Spinal Cord Injury
Table of Contents
What is Spinal Cord Injury?
A spinal cord injury damages the spinal cord itself or nearby bones and tissues. Depending on the severity of the condition, it frequently causes permanent changes in sensation, strength, and other body mobility or function in various parts of the patient’s body below the site of the injury.
Treatments include medication, surgery, and physiotherapy. Symptoms of spinal cord injury depend on its location on the spinal cord and the severity of the injury. Symptoms may include complete or partial loss of sensory function or motor control of legs, arms, and/or body.
The most severe spinal cord injury affects the systems that regulate bladder or bowel control, heart rate, breathing, and blood pressure. Most patients with spinal cord injury have chronic pain.
If a patient has recently injured his or her spinal cord, it might seem like every aspect of his life has been affected. A patient might feel the effects of their injury emotionally, mentally, and socially.
The spinal cord sends messages between the brain and the whole body. Layers of tissue known as meninges and a column of vertebrae mean spinal bones are present and surround the spinal cord and protect the spinal cord. Mostly seen spinal cord injuries come from a traumatic, sudden blow to the vertebrae. The fractured or broken bones damage the spinal cord and its nerves surrounding it. In a few rare cases, an injury can completely sever or split the spinal cord.
The most seen spinal cord injuries are because of preventable causes such as falls, road traffic crashes, or violence.
Patients with a spinal cord injury are 2 to 5 times more likely to die before than individuals without a spinal cord injury, with worse survival rates in middle and low-income countries.
Spinal cord injury is associated with lower rates of economic participation and school enrollment, and it carries substantial personal and societal costs.
The spinal cord does not have to be highly injured for a loss of function to happen. In fact, in most patients with spinal cord injury, the cord is intact or safe, but the damage or injury to it results in loss of function. Spinal cord injury is very unique from back injuries such as spinal stenosis, ruptured disks, or pinched nerves.
Key facts of Spinal cord injury
- Around the world, between 2.5 lakhs and 5 lakhs patients suffer a spinal cord injury (SCI) every year. There is no reliable estimation of global prevalence, however, the estimated yearly global incidence is 40 to 80 cases per million population. Though the proportion of non-traumatic spinal cord injury appears to be growing, up to 90% of these spinal cord injury cases are because of traumatic causes.
- Spinal cord injury (SCI) is a debilitating neurological condition with a lot of socio-economic impact on the affected person and the whole health care system. In the recent era, the estimated lifetime cost of spinal cord injury (SCI) patients is $2.35 million per head. The Male to female ratio of 2:1 for SCI happens more generally in adults in comparison to children. Demographically, men are mostly affected during their late and early adulthood approximately the 3rd and 8th decades of life whereas women are at higher risk during their adolescence around 15–19 years and the 7th decade of their lives i.e. age distribution is bimodal, with the first peak including young adults and a second peak including adults over the age of 60. Those over 60 years of age who suffer spinal cord injury (SCI} have considerably worse outcomes than younger patients their injuries usually result from age-related bony changes and falls.
What are the symptoms of spinal cord injury?
Symptoms of spinal cord injury (SCI) can vary widely. The location of the injury on the spinal cord identifies how severe the symptoms are and what part of the body is affected.
- Immediately after a spinal cord injury, a patient’s spine may be in shock. This causes a decrease or loss in feeling, reflexes, and muscle movement, however, as swelling heals, other symptoms may be seen depending on the location of the injury in the spinal cord.
- Any person who is with an individual who may have sustained a back injury should avoid trying to move or lift them, as this could mainly worsen any damage or injury.
Usually, the more severe the symptoms, the higher the level of the injury is to the spinal cord. For instance, an injury to the neck or cervical spine, the first and second vertebrae in the spinal column (C1, C2), or the mid-cervical vertebrae (C3, C4, and C5) affects the ability to breathe and the respiratory muscles. A lower injury, which is in the lumbar vertebrae, may affect muscle and nerve control of the bowel, bladder, and legs, and sexual function.
The lowest part of a patient’s spinal cord that remains undamaged or uninjured after an injury is referred to as the neurological level of a patient’s injury. The severity of the injury is frequently known as “the completeness“.
Moreover, paralysis from a spinal cord injury can be referred to as:
- Tetraplegia. It is also known as quadriplegia, this means that a patient’s hands, arms, trunk, legs, and pelvic organs are all affected by his or her spinal cord injury.
- Paraplegia. This paralysis affects the legs, all or part of the trunk, and pelvic organs.
- A doctor will perform a series of tests to identify and diagnose the completeness and neurological level of a patient’s injury.
Spinal cord injuries can cause one or more of the below-given signs and symptoms:
- Muscle weakness
- Loss of voluntary muscle movement in the arms, chest, or legs
- Loss of or altered sensation, including the ability to feel cold, heat, and touch
- Loss of bladder or bowel control
- Exaggerated spasms or reflex activities
- Changes in sexual sensitivity, sexual function, and fertility
- An intense stinging sensation or pain caused by damage to the nerve fibers in a patient’s spinal cord
- Difficulty coughing, breathing, or clearing secretions from a patient’s lungs
Emergency signs and symptoms
Emergency signs and symptoms of a spinal cord injury after an accident are below given:
- Pressure or extreme back pain in a patient’s head, neck, or back
- In-coordination, weakness, or paralysis in any part of a patient’s body
- Tingling, numbness, or loss of sensation in a patient’s fingers, hands, feet, or toes
- Loss of bladder or bowel control
- Difficulty with balance and coordination, along with an inability to walk
- Trouble breathing after injury
- A twisted or odd positioned back or neck
Having these above-given symptoms does not necessarily mean that an individual has a spinal cord injury. Sometimes, a broken backbone or vertebra can put pressure on the spinal cord, causing symptoms that may go away after the bone heals.
Spinal Cord Injury Classification and Syndromes
- Grading the severity and classifying the type of a traumatic or non-traumatic spinal cord injury is a universal language spine specialists tell that can improve the communication of patients.
