer causes it
- Post-surgical spondylolisthesis: A vertebra slips out of place after spinal surgery.
Spondylolisthesis is more likely if:
- You are an athlete. It’s especially common in kids who do gymnastics or play football.
- You were born with thinner areas of vertebrae that are prone to breaking and slipping
- You are old
- You have a degenerative spinal condition
Risk Factors of Lumbar Spondylolisthesis
Risk factors for Lumbar Spondylolisthesis include a family history of back problems. People who are born with a defect in the pars interarticularis bone in the spine (a condition called spondylolysis) are at increased risk of isthmic spondylolisthesis. Other risk factors include a history of repetitive trauma or hyperextension of the lower back or lumbar spine. Athletes such as gymnasts, weight lifters, and football linemen who have large forces applied to the spine during extension are at greater risk for developing isthmic spondylolisthesis.
Preventions of Lumbar Spondylolisthesis
There are many things you can do to help prevent spondylolisthesis and to improve the health of your spine. By following the tips listed below, you can enjoy the benefits of a healthy spine at any age.
- Follow your doctor’s treatment plan and continue your home exercise plan (if you were in physical therapy)
- Sit and stand properly
- Learn to lift correctly
- Exercise regularly (Aerobic exercise is especially good)
- Don’t add stress to your low back. Avoid lifting heavy items, doing strenuous sports, and excessive bending and twisting
- Attain and maintain a healthy body weight
- Eat healthy (a well-balanced, low-fat diet rich in fruits and vegetables)
- Stop smoking
- Avoid excessive use of alcohol
- Get plenty of rest
Diagnosis
In many cases, a person may not know they have spondylolisthesis as they may have no symptoms. In these cases, a doctor might discover the condition during an exam for something else entirely.
Diagnosis starts with a physical exam and questions about what kind of pain or numbness the person is experiencing. If a doctor suspects spondylolisthesis, they will order an X-ray of the back.
Visual examination of the X-ray is often enough to determine if a person has spondylolisthesis, as well as to decide the grade.
In some cases, a doctor may order additional imaging to find the exact locations of the fractures to help guide the individual’s treatment.
The cause of spondylolisthesis can often be found by the initial questions about when and how the symptoms started.
Types and Grades of Lumbar Spondylolisthesis
Due to the varying degrees and causes of the misalignment, spondylolisthesis is broken down into types and grades. The six main types are based on the cause of the spondylolisthesis.
Type I – In some cases, people are born with spondylolisthesis. A child may also develop the condition naturally during his or her developmental years. In both cases of Type I spondylolisthesis, a child may not experience any symptoms or problems until later in life.
Types II – In Type II, the most common type, there is a problem with a section of the vertebra called the pars interarticularis. Type II is further broken down into the following subtypes:
- Type IIA involves many microfractures caused from overuse and hyperextension
- Type IIB involves many microfractures that do not fracture completely and heal with extra bone in place. The extra bone causes stretching and misalignment
- Type IIC is a complete fracture that has been caused by trauma. A sports injury or being in a car accident may cause Type IIC
The fractures from Type II only become spondylolisthesis if they cause the vertebrae to slip forward.
Type III – Type III is associated with aging and the natural wear and tear on a person’s body.
Type IV – Type IV is a fracture that occurs anywhere in a vertebra except in the pars interarticularis region.
Type V – Type V involves tumors on the vertebrae that push on the bones and cause weakness.
Type VI – Type VI is an uncommon spondylolisthesis caused by weakening of the back due to surgery.
Lumbar Spondylolisthesis is further classified into grades, according to how far out of place the vertebra is. The grades are:
- Grade 1: 25 percent of the vertebral body has slipped forward. This is the lowest grade
- Grade 2: Between 25-50 percent of the vertebral body has slipped forward
- Grade 3: Between 50-75 percent of the vertebral body has slipped forward
- Grade 4: Between 75-100 percent of the vertebral body has slipped forward
- Grade 5: The vertebral body has completely fallen off and looks detached
Treatment of Lumbar Spondylolisthesis
Treatment depends on the grade of the slippage, your symptoms, age and overall health. Your doctor will discuss treatment options with you. You may need medication, physical therapy or surgery.
