Dysphagia (Difficulty Swallowing)
Table of Contents
What is dysphagia?
Dysphagia can be done due to difficulty anywhere in the swallowing process. Dysphagia is more seen in older adults.
A typical “swallow” involves several various muscles and nerves; it has an unusually complex process trusted Source.
There are three general types of dysphagia
Oral dysphagia (high dysphagia): difficulty in the mouth, ocassinaly caused by tongue weakness after a stroke, a problem in chewing food, or difficulty in transporting food from the mouth.
Pharyngeal dysphagia: the difficulty is in the throat. Issues in the throat are often due to a neurological problem that affects the nerves (like Parkinson’s disease, stroke, or amyotrophic lateral sclerosis).
Esophageal dysphagia (low dysphagia): the problem is creat in the esophagus. This has usually because of a blockage or irritation. Often, a surgical procedure has required.It is noteworthy that pain while swallowing (odynophagia) varies from dysphagia, but it has possible to have both at the same time. And, Globus has the sensation of something being inserted in the throat.
Causes of dysphagia
Possible causes of dysphagia include:
Amyotrophic lateral sclerosis — an incurable form of progressive neurodegeneration; after a long time, the nerves in the spine and brain continuously lose function.
Achalasia — lower esophageal muscle does not relax sufficiently to allow food into the stomach.
Diffuse spasm — the muscles in the esophagus in a compact awkward way.
Stroke — brain cell death leads to a lack of oxygen because blood flow is deceased. If the brain cells that control swallowing are infected, it can lead to dysphagia.
Esophageal ring — a small part of the esophagus narrows, stopping solid foods from passing through sometimes.
Eosinophilic esophagitis — severely raised levels of eosinophils (a type of white blood cell) in the esophagus. These eosinophils lengthen in an uncontrolled way and attack the gastrointestinal system, leading to vomiting and difficulty with swallowing food.
Multiple sclerosis — the central nervous system is attacked by the immune system, blasting myelin, which normally protects the nerves.
Myasthenia gravis (Goldflam disease) — the muscles under voluntary control become easily tired and weak because there is difficulty with how the nerves stimulate the contraction of muscles. This is known as an autoimmune disorder.
Parkinson’s disease and Parkinsonism syndromes — Parkinson’s disease is a gradually continuing degenerative neurological disorder that damages the patient’s motor skills.
Radiation — some patients which can receive radiation therapy (radiotherapy) to the neck and head part may have swallowing problems.
Cleft lip and palate — types of abnormal developments of the face lead to the incomplete fusing of bones in the head, resulting in gaps (clefts) in the palate and lip-to-nose part.
Scleroderma — a group of rare autoimmune diseases that the skin and connective tissues enhance tighter and harden.
Esophageal cancer — a type of cancer in the esophagus, usually leads to either alcohol and smoking, or gastroesophageal reflux disease (GERD).
Esophageal stricture — the reduced size of the esophagus, often leads to GERD.