- Spine specialists or surgeons who treat and diagnose traumatic spinal cord injuries (SCI) use a classification system to evaluate and grade a patient’s injury in terms of severity and damage. The grading of an injury improves communication for various medical specialties. Moreover, classifying the severity and type of spinal cord injuries (SCI) can help patients better understand neurological injury, the extent of their function, and the potential for improvement.
- Doctors all over the world classify spinal cord injuries (SCI) by use of a method developed by the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI). If a doctor suspects a spinal cord injury (SCI), he or she may conduct the ISNCSCI exam shortly after an individual arrives in the hospital.
The ISNCSCI is based on 3 scores:
- American Spinal Injury Association (ASIA) motor score, which grades muscle movement and strength.
- The ASIA sensory score, grades pinprick feeling and light touch.
- The ASIA Impairment Scale grade determines whether the injury is incomplete or complete.
American Spinal Injury Association (ASIA) impairment scale
The American Spinal Injury Association (ASIA) impairment scale or AIS describes a patient’s functional impairment as
a result of spinal cord injuries (SCI). Grades range from A to E, in that A indicates the most severe injury and E indicates the least severe. This scale shows how much sensation a patient feels after a pinprick and light touch at multiple points on the body and tests key motions or movements on both sides of the body.
Grade A = Complete
No sensory or motor function is preserved in the sacral segments S4-5.
Grade B = Sensory Incomplete
Sensory but not motor function is preserved below the neurological level and includes the sacral segments S4-5, and no motor function is preserved more than three levels below the motor level on either side of the body.
Grade C = Motor Incomplete
Motor function is preserved at the most caudal sacral segments for voluntary anal contraction OR the patient meets the criteria for sensory incomplete status (sensory function preserved at the most caudal sacral segments (S4-S5) by light touch, pinprick, or deep anal pressure, and has some sparing of motor function more than three levels below the ipsilateral motor level on either side of the body. For AIS C – less than half of key muscle functions below the single neurological level of injury have a muscle grade ≥ 3.
Grade D = Motor Incomplete
Motor incomplete status as defined above, with at least half (half or more) of key muscle functions below the single neurological level of injury having a muscle grade ≥ 3.
Grade E = Normal
If sensation and motor function as tested with the ISNCSCI are graded as normal in all segments, and the patient had prior deficits, then the AIS grade is E. Someone without an initial spinal cord injury (SCI) does not receive an AIS grade.
Complete and Incomplete Spinal Cord Injuries
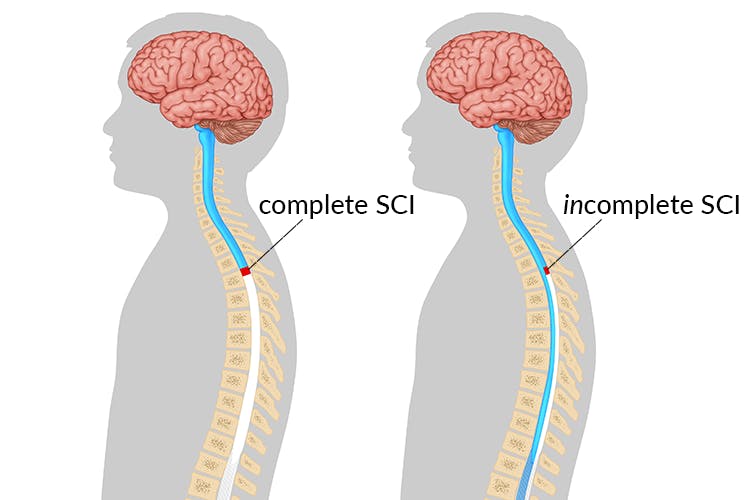
The ASIA Impairment Scale determines the category of spinal cord injury (SCI), which generally is complete or incomplete. A third, less common category, incomplete—refers to complete injuries that show some signs and symptoms of brain-muscle connectivity.
Complete Spinal Cord Injuries
- Complete spinal cord injuries (SCIs) are the most serious and occur when the spinal cord is damaged or injured, disturbing the brain’s ability to send signals below the injury site. Complete SCI occurs when there is a total loss of feeling (sensory function) and function (motor function) below the injury level. For an injury level, a thoracic injury may start at the arms and torso level, but it will also affect the pelvis, low back, tailbone, groin, legs, and toes. Complete spinal cord injuries (SCI) affect both sides of the body equally.
- Knowing the location of a patient’s injury and whether or not the injury is complete can help them begin researching their prognosis and asking a doctor intelligent questions about a patient’s spinal cord injury (SCI) rehabilitation. A doctor gives different labels to spinal cord injuries depending upon the nature of those injuries. The most commonly seen types of spinal cord injuries include:
Tetraplegia
These injuries are the result of damage or injury to the cervical spinal cord, typically the most severe, which produces varying degrees of paralysis of all four limbs. it is also known as quadriplegia. It eliminates a patient’s ability to move below the site of the injury and may produce difficulties with respiration, bowel and bladder control, and other routine functions. The more severe symptoms will be there if the higher up on the cervical spinal cord the injury is.
Paraplegia
This occurs when movement and sensation are removed from the lower half of the patient’s body, including the legs. These injuries are the result of damage or injury to the thoracic spinal cord, which can lead to paralysis below the waist while preserving a patient’s motor functions in his or her upper body and arms.
Triplegia
Triplegia causes a loss of movement and sensation in one arm and both legs, which is typically the result of an incomplete spinal cord injury.
Incomplete Spinal Cord Injuries
- Incomplete Spinal Cord Injuries (SCIs) commonly result from damage or compression being inflicted on the spinal cord that reduces the brain’s ability to send signals below the level of the injury site. Due to the partially compromised condition of the spinal cord, incomplete injuries vary drastically from patient to patient. Some motor and sensory functions may be slightly compromised in a few or nearly eliminated in others. Moreover, few incomplete injuries result in triplegia or the loss of movement and sensation in one arm and both legs.
