Inferior Rectus Muscle
Table of Contents
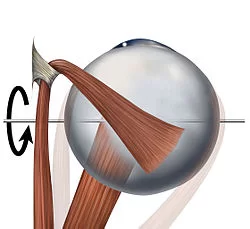
Inferior rectus muscle Anatomy
- Inferior rectus muscle is one of the 4 straight muscles of the orbit and it is responsible for the movement of the eye on the downward side.
- The inferior rectus muscle originates from the common tendinous ring and goes on to attach at the lower anterior surface of the eyeball.
- This muscle are supplied by the oculomotor nerve if trauma affecting this nerve impacts the movement of the inferior rectus muscle.
Origin
- The inferior rectus muscle originates from the common tendinous ring, also called the annulus of Zinn, that is found in the posterior pole of the orbit encircling the margins of the optic canal.
Insertion
- Inferior rectus muscle insertion by the Anterior half of the eyeball (posterior to corneoscleral junction)
Nerve supply
- Inferior rectus muscle supply by the inferior branch of the oculomotor nerve.
Blood supply:
- The inferior muscle rectus is principally supplied by the inferior muscular artery (4 pedicles) and the lateral muscle is supplied by the lacrimal artery or the lateral muscular artery (3 to 6 branches).
Venous Drainage
Venous drainage discharges into the superior and inferior orbital veins, functioning similarly to the artery system. The superior and inferior rectus muscles’ lateral and medial sides are home to the four vortex veins that are typically present. The orbital venous system receives the drain from these vortex veins.
Actions:
- Inferior rectus produces three simultaneous actions:
= Depresses the anterior pole of the eyeball
= Adducts the eyeball medially
= Externally rotates the eyeball
Relations:
- The inferior rectus muscle arises from the inferior part of the common tendinous ring and attachments of the medial, lateral, and superior recti muscles.
- The common tendinous ring encircles the superior, medial, and inferior margins of the optic canal and part of the superior orbital fissure.
- The inferior rectus muscle passes along the floor of the orbit superior to the infraorbital canal, which is supplied by infraorbital artery and inserted onto the anteromedial part of the sclera, the inferior rectus muscle is covered by the inferior oblique muscle.
Assessment
During the clinical examination, the inferior rectus muscle’s function can be evaluated in addition to that of the other extraocular muscles. The patient can be asked to stare in nine different directions to gauge the movement of the extraocular muscles. The main gaze comes first, then the secondary positions (up, down, left, and right), and finally the tertiary positions (up and left, up and left, down and right, down and left). By having the patient follow their finger as it traces a broad “H” in the air, the doctor may test these postures.
Additional ocular alignment testing can be carried out using a variety of techniques, such as different target, corneal light reflex, cover, and dissimilar image tests. Since many patients with extraocular muscle anomalies are young children, the doctor may need to use creative testing methods, such as getting the kid to cooperate by utilizing toys or other things.
Embryology
The primary source of mesoderm and neural crest cells is the mesenchyme of the head, which includes the orbit and associated components. While the satellite and connective tissue of the muscles are derived from neural crest cells, the extraocular muscles are derived from the mesoderm. Neural crest cells also provide the majority of the orbit’s residual connective tissue.
Physiologic Variantions
Individual differences can be observed in the size of the inferior rectus muscle, the location of its insertion on the globe from the limbus, and other anatomical parameters.
Ocular misalignment may be caused by congenital variations in the extraocular muscles.
Clinical significance
Occlusive floor fractures may affect the inferior rectus because of its proximity to the orbital floor. Trauma to the inferior rectus muscle or nerve can cause inferior rectus muscular paresis. This can happen during orbital floor repair surgery or at the time of the initial damage.
When a patient has inferior rectus muscular paresis without entrapment, they may have primary position hypertropia. The patient may have a small deviation, or hypotropia, which diminishes with downgaze if paresis is associated with entrapment. Six months of observation is the first course of treatment for inferior rectus paresis. In the event that no progress is shown throughout this period, muscle surgery may be advised.
- If damage to the oculomotor nerve may cause a partial or complete paralysis of the extraocular muscles it supplies, as well as the levator palpebrae and sphincter pupillae muscles This condition is called the external oculomotor palsy.
- Complete palsy involves all the muscles innervated by the oculomotor nerve, whereas partial oculomotor palsy involves specific muscles.
- A muscle capsule found in the inferior rectus connects to the inferior oblique muscle capsule. The muscles that retract the lower eyelid are joined by a fibrous band called the Lockwood ligament.
Etiology:
- Aneurysms (especially of the posterior communicating artery).
- Transtentorial brain herniation.
- Ischemia of the 3rd cranial nerve (usually due to diabetes or hypertension) or of the midbrain
Occasionally, a posterior communicating artery aneurysm causes oculomotor palsy and spares the pupil.
Symptoms:
- Diplopia and ptosis (drooping of the upper eyelid).
- The affected eye turns slightly outward and downward when the unaffected eye looks straight ahead, causing double vision.
- The affected eye may turn inward very slowly and may move only to the middle when looking inward. It cannot move up and down.
Sign:
- Ptosis
- abduction of globe
- limitation of adductions
- limitation of elevation
- limitation of depression
Treatment:
- If the paralysis is at the acute stage (first 6 months), treatment must be conservative and include various therapeutic options.
- Observation.
- Eye occlusion (preferably alternately) to avoid double vision.
- Non-steroid anti-inflammatory drugs if it is painful.
After 6 months have passed from the start of the clinical picture, we talk about the chronic phase.
- If the deviation is small, prisms are incorporated into your glasses to prevent double vision.
- If the deviation is greater, the prism cannot be tolerated so surgical treatment is indicated.
FAQ
The eye is adducted and depressed by the inferior rectus. In the event that the inferior rectus becomes entrapped, patients frequently exhibit restricted upgaze and vertical gaze diplopia. The medial rectus runs parallel to the medial orbital wall and is derived from Zinn’s upper and lower tendons.
Oculomotor Nerve
The oculomotor nerve, which enters the muscle on its superior surface, is the inferior division of cranial nerve III and innervates the inferior rectus.
When compared to other muscles, the inferior rectus was found to have the lowest mean thickness of 3.177 ± 0.662 mm. Based on this, we can conclude that the mean values for the inferior, superior, lateral, and medial recti in our study were, respectively, 4.015 + 0.762 mm, 3.548 ± 0.369 mm, 3.757 ± 0.654 mm, and 0.1775 ± 0.6622 mm.
Orbit
A muscle in the orbit close to the eye is called the inferior rectus. Within the category of extraocular muscles, it is one of the four recti muscles. It inserts into the anteroinferior surface of the eye after emerging from the common tendinous ring. The eye is depressed (downwards) by it.
Congenital, traumatic, myasthenic, and vascular etiology was the cause. The presenting symptoms were diplopia, a disfiguring hypertropia, or an abnormal head position.
The inferior rectus muscle originates from the tendinous ring’s lower limb. Its insertion is situated roughly 6.5 mm from the limbus in an arc, with the nasal side being closer to the limbus. The tendon’s length is approximately 5.5 mm.