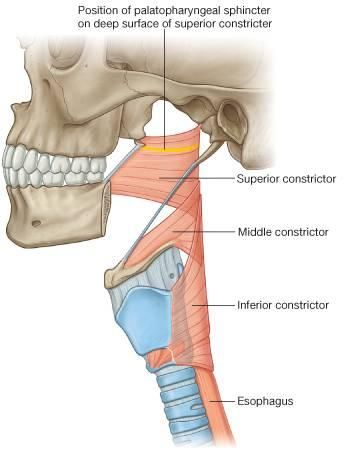
Inferior Pharyngeal Constrictor Muscle
Inferior Pharyngeal Constrictor Muscle Anatomy
The Inferior pharyngeal constrictor, the thickest of all three constrictors, arises from the sides of the cricoid and thyroid cartilage. Similar to the superior and middle pharyngeal constrictor muscles, This Muscle Nerve supply is the vagus nerve (cranial nerve X), specifically, by branches from the pharyngeal plexus and by neuronal branches from the recurrent laryngeal nerve.
the thickest of the three constrictors arises from the sides of the cricoid and thyroid cartilage.
Origin:
cricoid and thyroid cartilage.
Insertion:
pharyngeal raphe.
Blood Supply
ascending pharyngeal artery, a branch of the external carotid artery.
Nerve supply
the external laryngeal branch of the vagus.
pharyngeal plexus; cricopharyngeus part can also receive innervation from the recurrent laryngeal nerve and/or the external laryngeal nerve.
Action
Swallowing
As soon as the bolus of food is received in the pharynx, the elevator muscles relax, the pharynx descends, and the constrictors contract upon the bolus and convey it down into the esophagus. During deglutition, they contract and cause peristaltic movement in the pharynx.
Breathing
When speaking and breathing, the inferior pharyngeal constrictor muscle is partially engaged. Maintaining an open pharynx is beneficial, especially when you’re sleeping.
Structure
There are two components to the inferior pharyngeal constrictor muscle. The thyroid cartilage (thyropharyngeal portion) gives rise to the first and more superior component, whereas the cricoid cartilage (cricopharyngeal part) gives rise to the second part.
It originates on the thyroid cartilage from the inferior horn of the thyroid cartilage, the oblique line on the side of the lamina, and the surface behind this almost all the way to the posterior boundary.
It emerges from the cricoid cartilage in the space between the articular facet of the thyroid cartilage’s inferior horn behind and the cricothyroid muscle in front.
From these points of origin, the fibers extend medially and rearward to join the opposing side’s muscle at the fibrous pharyngeal raphe, which is located in the pharynx’s posterior median line. Anaerobic type 2 fibers are primarily used in the thyropharyngeal portion, whereas aerobic type 1 fibers are primarily used in the cricopharyngeal portion. Following birth, fiber type may alter.
The inferior fibers are horizontal and continuous with the circular fibers of the esophagus; the remainder rise, increasing in obliquity, and overlap the middle pharyngeal constrictor muscle. The cricopharyngeal portion is synonymous with the upper esophageal sphincter (UES), which controls the opening of the cervical esophagus. It is also known as the cricopharyngeal inlet.
Anatomical Variation
The posterior portion of the pharyngobasilar fascia or the superior pharyngeal constrictor muscle may combine with the inferior pharyngeal constrictor muscle.
Pathology Related to This Muscle:

Uncoordinated contraction,//cricopharyngeal spasm, and/or impaired relaxation of this muscle are currently considered the main factors in the development of a Zenker’s diverticulum. Zenker’s diverticulum develops between the two bellies of the inferior constrictor (Thyropharyngeal and Cricopharyngeal) in a small gap called Killian’s dehiscence.
A diverticulum can form where a balloon of mucosa becomes trapped outside the pharyngeal boundaries. Food or other materials may reside here, which may lead to infection.
Motor incoordination of the cricopharyngeus can cause difficulty swallowing.
Radiological damage
Chemotherapy combined with intensity-modulated radiation therapy may cause injury to the inferior pharyngeal constrictor muscle. Dysphagia could result from this, necessitating the continuous use of a feeding tube in place of autonomous swallowing.