- Incomplete spinal cord injuries are raising common, thanks in part to better treatment and increased knowledge about how to respond and how not to respond because of improved spinal cord injury research. These injuries now occur in more than 60% of spinal cord injuries, which means researchers are making real progress toward better treatment for spinal cord injury (SCI) rehabilitation. With incomplete spinal cord injury (SCI), some feelings and functions remain below the injury level. Usually, one side of the body has more function or feeling than the other side in patients. There are various types or syndromes of incomplete spinal cord injury (SCI), including central cord syndrome, Brown-Séquard syndrome, anterior cord syndrome, and posterior cord syndrome.
Spinal Cord Injury Syndromes
Central cord syndrome
Central cord syndrome is the most seen incomplete spinal cord injury (SCI) syndrome, which occurs in 15-25% of traumatic SCIs. Central cord syndrome is mostly seen in elderly patients with a history of spinal stenosis and cervical spondylosis who suffer spinal cord injury (SCI) from a traumatic fall. As the name identifies, this syndrome affects the central part of the spinal cord of patients. The central spinal cord contains large nerve fibers that exchange information between the cerebral cortex and the spinal cord. The cerebral cortex is essential to interpreting sensation (feeling),
personality, and motor function. The central spinal cord is also vital for arm and hand function, such as fine motor control eg. and writing, although the lower body may also be affected eg, loss of bowel and bladder control. Some survivors also suffer a loss of the ability to sexually function.
Brown-Séquard syndrome
Brown-Séquard syndrome is the result of damage or injury to one side of the spinal cord. This type of injury most often
occurs in patients who suffered a penetrating traumatic spinal cord injury (SCI), such as a knife or bullet wound. This syndrome affects either the right or left side of the spinal cord, while symptoms can affect both sides of the body, for example, movement may be not possible on the right side, but maybe fully retained on the left side. It is characterized by partial loss of function or impaired function, a vibrating sensation on the same side of the injury, and temperature and pain loss on the opposite side of the injury. The degree to of Brown-Sequard patients is injured greatly varies from individual to individual.
Anterior cord syndromes
The anterior spinal cord is the front part of the structure of the spinal cord. These syndromes are most common in patients with non-traumatic spinal cord injury (SCI) as opposed to traumatic spinal cord injury (SCI). Anterior cord syndrome causes a complete loss of movement, temperature, and pain loss, but it preserves light touch sensations.
Posterior Cord syndromes
The posterior spinal cord in the back and presents with preservation of motor function, pain, and temperature sensation but
with loss of light touch, vibration, and proprioception secondary to damage to the posterior column. This type of syndrome is very rare and a patient will display profound ataxia because of a loss of proprioception.
Cauda Equina Syndrome
An injury located below the level at which the spinal cord splits into the Cauda Equine around Levels L2 – S5, below
the Conus Medullaris, is most generally caused by compression. It is not a true spinal cord injury as it impacts the nerve roots rather than the spinal cord. It presents as a lower motor neuron lesion with flaccid paralysis secondary to
peripheral nerve damage at this level of the spine, generally affecting many levels with loss of spinal cord mediated reflexes and variable sacral root interruption. It can cause low back pain, paralysis or weakness in the lower limbs, loss of
sensation, bladder and bowel dysfunction, and loss of reflexes, and more generally occur on one side of the patient’s body.
This type of injury has a better prognosis for recovery of function if managed as early as possible because the peripheral nervous system has a greater capacity for healing faster than the central nervous system.
What causes spinal cord injury?
Spinal cord injuries can occur because of damage to the vertebrae, discs, or ligaments of the spinal column or to the spinal cord itself.
- A traumatic spinal cord injury can result from a traumatic, sudden blow to a patient’s spine that fractures, dislocates, compresses, or crushes one or more of a patient’s vertebrae. It can also occur because of a knife or gunshot wound that penetrates and cuts a patient’s spinal cord. More damage generally occurs over days or weeks because of bleeding, inflammation, swelling, and fluid accumulation in and around his or her spinal cord.
- A non-traumatic spinal cord injury can be occurred because of cancer, arthritis, inflammation, infections, or disk degeneration of the spine of an individual.
Damage to nerve fibers
Whether the reason for injury is non-traumatic or traumatic, the damage affects the nerve fibers passing from the injured area and can impair part of or all the nerves and muscles below the injury site.
A chest means thoracic level or lower back means lumbar level injury can affect a patient’s torso, legs, bladder and bowel control, and sexual function. A neck means cervical level injury affects the same areas along with affecting movements of a patient’s arms and sometimes his or her ability to breathe.
Common causes of spinal cord injuries
Motor vehicle accidents
Being stuck as a pedestrian, motorcycle, and auto accidents are the main leading cause of spinal cord injuries, which accounts for almost half of the new spinal cord injuries each year.
Falls
A spinal cord injury after age 65 is most frequently caused by falling from a significant height.
Acts of violence
About 12% of spinal cord injuries occur because of violent activities, generally from gunshot wounds or Knife wounds also are common.
Sports and recreation injuries
Athletic activities, such as impact or dangerous sports and diving into water that is too shallow and hitting the bottom, cause about 10% of spinal cord injuries.
Diseases
Arthritis, cancer, osteoporosis, and inflammation of the spinal cord also can cause spinal cord injuries. Along with this, spina bifida and polio also can cause spinal cord injury.
electrical accidents
Severe twisting of the middle portion of the back movement can cause spinal cord injury.
What are the risk factors for spinal cord injury?
Although a spinal cord injury is generally the result of an accident and can happen to any person, few factors can predispose a person to be at higher risk of having a spinal cord injury, which includes:
Being male
Spinal cord injuries affect a huge number of males. In fact, females have chances for only about 20% of traumatic spinal cord injuries in the United States.
Being between the ages of 16 and 30
More than 50% of spinal cord injuries occur in patients in this age group.
