Use of Traction in Physiotherapy: Spinal Lumbar Cervical Traction
Table of Contents
CERVICAL TRACTION | LUMBAR TRACTION | SPINAL TRACTION
~Traction is the act of drawing or pulling and relates to forces applied to the body to stretch a given part or to separate 2 or more parts. Currently, traction is used effectively in the treatment of fractures.
~In physiotherapy practice, the use of traction is often limited to the cervical or lumbar spine with the goal of relieving pain in, or originating from, those areas.
~Since the days of Hippocrates, correction of scoliosis also has involved traction. There are various types of traction currently in clinical use.
~The most common are mechanical, hydraulic, or motorized, manual, and autotraction.
~Mechanical forms of traction use a hydraulic or motorized pulley system with weights, along with a harness or sling device to attach to the patient’s body.
~Manual traction involves the therapist using his or her hands on the patient’s body, with the body weight of the therapist providing the tractive force.
~Autotraction is controlled by the patient pulling on bars or handles at the head of the table, without the direct involvement of a therapist.
~Gravitational traction with a tilt table and underwater variations of traction are also in clinical and home use but are less frequently employed than the other forms described.
Physiologic Effects of Traction:
~In the cervical spine, the most reproducible result of traction is elongation. In a classic study, Cyriax
reported applying force of 300 pounds manually, with a resultant 1 cm increase in cumulative lumbar spine interspace distance.
~Studies have shown that the optimum weight for cervical traction to accomplish vertebral separation is 25 pounds. Additionally, 2-20 mm elongation of the cervical spine has been shown to be achievable with 25 or more pounds of tractive force.
~Studies have demonstrated that anterior intervertebral space shows the most increase in cervical flexion of 30°.
~Traction in the extended position generally is not recommended, because it is often painful and may increase risk of complications from vertebral basilar insufficiency or spinal instability.
~Once friction is overcome in the lumbar spine, the major physiologic effect of traction is elongation.
Investigators have reported widening of lumbar interspaces requiring between 70-300 pounds of pull.
~This widening averaged up to slightly more than 3 mm at one intervertebral level. The length of time that the separation persists remains indeterminate, with studies documenting distraction durations of 10-30 minutes after
treatment.
~Data on dimensional and pressure changes of lumbar disks caused by traction are not conclusive. Decreases in intradiscal pressure with 50-100 pounds of traction have been documented, but evidence exists that some applications actually cause an increase in intradiscal pressure.
~Therefore, evidence is inconclusive, with much information favoring at least a temporary reduction of the herniated component of an abnormal lumbar disk with concomitant traction.
~Some theories on the physiologic effects of traction suggest that stimulation of proprioceptive receptors in the vertebral ligaments and monosegmental muscles may alter or inhibit abnormal neural input from those structures. As with other theories to explain the physiology of traction, there is little to no empirical evidence to fully
support it.
Outcome studies related to Traction:
~Criteria have been suggested that would allow the true effects of traction to be delineated. These criteria include
(1) randomized controlled trials,
(2) blind outcome assessments,
(3) equivalent co-interventions,
(4)monitored compliance,
(5) minimal contamination and attrition,
(6) adequate statistical power and description of study design and interventions,
(7) relevant, functionally oriented outcomes.
~No traction outcome study to date has incorporated these criteria. Despite inadequacies in the literature, randomized, controlled trials that meet some of these criteria do provide some insight into the efficacy of traction as a treatment modality. A review of randomized, controlled trials of traction analyzed English language studies done between 1966 and 2001.
The only conclusion that could be drawn, based on this review, was that there exists poor evidence to support the effectiveness of traction for back pain relief. A subsequent review, by Graham and colleagues, arrived at 2 clinical conclusions; one conclusion favors the use of intermittent traction over a continuous protocol, and the other does not support the use of continuous traction. The reviewers felt there was inconclusive evidence overall for either form of traction, based on the methodologic quality of the numerous studies reviewed.
~A systematic literature review by Clarke and colleagues further supported the aforementioned conclusions regarding traction for low back pain. Through an examination of randomized clinical trials, the authors determined that the evidence did not support the intermittent or continuous use of traction alone to treat low back pain in mixed groups of patients suffering from this condition, whether or not sciatica was present.
~Owing to inconsistent results and methodologic problems in most of the studies involved, the authors also did not recommend traction for patients with sciatica. Clarke and his coauthors also said that because the available research was insufficient, they could not comment on the use of traction in combination with other therapies.
