Symphysis Pubis Dysfunction (SPD)
Table of Contents
What is a Symphysis Pubis Dysfunction?
Symphysis pubis dysfunction (SPD) is a condition that affects the pelvic area, particularly the joint known as the symphysis pubis. This joint connects the two halves of the pelvis at the front of the body. SPD occurs when there is an abnormal movement or instability in this joint, leading to pain and discomfort.
The symphysis pubis may partially or completely rupture in severe cases of SPD. When the gap widens to more than 10 mm, this is diastasis of the symphysis pubis (DSP).
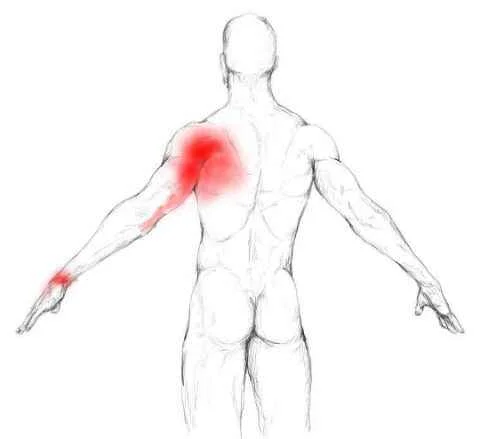
Pubic Symphysis Dysfunction has been defined as a group of signs and symptoms of pelvic discomfort and pain, including pelvic pain radiating to the upper thighs and perineum. These are caused by the physiological pelvic ligament relaxation and increased joint mobility during pregnancy. The severity of symptoms ranges from mild discomfort to severe pain.
Pubo-sacroiliac arthropathy, pelvic insufficiency, symphysis pain syndrome, pelvic joint syndrome, pelvic girdle pain, pelvic relaxation syndrome, and, most importantly, symphysis pubis dysfunction have all been discussed in the literature.
Understanding the causes, symptoms, and management of SPD is crucial for effective treatment and improving the quality of life for individuals affected by this condition.
Clinically Relevant Anatomy
The Pubic Symphysis
The pubic symphysis is the perineum’s anterior boundary, situated on the anterior part of the pelvis. The pubis symphysis is a joint with cartilage formed in the centre of the medial plane by the pubic bones. During activity, the joint holds the two pelvic bones together and is stable.
The symphysis forms a stable pelvic ring in collaboration with the sacroiliac joints. This ring provides only limited mobility.
The pubic symphysis is a cartilaginous joint that consists of a fibrocartilaginous interpubic disc. The four ligaments interact with the pubic bones. The superior pubic ligaments extend from the superior part of the pubis to the pubic tubercles. The arcuate pubic ligaments blend with the fibrocartilaginous disc to form the lower border of the pubic symphysis. The arcuate ligament, which is also the strongest, provides the majority of joint stability. The four ligaments work together to counteract shear and tensile stresses.
The disc connects the two pubic bones’ adjacent surfaces. A thin layer of hyaline cartilage covers both of these surfaces. There are papilliform elevations with reciprocal depressions and ridges at the junction, which is not flat.
This disc is very small in children, and the hyaline cartilage is very wide, but it develops in the opposite direction. In men, the disc is higher, smaller, and narrower. The symphysis pubic gap is normally 4-5 mm wide in women and widens 2-3 mm during the last trimester of pregnancy. This is required to make the baby’s delivery easier. With symphysis pubis dysfunction, the joints become more relaxed, allowing for pelvic girdle instability. A diastasis of the symphysis pubic occurs when the gap is equal to or greater than 10 mm.
Pelvic Floor
The Muscles of the Pelvic floor are divided into 3 layers. The first is the superficial perineal layer, which includes the Bulbocavernosus, Ischiocavernosus, Superficial transverse perineal, and external anal sphincter (EAS) and is innervated by the pudendal nerve.
The deep urogenital diaphragm layer (innervated by the pudendal nerve) includes the Compressor urethra, Uretrovaginal sphincter, and Deep transverse perineal.