Being 65 and older
Another peak level in spinal cord injuries occurs at age 65 because Falls cause most injuries in older adults.
Alcohol use
Alcohol use is involved in approximately 25 % of traumatic spinal cord injuries.
Engaging in risky behavior
Playing sports or diving into too-shallow water without wearing the proper safety gear such as a helmet or taking proper precautions can lead to spinal cord injuries. Motor vehicle crashes or accidents are the main cause of spinal cord injuries for individuals under 65 age.
Having certain diseases
A comparatively minor injury can cause a spinal cord injury if a person has another disease that affects a person’s joints or bones, such as osteoporosis.
According to the National Spinal Cord Injury Statistical Center:
- 43 years is the average age at which spinal cord injury occurs.
- Men have approximately 78% of new spinal cord injury cases.
- Motor vehicle crashes are responsible for around 40% of spinal cord injuries, with falls following closely behind.
The American Association of Neurological Surgeons state:
- Motor vehicle accidents are the main cause of spinal cord injury in younger individuals.
- Falls are the main cause of spinal cord injury in individuals above the age of 65 years.
- As high as 90% of all sports-related spinal cord injuries occur in men.
What are the complications of spinal cord injury?
Spinal cord injury results not only in sensory and motor problems but also in autonomic dysfunctions because of the disruption between the spinal cord and higher brain centers. Autonomic dysfunction can include affected cardiovascular, respiratory, urinary, thermoregulatory, gastrointestinal, and sexual activities. Common secondary health conditions like spasms, pressure sores, chronic pain, and urinary tract infections frequently negatively affect social participation and quality of life.
Autonomic Dysfunction
In the acute phase of spinal cord injury, the main type of autonomic dysfunction present is a spinal and neurogenic shock.
Spinal Shock
It is a temporary loss of all neurological activity including sensory, motor, and reflex activity below the level of the spinal cord lesion, which can occur immediately after the onset of an acute spinal cord injury. Reflexes above the level of injury remain normal while below the level of injury is either absent (areflexia) or depressed (hyporeflexia). The gradual development of spasticity in patients with an upper motor lesion is proof of spinal shock resolution.
Neurogenic Shock
It also referred to as vasogenic shock, can occur after damage to the central nervous system, generally in patients with a lesion at T6 or above. Incidence of neurogenic shock was 3% in lumbar injuries, 7% in thoracic injuries, and 19.3% in cervical injuries. Consequences of neurogenic shock results in a hemodynamic triad of bradycardia, severe hypotension with systolic blood pressures of < 90 mmHg in a supine position, and peripheral vasodilation.
Thermoregulation
It is a process that allows the body to maintain its core internal temperature, with baseline temperature generally between 37°C (98°F) and 37.8°C (100°F). Patients with a spinal cord injury have impaired thermoregulation and are unable to respond properly to the changing temperatures of their surrounding environments, which leads to dysregulation in vasomotor tone, sweating dysfunction, and skeletal muscle shivering below the level of the spinal cord injury.
Sweat secretion
Excessive sweating(hyperhidrosis) is a common problem in patients with SCI. The most common symptoms are abolished/ minimal sweating below the level of injury and profuse sweating above the level of injury. This is because a compensatory increase in sweat secretion above the level of injury and due to the loss of sympathetic stimulation below the level of injury, which reduced sweat production.
Cardiovascular Dysfunction
In the acute phase, many problems of the cardiac rhythm may occur including sinus bradycardia and bradyarrhythmias (14%-77%) such as escape rhythm, orthostatic hypotension (33%-74%), supraventricular ectopic beats (19%), ventricular ectopic beats (18%-27%), increased vasodilatation, vasovagal reflex, and stasis, whereas in the chronic phase of injury common cardiovascular complications include autonomic dysreflexia, orthostatic hypotension, loss of reflex cardiac acceleration, impaired cardiovascular reflexes, reduced transmission of cardiac pain, cardiac atrophy with quadriplegia because of loss of left ventricular mass and pseudo-myocardial infarction.
Autonomic Dysreflexia
It also referred to as autonomic hyperreflexia, is an acute syndrome characterized by a sudden excessive raise in Systolic Blood Pressure triggered by ascending sensory noxious stimuli below the level of the lesion. Noxious stimuli can include urinary stasis, bladder infection, bowel obstruction, pressure sores, tight clothing, improper positioning, catheter blockage, twisted intercostal drainage tubes, sudden violent hip range of motion, and extremely hot weather with the most common causes resulting from bowel and bladder related problems.
Deep Vein Thrombosis
It refers to the formation of one or more blood clots in one of the body’s large veins. It tends to start in the calf muscle. The signs and symptoms include:
- Low-Grade Fever
- Localized swelling of the lower limb, generally unilateral
- Increased Leg Spasms
- Heat and Discolouration/Erythema of Skin
- Pain sometimes present in patients with intact sensation
- Autonomic Dysreflexia if Lesion Above T6
Pulmonary Embolism
It is the blockage of an artery in the lungs by a substance or clot that has moved from elsewhere in the body through the bloodstream. The signs and symptoms include:
- Shortness of Breath
- Hypoxia
- Sweating
- Haemoptysis
- Tachycardia
- Confusion
- Chest Pain
- Loss of Consciousness
Orthostatic Hypotension
It is also referred to as Postural Hypotension, which is defined as a reduction in systolic blood pressure of 20 mmHg or more, or a decrease in diastolic blood pressure of 10 mmHg or more, while the body position changes from supine to upright.
Symptoms include lightheadedness, dizziness, pallor, headache, yawning, sweating, muscle weakness, fatigue, and occasionally syncope which occurs especially if there has been an extended period of prior bedrest.