~What can be reasonably derived from these studies is that more work needs to be done to be able to make evidence-based recommendations on the application of traction for back pain. Additional evidence is also needed to evaluate the optimal type and position of the tractive forces for various clinical conditions, as well as to assess the use of traction as a component of a patient’s treatment, rather than as an isolated modality.
~The Agency for Health Care Policy and Research (AHCPR) review of the literature on traction resulted in a conclusion that “spinal traction is not recommended in the treatment of acute low back problems.”
~”There is little evidence to support the continued use of traction in the management of acute low back pain (LBP).” Despite these recommendations, the widespread use of lumbar traction remains relatively high, with up to 20% of patients in the United States and 30% of those with low back pain and sciatica receiving traction as a treatment.
~Studies that claim improvement after traction report modest and very short-term improvements, with limited or no improvement in overall function. Additionally, these studies have significant design flaws. While a particular group of patients may benefit from a particular type of traction for either short-term or long-term improvement in functional outcomes, the literature currently does not identify this patient population.
~In addition, it is important to note that although high-quality evidence supporting the use of traction for the treatment of low back pain is currently scarce, there is likewise insufficient data in the literature to show that traction is not effective for this problem.
Cervical Traction:

TECHNIQUES FOR APPLYING TRACTION
~Cervical traction generally is accomplished with a free-weight–and––pulley system or an electrical, motorized device. Adequate pull is achieved by using a head or chin sling attached to a system that can provide pull in a cephalic direction.
~Motorized devices are applied easily but require the patient to be attended to. Free-weight–and–pulley systems often are used in the home with 20 or more pounds of water or sand and a pulley system attached to a door. If a tractive force of only 20 pounds is possible, the system is likely to fail to achieve therapeutic results.

~Advise patients not to attempt cervical traction at home alone, because they may find themselves in uncomfortable positions and may need assistance doffing the traction devices.
~Most home traction systems are difficult for patients to set up without assistance. Home cervical traction may cause an increase in pain or may fail to produce significant pain relief unless professionally monitored on a periodic basis. At the initiation of home traction, the patient should be required to demonstrate proper use of equipment to the satisfaction of the prescribing physician or therapist.
~In the lumbar spine, adequate pull with weights and pulleys or motorized devices to achieve vertebral distraction usually can be obtained with the proper apparatus. Generally, a harness is attached around the pelvis (to deliver a caudal pull), and the upper body is stabilized by a chest harness or voluntary arm force (for the cephalic pull).
~Motorized units have the advantage of allowing intermittent traction with less practitioner intervention. If the goal of tractive force is to distract lumbar vertebrae, 70-150 pounds of pull usually are needed. Friction between the treatment table and the patient’s body usually requires a tractive force of 26% of the total body weight before effective traction to the lumbar spine is possible.
~Many traction devices use a split table that eliminates the lower body segment friction.
~Body weight theoretically should provide enough pull to distract lumbar vertebrae and eliminate mechanical devices.
~Gravity traction is applied almost exclusively in the lumbar region. After 10 minutes of inversion traction, documented increases in intervertebral separation are noted; however, side effects also are frequently reported, including increased blood pressure, periorbital petechiae, headaches, blurred vision, and contact lens discomfort.
~A study from Hungary re-analyzed an old method of applying traction in the treatment of patients with lumbar or cervical diskopathy.
~Patients were vertically suspended by a special harness in a warm-water bath, with a specified amount of weight applied to the lower limbs. One harness allowed for traction on the lumbar spine, while the other focused on the cervical region. The study participants had land-based physical therapy exercises and weight bath therapy, while a control group only had the exercises.
~Therapeutic benefit was perceived to be greater by patients treated with a combination of the weight bath and exercise than it was by patients in the control group, according to results following treatment and at 3-month follow-up.
~The treatments were well tolerated, and no adverse effects were reported. Although the study concluded that this form of traction treatment “is a relatively straightforward, non-invasive, and low-cost intervention that can be implemented anywhere,” further research may be needed to corroborate the findings of this pilot study. Such investigation may need to be supplemented with cost and feasibility data before widespread implementation is initiated.
Indications For Traction:
~The literature does not give clear indications of what types of neck or lower back pain may improve from traction. Studies strongly suggest that traction does not produce a significant influence on the long-term outcome of neck pain or lower back pain.