Xerostomia (dry mouth) — there is faulty saliva to keep the mouth wet.
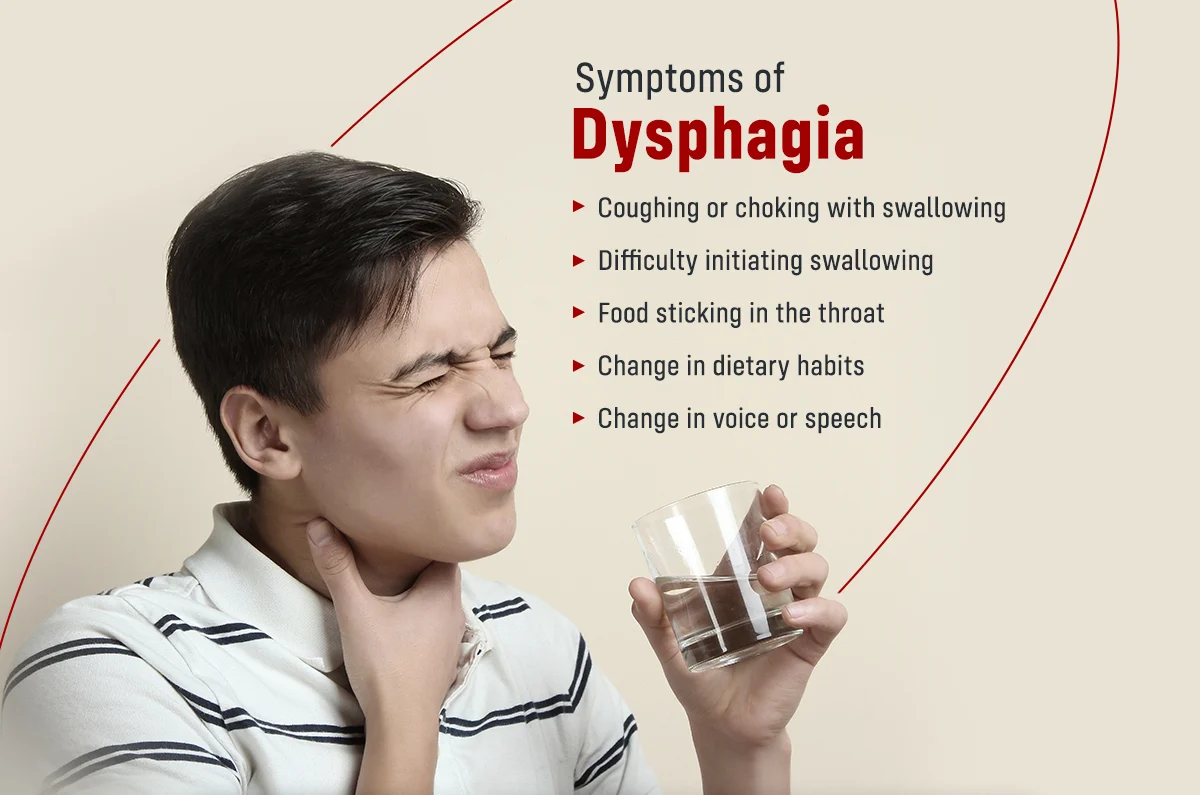
Symptoms of dysphagia
Coughing while swallowing can be a symptom of dysphagia.
Some patients have dysphagia and are unknowing of it — in these cases, it may not go diagnosed and not be treated, increasing
the risk of desire pneumonia (a lung infection that can develop after accidentally inhaling saliva or food particles).
Undiagnosed dysphagia may also cause dehydration and malnutrition.
Symptoms linked to dysphagia include:
- Choking when eating.
- Coughing or gagging when swallowing.
- Drooling.
- Food or stomach acid reverses into the throat.
- Recurrent heartburn.
- Hoarseness.
- The sensation of food getting stuck in the throat or chest, or behind the breastbone.
- Unexplained weight loss.
- Bringing food back up (regurgitation).
- Difficulty controlling food in the mouth.
- Difficulty starting the swallowing process.
- Recurrent pneumonia.
- Inability to control saliva in the mouth.
- Patients may feel such“the food can get stuck.”
Risk factors for dysphagia
The risk factors of dysphagia include:
Aging — older people are more at risk. This leads to general wear and tear on the body for a long time Also, certain diseases of old age can lead to dysphagia, like Parkinson’s disease.
Neurological conditions — certain nervous system disorders make dysphagia likely.
Complications of dysphagia
Pneumonia and upper respiratory infections – specifically aspiration pneumonia, can be done if something is swallowed down the “wrong way” and enters the lungs.
Malnutrition — this is especially the case with people who are less aware of their dysphagia and are not being treated for it. They may simply not be getting too many vital nutrients for good health.
Dehydration — if an individual cannot drink regularly, their fluid intake may not be enough, cause to dehydration (shortage of water in the body).
Diagnosis of dysphagia
A speech-language pathologist will try to determine where the difficulty lies – that is a part of the swallowing process is causing the problem. The patient will be asked about symptoms, how long they have been present, and whether the problem is with liquids, solids, or both.
Swallow study — this is likely administered by a speech therapist. They test various consistencies of food and liquid to see which leads to difficulty. They may also do a video swallow test to show where the problem is
Barium swallow test — the patient consumes a barium-containing liquid. Barium appears in X-rays and helps the doctor identify what is happening in the esophagus in more detail, especially the activity of the muscles.
Endoscopy — a doctor uses a camera to refuse into the esophagus. They can bring a biopsy if they find something they think might be cancer.
Manometry — this study measures pressure changes produced when muscles in the esophagus are working which be used if nothing is found during an endoscopy.
Treatment for dysphagia
Treatment depends on the type of dysphagia:
Treatment for oropharyngeal dysphagia (high dysphagia)
Because oropharyngeal dysphagia is frequently a neurological problem, providing effective treatment is challenging. Patients with Parkinson’s disease can respond well to Parkinson’s disease medication.