Respiratory Dysfunction
Partial paralysis or paralysis of key muscles has a marked impact on respiratory function. Respiratory complications include:
- Ventilation-perfusion (V/Q) mismatch due to adrenergic blockade and/or sympathectomy
- Atelectasis because of decreased vital capacity and functional residual capacity
- Decreased cough, which increases the risk of atelectasis, retained secretions, pneumonia, and respiratory infections
- Increased work of breathing because of decreased compliance
- Breathing Pattern Disorders e.g. Hypoventilation
- Muscle Paralysis
- Muscle Fatigue
Gastrointestinal Dysfunction
It includes diarrhea, constipation, straining, distention, abdominal pain, rectal bleeding, Urinary Incontinence, hemorrhoids, and autonomic dysreflexia during bowel movements occur in 27% to 62% of patients with a spinal cord injury.
Paralytic Ileus
It is an obstruction of the intestine after the paralysis of the intestinal muscles with no evidence of mechanical obstruction. The paralysis does not require to be complete to cause ileus, however, the intestinal muscles are so inactive that it prevents the passage of food, which leads to a functional blockage of the intestine and causes abdominal distension.
Neurogenic Bowel
Neurogenic bowel dysfunction with sphincter control changes to bowel motility, paired with hand dexterity, and impaired mobility is a major psychological and physical problem for many patients with spinal cord injury.
Upper Motor Neuron (UMN) Bowel Syndrome
It occurs in a spinal cord injury above the conus medullaris and results in a hyperreflexia bowel, seen by anal tones and increased colonic wall, with voluntary external anal sphincter control. Typically associated with fecal retention and constipation.
Lower Motor Neuron (LMN) Bowel Syndrome
It occurs in a spinal cord injury at the injury of level cauda equina or conus medullaris results in an areflexic bowel, characterized by slow stool propulsion with an atonic external anal sphincter and loss of spinal cord mediated peristalsis. Generally associated with constipation and a higher risk of incontinence because of flaccid paralysis of the external anal sphincter and reduction of levator ani motor control.
Urological Dysfunction
It occurs in up to 80% of patients with a spinal cord injury including urinary tract infection (UTI), urinary retention, upper and lower urinary tract deterioration, bladder or stones, neurogenic bladder, and incontinence.
Neurogenic Bladder
Neurogenic bladder dysfunction with changes to sphincter control, and micturition, coupled with impaired hand dexterity and mobility, is a major psychological and physical problem for many patients with a spinal cord injury.
Upper Motor Neuron Bladder
It occurs in Suprasacral Lesion results in a reflex bladder, identify by loss of cortical inhibition of sacral reflex arcs because of disturbance of descending spinal tracts, which leads to detrusor hyperactivity with detrusor sphincter dyssynergia. Generally associated with spontaneous, residual urine volume after the Detrusor Sphincter Dyssynergia and recurrent voiding after the detrusor hyperactivity with high voiding pressure.
Lower Motor Neuron Bladder
It occurs in a Sacral Lesion at S2 – S4 and results in an areflexic bladder, identify by decreased motor stimulation of the bladder and absent or reduced contractility of the detrusor, which means the bladder will not contract no matter how much it fills up. Generally associated with Hydronephrosis and bladder distension, when an over distended bladder causes a reflux of urine into the kidney.
Depending on the location and extent of nerve damage it is possible to have a mixed bladder pattern with elements of lower motor neuron and upper motor neuron bladder.
Sexual Dysfunction
It can be affected by a spinal cord injury either directly or indirectly including sexual intimacy and relationships; the ability to engage in sexual activities; sexual self-view, and reproductive and fertility health. Patients with upper motor neuron lesions retain reflexive but not psychogenic responses, whereas patients with lower motor neuron lesions lose reflexive but retain psychogenic responses, while all retain few abilities for non-genital sexual arousal.
Erectile Dysfunction
Depending on the completeness and level of injury male can attain an erection after a spinal cord injury through either the reflexogenic pathway at S2-S4 or the psychogenic pathway at T11- L2.
Fertility
Sperm production is generally normal, male fertility post a spinal cord injury may be affected after impaired ejaculation and reduced sperm quality, which can result in impaired fertility or complete infertility. The degree and symptoms of infertility will vary depending on the severity and type of the spinal cord injury.
Female fertility and menstruation are hugely unchanged after spinal cord injury though women may cease ovulating after an injury for between 1 – 3 months.
Bone Metabolism Dysfunction
Heterotopic Ossification of the Hip
It is also known as myositis ossificans and ectopic ossification is the formation of pathological bone in soft tissue or muscle, which if severe can lead to ankylosis and impaired function. It generally presents around the joint, particularly in the hip, with the initial signs including swelling around the joint, reduced range of motion, spasticity, and pain, with or without fever.
Osteoporosis
It means porous bone, is a disease characterized by a decrease in bone density, both quality, and mass. In this, bones become increasingly brittle and porous, leading to raising the risk of fracture.
Spasticity
It is a motor disorder characterized by a velocity-dependent increase in tonic stretch reflexes means muscle tone with exaggerated tendon jerks, because of hyper-excitability of the stretch reflex, painful muscle spasms, and clonus.
Pain
Up to 80% of patients with a spinal cord injury have chronic pain, which leads to functional impairment and reduced quality of life and community participation.
There are various types of pain that occur in association with spinal cord injury, and patterns of presentation, intensity, characteristics, and location are highly variable.
Nociceptive
It is associated with the activation of peripheral receptive terminals of primary afferent neurons in response to noxious mechanical, chemical (inflammatory), or ischemic stimuli. Abnormal gait, posture, and overuse of structures such as the shoulder and arm for transfers and wheelchair propulsion result in musculoskeletal pain and chronic overuse injuries, a type of nociceptive pain. Muscle spasm pain is another type of musculoskeletal pain. Visceral pain is less common and arises from irritation, damage, or distention of internal organs such as the bowel or bladder.
Neuropathic
Central neuropathic pain is pain that is started by dysfunction or a primary lesion in the Central Nervous System (CNS), whereas peripheral neuropathic pain is initiated or caused by dysfunction or a primary lesion in the Peripheral Nervous System (PNS).