The third layer is the pelvic diaphragm (innervated by sacral nerve roots S3-S5), which includes the Levator ani, the pubococcygeus (pubovaginalis, puborectalis), the iliococcygeus, the coccygeus/ischiococcygeus, the Piriformis, and the Obturator internus.
The pelvic floor muscles support the organs that lie beneath it. The sphincters (anal and urethral sphincters, respectively) provide conscious control over the bowels and bladder, allowing us to control the release of faeces/flatus or urine, as well as prevent and delay emptying until it is convenient.
When the pelvic floor muscles contract, they raise the internal organs and tighten the sphincter openings of the vagina, anus, and urethra. The passage of faeces and urine is enabled by the relaxation of the pelvic floor muscles.
Pregnancy changes all of these muscles, as well as their function.
Causes of sympathetic pubis dysfunction
When pregnant, your body produces a hormone called relaxin, which relaxes the ligaments between your left and right pelvic bones. This hormone may be produced by your body as early as 10 weeks into your pregnancy.
Loosening your ligaments’ grip on the joint allows it to move around more freely. When it comes time for your baby to be born, the extra movement allows your left and right pelvic bones to widen. These changes in the ability of your pelvic bones to move allow for vaginal childbirth.
This loosening is intended to increase your range of motion so that you can give birth, but it also means that your joints may become unbalanced and mobile. Such may lead to pain and discomfort.
Although this slackening is intended to aid in birth, these hormones can sometimes be produced in early pregnancy. SPD symptoms may appear long before it is time to give birth.
Pelvic pain is thought to be influenced by the baby’s weight and position. SPD symptoms usually worsen as the pregnancy progresses.
SPD occurs much less frequently outside of pregnancy, but it does occur. Other causes of SPD include pelvic injuries and conditions such as osteoarthritis. There is no identified cause in some instances.
Symptoms of Symphysis Pubis Dysfunction
Certain of the symptoms of symphysis pubis dysfunction include:
- Shooting pain in the lower abdomen
- Pain in the lower back that radiates into the abdomen, groin, thigh, and/or leg
- Pain when performing certain movements, such as putting weight on one leg or spreading your legs apart
- Walking, rolling over in bed, going up and down stairs, bending forward, or rising from a seated position all cause pain.
- Hearing or feeling a snapping, clicking, or grinding sensation in the lower pelvic area
- Pain while having sex
- Fatigue.
Keep in mind that the pain you may experience as a result of SPD can range from mild to severe.
SPD pain is frequently exacerbated by:
- Lifting
- Walking, bending forward, or rising from a chair are examples of hip-related movements.
- Sexual interactions
- Long periods of sitting or standing.
Diagnosis of Symphysis Pubis Dysfunction
Your provider can determine whether you have symphysis pubis dysfunction in several ways.
Your provider will review your medical history to determine whether you are pregnant or have had an injury that could have harmed your pubic symphysis joint.
A physical exam may be performed by your provider to check for tenderness, pain, or swelling. Your doctor may perform tests to determine how easily you can perform certain movements.
Your provider may examine your pelvis joint more closely using ultrasound, CT scan, or X-ray. If you are pregnant, your provider will recommend a fetal-safe imaging procedure.
Complications of Symphysis Pubis Dysfunction
SPD isn’t harmful to your baby, and most women with the condition can still give birth vaginally. However, chronic pain can cause sadness or even depression, which is thought to be harmful to your baby.
Although the symptoms of SPD do not usually go away until after you give birth, there are many things you can do to reduce your pain. For this reason, getting help is essential.
If you have SPD, the Pelvic, Obstetric, and Gynaecological Physiotherapy group in the United Kingdom recommends that you avoid the following activities:
- putting all of your weight on one leg
- lifting while twisting and bending
- You’re carrying a child on your hip.