Swallowing therapy — this can be done by a speech and language therapist. The individual will learn a new manner of swallowing properly. Exercise can help increase e the muscles and how they respond.
Diet — Some foods and liquids, or combinations of them, are not hard to swallow. When you are eating the easiest-to-swallow foods, it has also needy that the patient has a maintained diet.
Feeding through a tube — if the patient has at risk of pneumonia, malnutrition, or dehydration they may need to be fed through a nasal tube (nasogastric tube) or PEG (percutaneous endoscopic gastrostomy). PEG tubes are surgically implanted directly into the stomach and pass in a small incision in the abdomen.
Treatment for esophageal dysphagia (low dysphagia)
Surgical intervention is such that requires for esophageal dysphagia.
Dilation — of the esophagus tries to be widened ( leads to a stricture, for example), a small balloon may be inserted and then inflated (it is then removed).
Botulinum toxin (Botox) — mostly used if the muscles in the esophagus can be stiff (achalasia). it has a strong toxin that can paralyze stiff muscles, reducing constriction.
Physiotherapy management:
Rehabilitative exercises changes and improves the swallowing physiology in force, speed, or timing, with the mission being to produce a long-term effect, compared to compensatory interventions used for a short-time effect.
Rehabilitative exercises also take part in retraining the neuromuscular systems to bring about neuroplasticity, still pushing any muscular system in an intense and persistent manner will bring about changes in neural innervation and patterns of movement. Rehabilitation exercise can be widely divided into :
- Swallowing exercises
- Non-swallowing exercises
Swallowing Exercises
Swallowing exercises also are used to treat dysphagia with the goal of altering swallowing physiology and promoting long-time changes. Exercises are expected to affect swallowing mechanics and impact bolus flow. forcefully swallow, Mendelsohn, super-supraglottic, and Masako have some of the swallowing exercises. Swallowing exercises do many of the neuroplasticity principles as:
- Use it or lose it
- Use it and improve it
- Specificity
- Transference
- Intensity
Non-Swallowing Exercises
Non-swallowing exercises those such don’t involve the act of swallowing, like tongue strengthening exercises. Non-swallowing exercises can be done by patients he/she can’t eat orally (are tube-fed) or those after surgery who are temporarily restricted to eating orally. Shaker head lift, tongue strengthening, Lee Silverman voice treatment, and expiratory muscle strength training have some of the non-swallowing exercises. Non-swallowing exercises do a few neuroplasticity principles and they are:
- Transference
- Intensity
- Therapeutic Interventions
- Therapeutic techniques are divided into those used:
Compensatory strategies like patient do Head Rotation (Head Turn), Chin Tuck (Head Flexion and Head Tilt, and Bolus Viscosity, Texture, and Volume Modifications)
Exercises (Tongue Hold, Shaker Exercise)
Those used two compensatory strategies or exercises like Supraglottic Swallow, Super-Supraglottic Swallow, Effortful Swallow, Mendelsohn Maneuver
Another method (Neuromuscular Electrical Stimulation (NMES), Oral Stimulation, and Other Interventions )
Head Rotation (Head Turn)
The head rotation has a compensatory strategy used for patients with unilateral pharyngeal and/or laryngeal weakness like decreased UES opening.
Instruction: When the patient is swallowing food, turn your head to the affected side as if you are looking over your shoulder.
Physiological advantages:
It redirects the bolus to the side of the pharynx odds the rotation (the stronger side)
It increases the duration of UES opening.
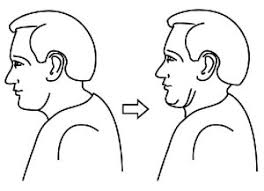
Chin Tuck (Head Flexion)
The chin tuck (head flexion) can be used for patients, those patients have reduced airway protection associated with late swallow initiation and/or reduced tongue base retraction.
Instruction: While the patient is swallowing food & bring your chin towards the chest and maintain this posture throughout the periods of the swallow.
Physiological benefits:
Expansion of vallecular recesses
Approximation of tongue base toward pharyngeal wall
Reduction in distance between hyoid and larynx
Increases timing of swallowing apnea during the swallow
Head Tilt
The head tilt can be used for patients who have a unilateral oral weakness.
Instruction: While the patient is swallowing then the patient tilts her head like you have to try to touch her ear to her shoulder. Swallow maintaining this position for some time.
Physiological benefits:
It directs the bolus at the stronger side of the oral cavity
Bolus Viscosity, Texture, and Volume Modifications
Increasing the volume & viscosity of liquids has an alternate technique used for patients who have problems in oral control of thin liquids and/or demonstrate reduced airway protection. Some patients may benefit from texture-modified foods.