Fitness and wellness
Muscle atrophy and weight loss are common after a spinal cord injury. Limited mobility leads to a more sedentary lifestyle, at risk of obesity, diabetes, and cardiovascular disease.
A dietitian can help a patient eat a nutritious diet to maintain an adequate weight. Physiotherapists and occupational therapists can help develop a fitness and exercise program.
Psychological
Spinal cord injury can have a negative effect on mental health and many patients experience psychological stress and/or psycho-social distress.
Anxiety and depression
Patients with good mental health are generally capable of coping with stress, but the patient’s response is affected by the extent of injury and cause, and the patient’s current life situation. Proper care and attention to each patient’s way of dealing with their injury psychologically are essential.
How is a spinal cord injury diagnosed?
Medical history and timing are vital factors in the diagnosis of a spinal cord injury. The faster a patient can receive treatment, the higher the chances for recovery from the injury. Also, it is required to understand how the injury occurred. A doctor will need to know if patients have had any of the following prior to their medical emergency:
- Pain in the back or neck
- Previous surgeries or injuries to the neck or back
- Weakness or loss of sensation in arms or legs
- Loss of bladder or bowel control
In the trauma condition, a doctor will check first to make sure the patient has a working airway, has a pulse, and is breathing. The following step in the diagnosis is to assess the patient’s neurologic function by testing their strength and sensation in the legs and arms. If there is a weakness or the patient is not fully awake, the patient is kept on a spine board and in a rigid cervical collar until a full imaging assessment can be complete.
Spinal Cord Injury Physical Examination
A doctor is able to test muscle movement and strength, sensory functions, and reflexes through a physical examination:
- Sensory messages include the feelings of cold, hot, pain, touch, pressure, and body position.
- Motor messages are sent to the muscles in the hands, arms, fingers, toes, legs, chest, and other parts of the body. These messages tell the muscles when and how to move.
- Reflex messages are involuntary, and they help to keep the safe body with instinctive reactions.
This examination will help a doctor determine if there is damage to the thoracic, cervical, lumbar, or sacral vertebrae.
Imaging tests can include:
X-rays
It can reveal vertebral or spinal column problems, tumors, fractures, dislocations (bones knocked out of place), and degenerative changes in the spine.
CT scan
It can provide a clearer or pixel image of abnormality seen on an X-ray. This scan uses computers to form a number of cross-sectional images that can define disk, bone, and other issues.
MRI
It uses radio waves and a strong magnetic field to produce computer-generated images. This test is useful for looking at the spinal cord and identifying blood clots, herniated disks, or other masses that can compress the spinal cord.
Electromyogram
It uses to check the electrical activity in nerve cells and muscles if there are co-exist peripheral nerve injuries.
Myelogram
This is an X-ray of the spine taken after a dye is inserted.
Somatosensory evoked potential (SSEP) testing or magnetic stimulation
These tests may show if nerve signals can pass through the spinal cord.
What are the treatments for spinal cord injury (SCI)?
Unfortunately, there is no way to change damage to the spinal cord. But, the treatment focuses on preventing more injury and empowering patients to return to productive and active life.
Emergency period
Urgent medical attention is essential to reduce the effects of the neck or head trauma.
An emergency person generally immobilizes the spine as quickly and gently as possible using a rigid carrying board and a rigid neck collar, which they use during transport to the hospital.
Acute (early) stages of treatment
In the emergency room, doctors focus on:
- Preventing shock
- Maintaining the ability to breathe
- Immobilizing the neck to prevent more spinal cord damage
- Avoiding possible complications, such as urine or stool retention, cardiovascular or respiratory difficulty, and formation of deep vein blood clots in limbs.
Patients will usually be admitted to the intensive care unit for treatment.
Surgery
Doctors may use surgery to remove tissue or fluid that presses on the spinal cord (decompression laminectomy); remove disk fragments, bone fragments, or foreign objects; fuse broken spinal bones, or place spinal braces. Surgery is needed to stabilize the spine to prevent future deformity or pain. There are various surgical approaches but generally, vertebrae are realigned and surgical stabilization is achieved by posterior or anterior fixation, or a combination of the two, with or without spinal decompression.
Pharmacological management
Methylprednisolone (Medrol)
This Glucocorticoids steroid medication is administered within 8 hours of injury, which may:
Improve blood flow.
Reduce inflammation.
Preserve nerve function.
Thyrotropin-releasing Hormone (TRH) shows antagonistic effects against the post-injury mediators.
Polyunsaturated Fatty Acids (PUFA) such as Docosahexaenoic Acid (DHA)
Immobilization
Patients managed conservatively usually need bed rest with the spine immobilized for a period of 6 – 12 weeks. Depending on the degree of severity, patients may have to be maintained in spinal alignment by some type of pillow wedge (thoracic, lumbar, and sacral lesions) or skull traction (cervical lesions) with tight restrictions placed on therapies. After this period of immobilization, the patient is mobilized in a wheelchair, with a spinal orthosis, that is worn for more few months. In a few cases, immobilization may be done with extensive bracing e.g. halo-thoracic brace.
Cellular Therapy management
It is used to provide functional recovery of the problem through axonal restoration and regeneration.
Schwann Cell is used for the repair of the spinal cord.
Olfactory Ensheating Cells are useful for promoting axonal remyelination and regeneration after injury.
Bone Marrow derived Mononuclear Cells transplantation is safe, feasible, and has a high degree of outcome improvement.
Ongoing care
After the initial condition or injury stabilizes, doctors will focus to prevent secondary complications, such as deconditioning, pressure ulcers, muscle contractures, bowel and bladder problems, respiratory infections, and blood clots.
The length of patients’ hospital stay will depend on their condition and medical issues. Once they are well enough to participate in treatment and therapies, they might transfer to a rehabilitation period.
Medicines
It might be used to manage some of the effects of spinal cord injury. These medicines control muscle spasticity and pain and improve bowel & bladder control, and sexual functioning.