- bending your knees
- sitting on the ground
- twisted position of sitting
- prolonged periods of standing or sitting
- hefty loads, such as wet laundry, shopping bags, or a toddler
- vacuuming
- dragging heavy objects like a shopping cart
- carrying everything in one hand
Treatment of Symphysis Pubis Dysfunction
The pain in your pelvis will usually subside a few months after your baby is born. When your body no longer produces relaxin, your ligaments tighten and the joint moves less. Meanwhile, you and your doctor can decide how to best manage your pain. Among the options are:
- NSAIDs are being taken.
- Wearing comfortable shoes.
- Applying an ice pack to your pelvic region.
- Sleep using a pillow in between your legs.
- Wearing a pelvic support belt (pregnancy belt).
- Squeezing your legs together as you exit your vehicle.
Getting personalized care can help you manage your symptoms. To relieve stress and strain in your body, your provider may recommend that you see a physical therapist, chiropractor, acupuncturist, or masseuse.
Your provider may teach you stretches and exercises to protect your pelvic area and improve your stability. Keep in mind that the exercises you do during pregnancy may differ from those recommended by your provider after pregnancy.
Learning how to move safely is also essential. When you are in pain, it is natural to move differently to find relief. However, it is easy to overcorrect and put undue strain on other joints in the process. Your provider can advise you on how to relieve pain without causing harm to other joints.
Physiotherapy treatment
The first line of treatment for SPD is physiotherapy. Physiotherapy’s goal is to:
- reduce your discomfort
- enhance your muscle function
- improve the stability and position of your pelvic joints
A physiotherapist can perform manual therapy to ensure that your pelvis, spine, and hip joints move normally. They will also be able to provide you with exercises to strengthen your pelvic floor, back, stomach, and hip muscles.
They may suggest hydrotherapy, which involves doing exercises in water. Being in the water can relieve joint stress and allow you to move more freely. The physiotherapist can advise you on the most comfortable positions for sex, labour, and birth.
Pain medications or TENS therapy may be prescribed in severe cases of SPD. You may also be assisted, such as crutches or pelvic support belts. The application of heat or cold to the affected area may alleviate pain or swelling.
Exercises to Help Symphysis Pubis Dysfunction
Squeezes from the Pelvic Floor
Working the muscles on the inside of your pelvis can assist in the support of your pelvic bones, internal organs, and baby.
- Determine the location of your internal pelvic muscles. Consider the sensation of holding your urine. Your pelvic floor muscles are the ones you’re squeezing.
- Sit in a firm chair in a comfortable position. Squeeze your pelvic floor muscles up and in slowly. preparing to put out it, hold it for ten seconds. Do this ten times.
- As hard as you can, pulse your pelvic muscles up and in, then immediately release. Do this ten times.
Exercises to Improve Stability
Your abdominal muscles are also important for pelvic stability. This exercise gradually strengthens these muscles.
- Find a comfortable position in which you can maintain a straight back. Place one hand just above your pelvis on your stomach.
- Inhale slowly through your nose, then exhale slowly while pulling your stomach in towards your spine.
- Hold this squeeze for up to ten seconds while breathing normally.
- Repeat up to ten times per day.
Stretches of the Inner Thigh
Stretching your thighs apart can help to relax tense hip muscles and prepare you for labour.
- With your feet flat on the ground, take a seat in a chair. Step your feet as far apart as possible while keeping your knees bent at a 90-degree angle.
- Spread your knees out and place the hands on the inner sides of your thighs. You will experience a nice stretch.
- Maintain this posture for 30 seconds.
- Repeat three to five times per day.
Pelvic Tilts
This exercise can help you loosen up tight back muscles, which can relieve pelvic pain.
- Sit on the edge of a firm-seated chair.
- Tilt your pelvis backward so that you appear to be slumping forward.
- Tip your pelvis forward to create an arch in your lower back.
- Repeat the rocking motion back and forth ten times.
- Repeat three or four times per day.
Back Stretches
Stretching your back may assist the pelvic joints moving and relieve pain caused by pelvic pressure.