Supraglottic Swallow
The supraglottic swallow can be used for patients who demonstrate decreased airway protection while the swallow and delayed swallow initiation.
Instruction: Before swallowing, first, inhale deeply then hold your breath, continue to hold your breath, and swallow immediately after you swallow (before you inhale), cough then at that time swallow again.
physiologic benefits :
Increases airway closure and
Increases UES opening during the swallow
Super-Supraglottic Swallow
Super-supraglottic swallow varies from supraglottic swallow only when implementing effortful breath hold
Instruction: Before swallowing, take a deep breath and hold it tightly when the patient bearing down; continue to hold your breath and bear down as you swallow; immediately after your swallow like before you inhale the cough then at that time swallow hard again (before you inhale).’’
Physiological advantages:
The patient can earlier tongue base movement
Higher hyoid position at swallow onset
Increased hyoid movement like longer bolus transit time
Note: Both the supraglottic swallow and the supra-supraglottic swallow maneuvers can result in Valsalva and may result in arrhythmia in stroke patients during treatment periods. since therapists should be mindful of using this technique in stroke patients, especially in those with coexisting heart disease.
Effortful Swallow
The effortful swallow can be used for patients who present with clinically significant took parts in the valleculae and/or pyriform sinuses as well as for patients who may be reduced airway closure.
Instructions: when the patient is wallowing, squeeze your throat muscles as hard as you can.
Physiological advantages:
It improves hyolaryngeal excursion, duration of hyoid elevation
Increases UES opening
Increases laryngeal closure
Increases lingual pressures
Increases peristaltic amplitudes in the distal esophagus
Increases pressure and period of tongue base retraction
Mendelsohn Maneuver
This technique can be used for patients who had decreased hyolaryngeal excursion and/or decreased duration of UES opening.
Before giving the command, the patient can be suggested first to feel laryngeal elevation through palpation while swallowing the saliva.
Instruction: After palpating the thyroid cartilage, feel the cartilage elevation while the patient is swallowing, now hold for several seconds and swallow the food while holding it up.
Physiologic benefits:
It increases the time and duration of the hyolaryngeal excursion
Increased duration of UES opening, pharyngeal peak contractions,
Increased bolus transit duration& time, and pressure of tongue base contact.
Tongue Hold
The tongue hold is used for decreased tongue base and pharyngeal wall contact.
Instruction: When the patient is swallowing the food, hold the anterior tongue (slightly posterior to the tongue tip) between the teeth.
Physiological benefits: It can improve anterior bulging of the posterior pharyngeal wall.
Shaker Exercise
The Shaker Exercise is used for patients while decreasing UES opening and weakness of the suprahyoid muscles.
Instruction: The patient’s position is supine and the patient is asked to complete 3 head lifts sustained till 1 min each; 1 min rest period between each head lift; then complete 30 sets head lifts holding for 2 s each’’ The suggested frequency has three times each day for 6 consecutive weeks.
Physiological benefits:
It increases anterior hyolaryngeal excursion
It increases UES opening
It strengthens suprahyoid muscles
It increased thyrohyoid shortening.
Masako
In this technique, the patient is asked to protrude the tongue and hold it between the teeth when the patient is swallowing.
FAQs
- What are the three signs of dysphagia?
Signs and symptoms related to dysphagia can include Pain when the patient is swallowing. Inability to swallow. A sensation of food tackle in the throat or chest or behind the breastbone (sternum)
2. Who usually gets dysphagia?
Dysphagia has many possible reasons and happens most frequently in older adults. Any condition that weakens or damages the muscles and nerves used for swallowing may lead to dysphagia. For example, people with diseases of the nervous system, like cerebral palsy or Parkinson’s disease, often have difficulty in swallowing.
3. Does drinking water help with dysphagia?
Maintain Hydration
It has easy for elderly adults to become dehydrated when they suffer from dysphagia. If they can’t drink normal water, they must not drink anything at all
4. What is end-stage dysphagia?
Swallowing difficulties are common at the end of life and dysphagia & refer them to a speech pathologist for a swallowing assessment and guidance for appropriate interventions
5. Can dysphagia be cured with medication?
Depending on the cause, it can be possible to treat oesophageal dysphagia with medication. like, proton pump inhibitors (PPIs )can be used to treat indigestion and may improve symptoms that lead to narrowing or scarring of the esophagus.





5 Comments