~Practitioners who rely on sound scientific advice may use traction rarely. Practitioners who are receptive to empirical treatments may be amenable to the concept that traction may separate vertebrae and decrease the size of herniated disks, thereby benefiting radiculopathy; however, no consensus has been reached among clinicians or researchers in this area.
~In a 2008 review investigating the use of lumbar traction for patients with chronic low back pain, Gay and Brault found only 10 randomized, controlled trials addressing this treatment. As a group, the studies contained more evidence against the use of traction than they did for it. The authors broke the information into subcategories based on whether the data covered patients with back and lower limb pain or with low back pain alone. They also looked at sustained and intermittent traction in these patient groups.
~The results indicated a lack of benefit in the use of sustained traction for chronic low back pain, with or
without lower limb symptoms. Motorized, intermittent traction, which has been aggressively marketed
(eg, VAX-D, DRX9000), likewise did not seem to differ in efficacy from simple intermittent axial traction.
Contraindications to Traction:
~No scientific reports clearly delineate contraindications for traction. The practitioner must rely on empirical information and opinion.
~Old age has been cited as a relative contraindication.
~Most practitioners agree that contraindications to cervical or lumbar traction include, but may not be limited to, the following:
1. Ligamentous instability
2. Osteomyelitis
3. Diskitis
4. Primary or metastatic tumor
5. Spinal cord tumor
6. Severe osteoporosis
7. Clinical signs of myelopathy
8. Severe anxiety
9. Untreated hypertension
~In the cervical spine, the practitioner also must take into account the fact that patients with vertebral basilar artery insufficiency may be more susceptible to cerebrovascular complications. Furthermore, patients with advanced rheumatoid arthritis or connective tissue disorders may be at risk for atlantoaxial instability.
Relative Contraindications:
1. Midline herniated nucleus pulposus
2. Acute torticollis
3. Restrictive lung disease
4. Active peptic ulcer
5. Hernia
6. Aortic aneurysm
7. Pregnancy.
REFERRAL CONSIDERATIONS
~The Physiotherapist who refers patients for traction must write a detailed and specific prescription that includes at least the following patient information:
~ Age
~Sex
~Diagnosis
~Underlying medical conditions
~Precautions needed
~Recommended follow-up.
~Traction should not be a single treatment approach but rather should be 1 part of a comprehensive rehabilitation treatment program. The most effective use of traction is likely to improve the patient’s activity level, mobility, and overall function.
Specific items to outline in traction referrals also should include the following information:
~Position (of the body, neck, or hip and knee)
~Mode of application (continuous or intermittent)
~Weight to be applied
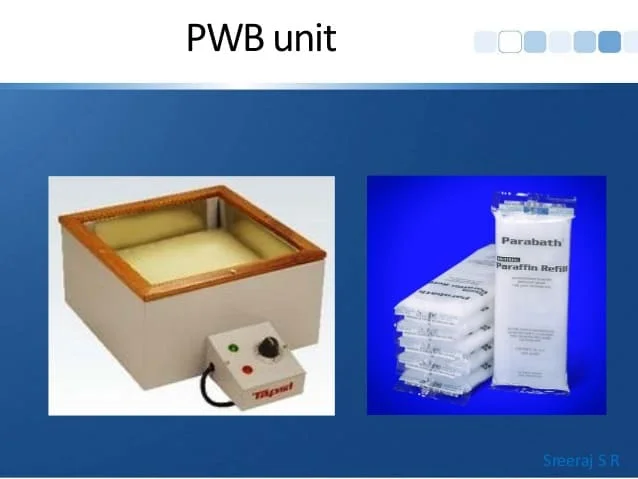
~Concurrent modalities (eg, heat)
~Frequency and duration of treatment
~Reevaluation guidelines and time frames
Spinal Traction:
~Spinal traction is a form of decompression therapy that relieves pressure on the spine. It can be performed manually or mechanically. Spinal traction is used to treat herniated discs, sciatica, degenerative disc disease pinched nerves, and many other back conditions.

What does spinal traction do?
~Spinal traction stretches the spine to take pressure off compressed discs. This straightens the spine and improves the body’s ability to heal itself.
Different types of lumbar traction have been described:

~First of all there is mechanical traction, using a mechanical device and a specially designed table that is
divided into two sections.
[1] The device delivers a certain tension to perform the traction. The patient wears
a harness, which consists of two rings, to support the patient.
[2] Autotraction also utilizes a table divided into two sections, the patient provides the traction force by pulling with the arms and/or pushing with the feet.