- Lean ahead onto a table with your back to the floor. arrange your weight on your forearms and elbows.
- Lean back slowly until there is a stretch in your back and thighs. is holding for ten seconds before returning to neutral.
- Repeatedly move the hips from side to side.
- Repetition as many times as needed until you’re at comfort.
Side Stretches
This stretch can assist in relieving pressure on either side of your pelvis.
- With your feet flat on the ground, take a seat in a chair. Straighten one arm in the air.
- Lean away from your arm and look away from it. Feel a stretch along your side as you arch your arm in the air over your head.
- Hold this position for ten seconds before repeating with the opposite arm.
- Three to four times a day, repeat the entire stretch.
Summary
Symphysis pubis dysfunction (SPD) is a condition where the pelvic girdle is relaxed, causing pelvic discomfort and pain. It can be caused by physiological pelvic ligament relaxation and increased joint mobility during pregnancy.
Symptoms include shooting pain in the lower abdomen, pain in the lower back, pain during certain movements, and fatigue. Diagnosis involves reviewing medical history, physical exam, and imaging.
SPD is not harmful to the baby, but chronic pain can cause sadness or depression. Treatment options include NSAIDs, comfortable shoes, ice packs, sleep, pelvic support belts, and squeezing legs together. Personalized care, such as physical therapy, can help manage symptoms. Physiotherapy is the first line of treatment, aiming to reduce discomfort, enhance muscle function, and improve pelvic joint stability.
Physiotherapists can perform manual therapy, provide exercises to strengthen muscles, and suggest hydrotherapy for hydrotherapy. Pain medications or TENS therapy may be prescribed in severe cases. Assistance may include crutches or pelvic support belts.
FAQs
This exercise can help you loosen up tight back muscles, which can relieve pelvic pain. Step 1: Sit on the edge of a firm-seated chair. Step 2: Tilt your pelvis backward so that you appear to be slumping forward. Step 3: Arch your lower back by tilting your pelvis forward.
Symphysis pubis dysfunction (SPD) is a group of symptoms that cause pelvic pain. Treatment may alleviate your pain while also improving muscle function and pelvic joint stability. SPD is most common during pregnancy when your pelvic joints stiffen or move unevenly.
The presence of laxity as a result of a hormonal link appears to be undisputed. However, there is no complete disclosure. Other factors that contribute to SPD include physically demanding work during pregnancy, fatigue, poor posture, and a lack of exercise.
Pubic Symphysis dysfunction is a common and excruciatingly painful condition that affects both men and women. A sports injury can cause it, but it is most common during or after pregnancy. Dysfunction occurs when a joint becomes too lax, resulting in excessive movement and pain.
Symphysis pubis dysfunction (SPD), also known as pelvic girdle pain (PGP), occurs when the ligaments that normally keep your pelvic bone aligned during pregnancy become overly relaxed and stretchy soon before birth (things are supposed to loosen up as delivery approaches).
References:
Professional, C. C. M. (n.d.). Symphysis Pubis Dysfunction. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/22122-symphysis-pubis-dysfunction
Young, B. (2023, April 20). What Is Symphysis Pubis Dysfunction? Healthline. https://www.healthline.com/health/symphisis-pubis-dysfunction
Pubic Symphysis Dysfunction. (n.d.). Physiopedia. https://www.physio-pedia.com/Pubic_Symphysis_Dysfunction
P. (2023, March 13). What Is Symphysis Pubis Dysfunction (SPD)? Web-Pampers-US-EN. https://www.pampers.com/en-us/pregnancy/pregnancy-symptoms/article/symphysis-pubis-dysfunction
Best Exercises for Symphysis Pubis Dysfunction. (2020, November 23). WebMD. https://www.webmd.com/baby/best-exercises-symphysis-pubis-dysfunction
Miles, K. (2023, November 24). Pubic symphysis dysfunction (SPD) in pregnancy. BabyCenter. https://www.babycenter.com/pregnancy/your-body/pubic-symphysis-dysfunction_40007958