Nonsurgical treatments include:
- Rest: Take a break from strenuous activities and sports
- Medication: An over-the-counter nonsteroidal anti-inflammatory drug (NSAID), such as ibuprofen (Motrin) or naproxen (Aleve), can bring relief. If those don’t work, your healthcare provider may prescribe other medications
- Injections: You receive an injection of steroid medications directly into the affected area
- Physical therapy: A physical therapist can teach you targeted exercises to strengthen your abdomen (belly) and back. Daily exercises often relieve pain after a few weeks
- Bracing: A brace can help stabilize your spine. The brace limits movement so that fractures can heal. Braces are not used in adults
You may need surgery if you have high-grade spondylolisthesis, the pain is severe or you’ve tried nonsurgical treatments without success. The goals of spondylolisthesis surgery are to:
- Relieve pain from the irritated nerve
- Stabilize the spine where the vertebra has slipped
- Restore your function
Surgery for back pain due to spondylolisthesis typically involves spinal decompression, with or without fusion. Decompression alone is almost never done in isthmic spondylolisthesis. Studies show fusion with decompression may give better outcome than decompression alone. During a decompression surgery, your surgeon removes bone and disk from the spine. This procedure gives the nerves space inside the spinal canal, relieving pain.
For a fusion surgery, your surgeon fuses (connects) the two affected vertebrae. As they heal, they form into one bone, eliminating movement between the two vertebrae. You may experience some limited spinal flexibility as a result of the surgery.
How to brace a Lumbar Spondylolisthesis?
Children or adults with spondylolisthesis can wear braces or corsets as part of a non-surgical (or conservative care) treatment plan. Bracing is usually recommended for patients with a pars interarticularis fracture that is likely to heal—if given the right support.
A lumbar brace or corset will compress your abdomen, and that will take some of the pressure off your spinal column. The goal is to give you some pain relief while keeping your spine safe as the pars interarticularis fracture tries to heal.
Corsets
Corsets are made of a soft fabric, and they usually have sturdy supports—stays—in them. Like corsets that women used to wear, medical corsets also lace up, either from the front, back, or side. Most likely, you’ll have to wear your corset during the day, but you’ll be able to take it off at night. Your doctor, though, will give specific instructions on how and when to wear it.
Braces are made of plastic, so they’re more rigid than corsets. There are many types of braces available today, such as the Boston brace, and your doctor will figure out which brace is best for you.
Braces
You may even need to have a brace custom made, especially if you have very severe spondylolisthesis (the vertebra has slipped forward quite far over the one below it). Custom-made braces are made by an orthotist, and your doctor will recommend one for you. You’ll need to see him or her for the fitting.
Wearing a Corset or Brace
For the corset or brace to be effective, you have to adhere to all of your doctor’s instructions. When you first get the corset or brace, he or she will tell you when to wear it, how to wear it, and what to avoid doing while wearing it. The doctor (or other medical professional—perhaps a nurse) will even explain what to do to avoid skin irritation. A general hint is to wear a light cotton T-shirt under the brace to protect your skin.
You may be concerned that wearing a brace will cause your back muscles to weaken too much. Don’t worry about that—most doctors don’t believe that to be the case. If you follow the doctor’s directions about when to wear the brace (and don’t wear it more than you are told to), then your body shouldn’t become overly dependent on it.
Bracing after Surgery
If you have to have surgery to fix or stabilize your spondylolisthesis, you may need to wear a brace after the surgery. This will help support your spine and muscles while you heal.
Exercises for Lumbar Spondylolisthesis
After a thorough evaluation, your physical therapist will be able to provide you with a personalized home exercise program to help decrease pain due to spondylolisthesis.