[3] Finally, there is manual traction performed by the therapist, pulling at the patient his ankles. Another way of manual traction is with the patient his legs over the therapist his shoulders, the therapist will place his arms on the patient’s thighs and pull.
[4] Continuous traction is applied for several hours with the use of a small amount of weight. Sustained traction has a shorter duration but a larger tension force.
[5] Intermittent traction is similar to sustained traction but alternately applies and releases the traction force at certain intervals.
Clinically Relevant Anatomy:
~The lumbar spine amounts to 5 moveable vertebrae numbered L1-L5. This complex anatomy is a considerable combination of these strong vertebrae, multiple bony components linked by joint capsules, ligaments/tendons, muscles, and highly sensitive nerves. The upper body weight is distributed to the lower extremities by way of the sacrum and pelvis. This reduces the amount of work required by spinal muscles.
~To achieve these functions:, the lumbar spine must consist of:
Resistance:
~Kyphotic and lordotic sagittal plane curves
~Increased mass of each vertebra from C1 to the sacrum And Elasticity:
~Lordotic and kyphotic curves
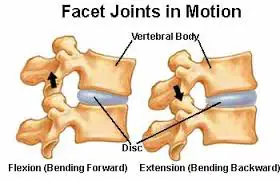
~Motion segments (or functional unit): composed of two adjoining vertebrae, intervertebral disc, ligaments, two
facet joints and capsules
~Structure of the lumbar vertebrae:
Ligaments:
~Anterior longitudinal ligament (ALL): from C2 to the sacrum
~Costal ligaments: connect the heads of the ribs to the vertebrae
~Intertransverse ligaments: inferior surface to the superior surface
~Posterior longitudinal ligament (PLL): from C2 caudally to the sacrum
~Interspinous
~Ligamentum flavum
~Intervertebral disks
~Facet joints
~Spinal cord/nerve roots
~Vertebral arch
~Cauda equina
Epidemiology /Etiology:
(1) Low Back Pain:
~ Low back pain (LBP) poses a significant problem to society.
~ Low back pain is the world’s number one cause of disability and one of the most prevalent health conditions.
~ Most patients also report radicular syndromes. Specific low back pain represents only 15% of all back pain problems, and 50% of specific back pain is due to a prolapsed intervertebral disc (PID), in which the nucleus pulposus herniates through a tear in the annulus fibrosus, resulting in irritation of the adjacent nerve root and causing a typical radiculopathy pain. Generally, pain that lasts less than 4 weeks is classified as acute pain.
~ The main clinical phenomena in acute LBP are pain and neurological disorders that affect daily activities.
~ Lumbar disc herniation: Disc degeneration might be caused by several conditions. A considerable proportion of patients with lumbar disc herniation remains symptomatic even after undergoing conservative treatments.
~ Lumbago – Sciatica: Epidemiological studies have shown that the rate of persistent sciatica is 1.6% in a given population while this rate increases to 25% with aging up to 64 years.
Mechanism of Action:
~Several theories have been proposed to explain the possible clinical benefit of traction therapy. Distracting the motion segment is thought to change the position of the nucleus pulposus relative to the posterior annulus fibrosis or change the disc-nerve interface. These effects are plausible based on studies examining the kinematics of the lumbar spine during traction therapies.
In addition to separating the vertebrae, traction has been shown to reduce nucleus pulposus pressure and increase foraminal area. However, it is unlikely that mechanical changes observed in a prone position will be sustained after a patient resumes an upright, weight-bearing posture. Any lasting clinical response to traction therapy would more likely be because of the effect of traction on the mechanobiology of the motion segment or neural tissues.
~Complicating the issue further is that not all traction therapies exert the same force on the spine and animal studies have found the mechanobiology of the disc to be sensitive to the amount, frequency, and duration of loading. It is possible that some forms of traction stimulate disc or joint repair whereas others promote tissue degradation.