Rehabilitation
Rehabilitation team members include a physiotherapist, an occupational therapist, a recreation therapist, a rehabilitation nurse, a rehabilitation psychologist, a social worker, a dietitian, and a physiatrist.
- During the starting phases of rehabilitation, therapists usually emphasize strengthening and maintaining muscle function, redeveloping fine motor skills, and learning ways to adapt to do daily tasks.
- Education on the effects of a spinal cord injury and how to prevent complications, and give advice on rebuilding a patient’s life and increasing independence and quality of life.
- Patients will be taught various new skills, and use equipment and technologies that can help them live on their own. They will be encouraged to resume their favorite hobbies, participate in fitness and social activities, and return to the workplace or school.
Medical devices
Inventive and new medical devices can help patients become more independent and mobile. These include:
Modern wheelchairs
Lighter weight and improved wheelchairs are making patients more mobile and comfortable. Few patients need an electric wheelchair. Some wheelchairs can travel over rough ground, climb stairs, and elevate patients to reach high places without help.
Computer adaptations
For patients who have limited hand function, computers can be hard to operate. Computer adaptations vary from simple to complex, such as voice recognition and keyguards.
Electronic aids to daily living
Devices can be turned off or on by voice-controlled or switch and computer-based remotes.
Electrical stimulation devices
It is also called functional electrical stimulation systems, use to control leg and arm muscles to allow patients to stand, walk, grip, and reach.
Physiotherapy treatment for spinal cord injury
The acute treatment and rehabilitation of SCI depend on the type and level of injury to the spinal cord. Patients require initial treatment in an intensive care unit with the rehabilitation typically initiate in the acute care setting, then extended treatment in a specialized Spinal Injury Unit. Inpatient treatment can last from 8 – 24 weeks, with follow-up outpatient rehabilitation from 3 – 12 months, usually then yearly functional and medical reviews.
The treatment of patients with a Spinal Cord Injury can be divided into 3 Phases;
- Acute
- Sub-acute (Rehabilitation)
- Chronic (Long Term)
During the acute and subacute period of management, rehabilitation strategies focus more on the prevention of secondary complications, addressing underlying impairments and maximizing function, and promoting neuro recovery. In the chronic period, assistive or compensatory approaches are used.
Acute Phase
In this early phase post-injury, physiotherapy treatment is predominantly involved in the management and prevention of circulatory and respiratory complications, along with minimizing the impact of immobilization on patients e.g. pressure ulcer and contracture development.
Objectives
- To educate and support the patient, family, carers, and staff
- To manage and monitor the neurological status
- To give a prophylactic respiratory protocol to treat respiratory conditions and any complications
- To achieve an independent respiratory status
- To maintain the full range of motions of all joints within the limitations given by the stability of the fracture
- To strengthen and maintain all innervated muscle groups
- To improve functional patterns of activity
Respiratory Function
Common secondary complications include atelectasis, hypoventilation, pneumonia, and secretion retention. Patients with C1-3 quadriplegia need mechanical ventilation, while most patients with C4 quadriplegia will be able to breathe independently. Patients with SCI C4 to T12 can breathe independently, but they might have reduced vital capacity and difficulty in raising intra-abdominal pressure for forced-expiratory techniques (FETs) or an effective cough.
Physiotherapy management includes increased ventilatory and secretion clearance techniques. Secretion clearance techniques include percussions, shaking and vibrations, postural drainage, and suctioning. Treatment to improve ventilation includes positioning, deep breathing exercises, abdominal binders, incentive spirometry, and inspiratory muscle training. Other medical equipment often used to improve ventilation are bi-level positive airway pressure (Bi-pap) and continuous positive airway pressure (CPAP).
Range of movement of all joints
Reduced ROM may lead to contractures because of poor positioning and immobility and increased tone and spasticity. These exercises can do at least 2-3 times a day in the presence of spasticity and in a flaccid period at least once a day.
Treatment techniques should include positioning in the lengthened position, passive stretches, and other common hypertonic treatment techniques such as heat, compression, and sustained deep pressure.
Stretching
It should be done to protect the tenodesis effect in patients without active fingers and wrist extensions that are not fully stretched.
Positioning of the joints
It is essential to maintain the optimal muscle tonus and protect the articular structure. Pillows and sandbags can be useful in positioning. If these are not able to provide positioning, it can be achieved with more rigid orthotics or plaster splints. Ankle foot orthosis, static ankle-foot orthosis or knee-ankle foot orthosis, etc. are mainly used for this purpose.
Prevention of Pressure sore
In the acute phase, treatment includes passive pressure care, such as frequent rolling regimes and mobilizing, nutrition, adequate skin moisturizing, and monitoring. In the sub-acute and chronic phases, patients will be taught how to perform frequent self-lift techniques to relieve pressure.
Strengthening and maintaining innervated muscles
Functional strength training and progressive resistance training are useful in maintaining and strengthening innervated muscle groups. Shoulder exercises performed with elastic bandages can be effective to decrease shoulder pain
Cardiac care
Orthostatic hypotension is seen in patients with a long period of lying in bed. Syncope can be observed in patients while sitting and being lifted up because of low blood pressure. A tilt table can use for patients with this condition, initiate from 45 degrees for 30 min a day. The degree is increased according to the patient’s state or complaints. Standing upright stimulates the blood pressure to a persistent and sufficient limit. When the patient comes to the upright position with a tilt table, the patient does balance exercises and a sitting position on the edge of the bed 3-4 times a day should be done to maintain position.
Sub-acute (Rehabilitation) Phase
Objectives
- To organize an interdisciplinary process that is patient-focused, coordinated and comprehensive.
- To do physical motor functional activities with early intervention and treatment to prevent further complications.
- To improve patients’ independence in activities of daily living, such as eating, bathing, grooming, dressing, and mobility.
- To gain functional independence, by use of verbal or physical equipment to facilitate this independence.
- To maintain and achieve successful reintegration into the social community.