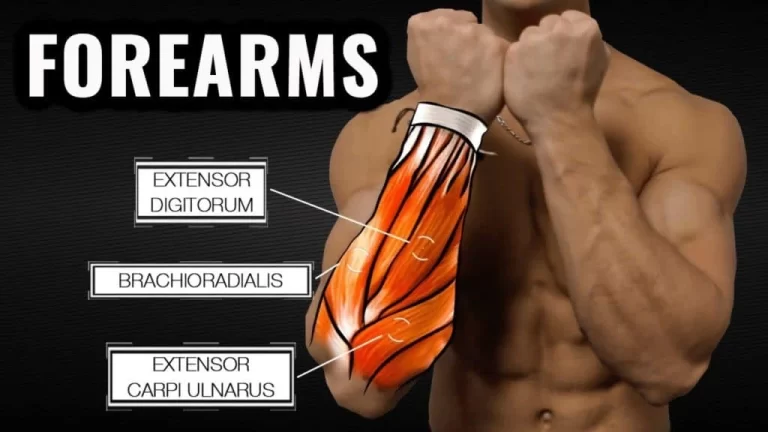
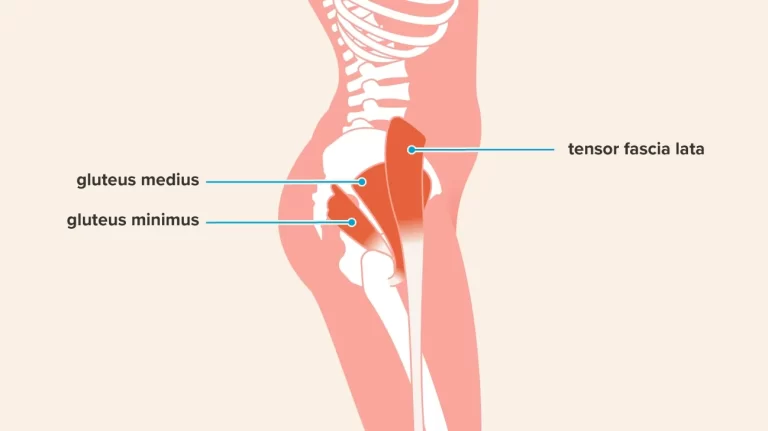
This program often includes lumbar flexion exercises also called Williams flexion exercises, core stabilization exercises, and exercises or stretches for the muscles of the back, hamstrings, and hips. Low-impact exercise such as cycling or swimming is also recommended to promote healing and decrease pain.
Pelvic tilt
Pelvic tilt exercises help decrease pain by stabilizing the lower spine in a flexed position. Pelvic tilts are done in different positions depending on pain and the patient’s preference.
- Lie face up with your knees bent and feet flat on the ground.
- Start by flattening your lower back against the ground, engage your abdominal muscles to hold the position.
- Hold for 15 seconds before relaxing.
- Repeat 10 times.
Crunches
Weak abdominal muscles often contribute to instability and cause pain in those with spondylolisthesis. You can strengthen your abdominal muscles with a crunch exercise.
Move slowly and focus on proper form by engaging your core muscles before starting any movement. Even small movements make a big difference.
Don’t force your body to move through full range of motion for these exercises, as it may increase pain and slow your recovery.
- Start by lying on the ground with your knees bent, feet flat on the ground and arms folded over the chest. If necessary, you can support your head with your fingers behind your ears, but don’t pull on your head as you go through this movement.
- Slowly lift your head and shoulders off the floor until a contraction in the abdominals is felt.
- Hold for three seconds, and then lower to starting position.
- Repeat 10 times.
Double knee to chest
Working the deep core muscles of the torso will help decrease instability and improve pain associated with spondylolisthesis.
- Start by lying face up with your knees bent and feet flat on the floor.
- Engage your stomach muscles by drawing the belly button to the floor.
- With the assistance of the hands, pull both knees up to the chest and hold for five seconds.
- Relax and repeat 10 times.
Multifidus activation
The multifidus muscles are small but important muscles that lie next to your spine. They help with twisting and bending movements, and they increase stability of the spinal joints. These muscles are often weak in people with spondylolisthesis.
You can find and activate your multifidus by lying on your side and reaching your top hand around to feel the vertebrae of your lower back. Slowly move your fingers to the side until they slip into the groove beside your spine.
- Activate your core muscles by imagining you are pulling your thigh to your chest, but do not actually move your leg.
- This contraction should cause the multifidus muscle to bulge under your fingers.
- Hold this for three seconds, and repeat 10 times on each side.
Hamstring stretch
For those with spondylolisthesis, spinal instability often causes tension in the hamstrings, the large muscles that run down the back of the thighs. Tight hamstrings can pull on the lower back, increasing pain or discomfort.
- Sit on the ground with your legs stretched directly in front of you, toes pointed toward the ceiling.
- Slowly lean forward and reach for your toes. Don’t worry if you can’t touch your feet — just reach until you feel a stretch down the back of your legs.
- Hold for 30 seconds and repeat three times, trying to get a little further each time.




3 Comments