~Although these variables have not been systematically examined, even in animal models, what is known regarding disc mechanobiology should alert us to the possibility that not all traction therapies are equal. If distracting the spine can influence disc and joint mechanobiology, different modes of traction may result in different clinical results. Systematic reviews of lumbar traction therapy have typically not considered that different effects may exist based on force and time parameters
~Traction trials have most often included patients with a mix of clinical presentations including back-dominant low back pain (LBP), leg-dominant LBP, or both. However, a patient with only dominant LBP and no radiculopathy is likely experiencing pain from a sclerotomal source, such as facet joints or disc, whereas sciatic pain, even if caused by disc herniation, may be predominately of neural origin. Although it is reasonable to suspect that traction therapies may affect these conditions differently, there is insufficient evidence to support this hypothesis. Distraction manipulation and positional distraction are mechanically different than traditional traction (intermittent or sustained). Rather than allowing forces to be dispersed throughout the lumbar tissues, these treatments attempt to concentrate them in a smaller area.
~AT, for example, allows the patient to concentrate the force by finding the position that most relieves their pain and applying distraction in that position. Distraction manipulation, most often used by chiropractors and physical therapists, is performed on treatment tables that allow the operator to determine the moment-to-moment vector and timing of the distractive force. These techniques include FD (Cox technique), Leander technique, and Saunders Active Trac method, among others.
Differential Diagnosis:
~In an effort to maximize conservative treatment in a population with higher rates of progression to costly interventions, such as surgery and injections, a trial of traction could be considered for patients who have a preference for this treatment or who are unresponsive to other physical therapy interventions. Summary evidence in recent systematic reviews and clinical practice guidelines concludes that mechanical lumbar traction is not effective for treating acute or chronic nonspecific low back pain (LBP).
~However, many physical therapists continue to use it, primarily as an additional modality. Indeed, expert clinical opinion, theoretical models, and some research evidence suggest that certain patients with LBP respond positively to traction. A study published in the March 2016 issue of JOSPT investigates the effectiveness of traction in prone as an adjunct to an extension-oriented exercise program in patients with LBP and leg pain and explores whether a previously identified set of patient characteristics is associated with better outcomes from traction.
~Low back pain – Either alone or in combination with other treatments, traction has little or no impact on pain intensity, functional status, global improvement and return to work among people with low back pain.
~Lumbar disc herniation – Herniated lumbar disks are the central cause of sciatica. Cohort studies suggest that the condition of many patients with a herniated lumbar disk improves in 6 weeks. In other words, conservative therapy is generally recommended for 6 weeks in the absence of a major neurologic deficit. There is no proof that conservative treatments change the natural history but some offer slight relief of symptoms. A few examples are NSAIDs (= reduce back pain, but they have a less clear benefit in patients with sciatica). A meta-analysis of 32 randomized trials showed no significant benefit of lumbar traction.
~Sciatica – Traction and exercise therapy were significantly inferior to surgery.
How much % of the body weight must be used?
~In deciding what traction weight to apply, one must consider 2 aspects:
~what weight will overcome the friction between the body and the bed; and
~what amount of force is required to exert an effect on the lumbar spine. Judovich showed that a traction force of 26% of the patient’s body weight was required to overcome friction. The use of a split tabletop with friction
-free rollers reduce this to a negligible amount. In its absence, a force in excess of 26% of the body weight must be used before any effect can be produced at the lumbar spine.
~Optimal weights for traction have been investigated by assuming that intervertebral widening or reduction of disk protrusion achieves the effect of traction; however, only the former has been demonstrated experimentally.
~Despite the studies, it remains unclear what magnitude of force is required to cause the desired effect in the intact human spine.
The mechanism by which traction may have its effects is not fully understood, and the neuromodulation of pain, which may require very low weight, must also be considered as a possible effect.
~This notwithstanding, clinical experts recommend using motorized traction on a friction-free surface and advocate a wide range of traction weights within their treatment regimes. Maitland suggests 10 to 65kg, with an average of 30 to 45kg; Cyriax suggests 40 to 85kg; Grieve suggests 13 to 34kg; and Hicklings suggests 32 to 68kg.
Placebo comparison:
~From a systematic review six studies compared traction with sham traction. Sham traction is a low-weight or placebo traction that the given researcher considers to be ineffective. Three studies used motorized traction (2 on a split tabletop, 1 on a plain tabletop)), 1 used autotraction, 1 used gravitational traction, and 1 used traction as part of bedrest. Only the study by Beurskens et al was of high quality, and all gave negative results except for the inconclusive result of Moret et al.
Conclusion:
~Lumbar traction is used by physiotherapists for threatening patients with lower back pain and leg pain. There are different types of lumbar traction: mechanical traction, auto traction, and manual traction. There had been shown that lumbar traction reduces nucleus pulposus pressure. Lumbar traction can be used in many disorders of the lower back: lumbar disc herniation, low back pain, and lumbago-sciatica. A few clinical trials still questioned the effectiveness of lumbar traction.