The range of activities used by physiotherapists during the rehabilitation period varies depending on the type and level of injury. The three most general therapy activities for patients with high-level quadriplegia were – range of motion or stretching, strengthening, and transfers; while for patients with low quadriplegia, more time was spent on transfers compared to strengthening. For patients with paraplegia, physiotherapy activities include transfers, then a range of movement or stretching, and strengthening.
Bed mobility and transfers
C6 and lower level SCI can gain 5 motor skills;
- rolling by using momentum
- mobilizing from supine to long-sitting
- unsupported short & long sitting
- lifting vertically
- transfers
C6 quadriplegia may have a few challenges, but these 5 motor skills can do with some modifications. With rolling, C6 quadriplegia should swing arms across their body instead of over-head and externally rotate shoulders. During an unsupported sitting, C6 quadriplegia should lock elbows in extension and externally rotate shoulders to maintain balance. Vertical lifting for patients with C6 quadriplegia can do passively extending elbows, depressing shoulders and externally rotating shoulders to weight bear with hands placed anteriorly to the pelvis.
Wheelchair (WC) mobility
- Patients with C1-4 quadriplegia require powered-WCs. These may be controlled by sip and puff, head array or chin movements.
- Patients with C5 quadriplegia mostly use powered-WCs controlled by hand movement.
- Patients with C6-8 quadriplegia can independently mobilize with a manual WC but they might use a hand-controlled WC as an option.
- patients with SCI lower than C8 will be able to independently transfer with a manual WC.
Patients with SCI should be started with their new way of mobilization. Turning, closing and opening doors, going up and down inclines, going over and around obstacles, as well as mobilizing outdoors and indoors are essential activities to practice to ensure independent and safe mobility.
Gait and standing
Gait training, balance, and strengthening exercises were the most common physiotherapy activities in patients with spinal cord injury.
standing has many benefits including orthostatic hypotension, emotional well being, spasticity, bone mineral density, and bowel and bladder function. Standing can gain by using assistive devices such as; standing WCs, tilt tables, and standing frames. Patients with paraplegia can be able to stand in parallel bars using orthoses or knee-extension splints.
Gait training is possible among patients with complete paraplegia to partially paralyzed lower extremities by using walking aids and orthoses such as hip-knee-ankle-foot and knee-ankle-foot orthoses.
Long Term Phase
Patients with spinal cord injury, depending on the type and level of lesion, may have many complex needs and face wide-ranging, drive or use public transport, long-term restrictions in their ability to live independently, return to education or work, participate in social and leisure activities.
Objectives
- To achieve high-level mobility goals required for community and social participation
- To monitor the recovery of all function
- To reinforce carer and family training
Ambulation
The most vital goal is a realization of the independent mobilization for both incomplete and complete paraplegic patients during the chronic period. Ambulation can be domestic, social, and aimed at exercise. Patients can able to walk 50 m with assistive devices or unaided for social ambulation.
Walkers, orthoses, and crutches are essential to provide chronic stage ambulation. Patients with pelvic control can walk with crutches or orthosis outside the parallel bars. If the quadriceps femoris muscle strength is normal, patients can walk with orthosis and elbow crutches without needing a wheelchair. In patients with complete injury of C8-T12, ambulation can be achieved by a parawalker with hip guidance orthosis, both outside and in the house.
Oxygen consumption, walking speed, and energy expenditure can vary depending on the shape, weight, and type of material devices used by patients. RGO (Reciprocating Gait orthosis) is one of them. The patient’s muscle mass must be increased and excess weight reduction and increased aerobic capacity must be maintained, for effective use. Hybrid walking devices are used by adding Functional Electrical Stimulation to orthosis, which is better for walking. Robotic training is developing day by day and is a new approach.
House modifications
- It is essential for patients with SCI to have independent activities of daily living.
- The door width should be 86.5 cm for battery-assisted wheelchairs and 81.5 cm for manual wheelchair access.
- The ideal height of electric switches and boards should be 91.5 cm.
- Adequate heat and insulation must be provided at home.
- Door handles must be the “leverage-shaped” type and the height of the door sills should not interfere with the passage of a wheelchair for quadriplegic patients.
- The surface should be hard and carpets should be removed to maneuver the wheelchair.
- Bathtubs must have handles and should be mounted on the wall.
- The height of kitchen materials should be accessible to the patient.
- A ramp at the entrance to the house is must required.
Restore the patient’s psychological and emotional state
One of the important functions of this phase because of the high incidence of depression in patients. Consultation with a psychiatrist is needed for depression and psychotic behavior. Occupational therapy and finding the patient’s role in society are the most vital factors in restoring the psychological state. Occupational therapy allows patients to be more social, deal with psychological problems like depression and use their own functions for creative jobs.
Occupational therapy
Occupational therapy is implemented and planned depending on the cultural and social characteristics of patients, level of education, personality traits, values, interests, attitudes, and behaviors before and after the injury. Pictures, crafts, music, ceramic work, and a variety of activities like sports and entertainment are planned and implemented to focus on the purpose of the occupational treatment.
It helps redevelop fine motor skills. Bowel and bladder management programs teach basic toileting routines and learn techniques for self-grooming.
Vocational rehabilitation
It initiates with an assessment of basic work skills, current dexterity, and cognitive and physical capabilities to determine the likelihood of employment. A vocational rehabilitation specialist identifies potential workplaces, helps arrange for a user-friendly workplace, and determines the type of assistive devices that will be needed. For patients whose disabilities prevent them from returning to the workplace, therapists focus on encouraging productivity through participation in activities that provide self-esteem and a sense of satisfaction. This could include hobbies, educational classes, memberships in special interest groups, and participation in community and family events.
Recreation therapy
It encourages patients to build on their abilities so that they can participate in athletic or recreational activities at their level of mobility. Engaging in athletics and recreational outlets helps patients achieve a more balanced and normal lifestyle and also provides opportunities for self-expression and socialization.







4 Comments