Risks of spinal traction:
~There are no long-term risks of spinal traction. Some side effects may occur during or after treatment. Many people experience muscle spasms after traction. Some have pain in the treated areas.
~Spinal traction is not for everyone. A physician can determine if the risks are worth the potential rewards based on your medical history.
Spinal traction can have several effects. For instance, traction can help:
~Decrease compression forces and help distract vertebral bodies. It can help mobilize the facet joints in the spine. This can also increase the (intervertebral) space where the spinal nerves exit out of the spine and help
~decrease irritation of these nerves.
~Enhance nourishment of the disc and nerve
~Decrease muscle spasm
~Stretch the muscles and connective tissues along the spine
~Increase circulation
~Decrease the sensitivity and pain in the joints of the spine
~Spinal elongation and the flattening of curvature in the spin
~Some conditions in the spine that it may help with include:
~Nerve pain and weakness down the arm and legs from disc and nerve injuries; radiculopathies
~Advanced degenerative changes in the spine, stenosis
~Biomechanical joint stiffness in the spine
~It is important to be carefully assessed by your physiotherapist to determine how appropriate spinal traction is in your case. This is dependent on your signs and symptoms, the acuity of your injury and stage of healing, your past and current medical history, and your response to previous treatment. When carefully and appropriately selected by you and your physiotherapist, spinal traction is an effective treatment choice.
How is spinal traction administered?
Spinal traction therapy can be administered manually or mechanically, depending on your needs.
(1)Manual spinal traction:
In manual spinal traction, a physical therapist uses their hands to put people in a state of traction.
Then they use manual force on the joints and muscles to widen the spaces between vertebrae.
(2)Mechanical spinal traction:
In mechanical spinal traction, you will lie on a table that has special tools to stretch the spine.
A physical therapist will attach a series of ropes, slings, and pulleys to your body to mechanically relieve pressure.
Precautions when you applying spinal Traction
~Joint hypermobility
~Acute inflammation
~Claustrophobia or anxiety associated with traction
~Cardiac or respiratory insufficiency (lumbar and inversion traction); cervical traction risk for internal jugular
thrombosis; BP fluctuations
~Pregnancy (increased ligamentous laxity and risk for abdominal compression)
~Symptoms increase with traction; hx of aggravation with traction
~TMJ dysfunction (cervical) if using a chin strap
Indication of Spinal Traction:
Following list of spinal condition where spinal traction is most used to relieve referred pain.
- Spinal nerve root impingement:
- Herniated disc (Slip Disc)
- Ligament encroachment
- Narrowing of the intervertebral foramen
- Osteophyte encroachment
- Spinal nerve root swelling
- Joint hypo mobility
- Spondylolisthesis
- Degenerative joint disease
- Extrinsic muscle spasm and muscle guarding
- Discogenic pain
- Joint pain
- Compression fracture
- Lumbar disc disorders of primary origin
Contraindication:
- Acute strains
- Sprains
- Inflammation
- Respiratory problem
- Claustrophobia
- Osteoporosis
- Infection
- Tumor
- Rheumatoid arthritis
- Pregnancy
- Cardiovascular disease
- Hernia
- Cauda Equina Syndrome
- Neoplasms
- Pott’s Disease and all inflammatory diseases of the vertebrae
- Cardiac or circulatory disease and severe respiratory problems
- Post-operative patients within 3 months of back surgery
FAQs
The use of traction in physiotherapy is to relieve pain, improve joint mobility, and promote healing in musculoskeletal conditions by applying controlled force to the affected area.
Intermittent traction is typically the preferred treatment option for degenerative disc degeneration and/or joint hypomobility. On the other hand, persistent traction is most frequently utilized for neck pain caused by disc herniations, muscles, or soft tissues.
Different types of traction in physiotherapy include manual traction, mechanical traction, and positional traction, each aimed at relieving pain and promoting joint mobility through controlled force application.
Benefits of Traction
Start rehydrating, then raise the disc height.
Strengthen the disc, the ligaments, and the tendons.
Assists in protecting against harm.
Helps wounded tissues heal faster and makes injured joints better.
Increase nutrition and lubrication of the spinal joints.
Traction side effects include cauda equina syndrome, fracture, lumbar disc protrusion development, shortness of breath, hypertension, and elevated blood pressure (gravity traction).