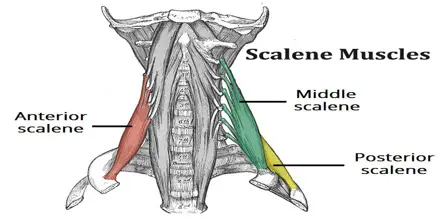
Scalene Muscles
Table of Contents
Introduction
Scalene Muscle is a group of three pairs of muscles in the lateral neck, namely the anterior scalene, middle scalene, and posterior scalene.
The cervical tract is laterally positioned and the scalene muscles are deep. Because the brachial plexus and the cervical plexus are involved in their function, their innervation is complex. Their functions are equally intricate and crucial, and they are multi-articular muscles. In addition to their function as accessory breathing muscles, they are crucial for head and neck mobility and posture maintenance. Numerous clinical patterns, including cervical discomfort, reduced ventilatory capacity, and thoracic outlet syndrome, are brought on by their malfunction.
Medical treatments aimed at reducing their tone and rehabilitation efforts aimed at enhancing their physiological length or contractile strength are frequently applied to them. We shall examine how to properly stretch the scalene muscles in this review, as well as how to manually differentiate between the sternocleidomastoid muscle and the latter.
Anatomy of Scalene Muscle
The scalene muscles are placed deep with respect to the sternocleidomastoid muscle, lateral to the cervical spine, linking the vertebrae to the first two ribs. Scalene muscles are covered by the prevertebral fascia, also known as deep fascia.
Anterior Scalene Muscle
The anterior tubercles of the transverse processes of the cervical vertebrae, which run from the third to the sixth vertebrae, are the source of the anterior scalene. It is put into the upper face of the first rib’s scalene muscle tubercle. The pleural dome may come into contact with a few anterior scalene fibers. The anterior and middle scalenes are crossed by the omohyoideus muscle.
The muscle is thinner at the origin and insertion levels and thicker at the cricoid cartilage level. Behind the subclavian vein, the phrenic nerve crosses and shares the muscle fascia from the lateral to the medial borders. The anterior and medial scalene muscles produce the gap (fissura scalenorum) for brachial plexus passage.
Middle Scalene Muscle
Originating from the transverse processes of the final six cervical vertebrae, the middle scalene inserts itself on the top face of the first rib, posterior to the subclavian artery sulcus, between the anterior and posterior tubercles. The upper part of the long thoracic nerve goes via the middle scalene, over the latter, or between the middle and posterior scalenes.
Posterior Scalene Muscle
The posterior tubercles of the transverse processes of the final three or four cervical vertebrae are the origin of the posterior scalene muscle. It fits on the second rib’s anterior face.
The fourth scalene, also known as the minimal scalene, affects the anterior tubercle of the transverse process of the seventh cervical vertebra and inserts itself on the first rib. It also covers the pleural dome posteriorly and is present in around 30% to 71% of the population. It is possible to confuse the transverse pleural ligament with the minimal scalene.
Origin
Cervical vertebrae (CII-CVII).
Insertion
First and second ribs.
Nerve Supply
Cervical nerves (C3-C8).
The anterior branches of the cervical spinal nerves, which run from C3 to C8, innervate the scalene muscles. The cervical and brachial plexuses are involved in the functions of the scalene muscles, and their cooperation is essential to their various roles. Although they are uncommon, there are variations in the neuroanatomy around the scalene.
Blood Supply and Lymphatics
Its pre-scalene region, which is the first segment of the subclavian artery, serves as its origin. The anterior scalene muscle area is in close proximity to the thyrocervical trunk. It is intended to split into two terminal branches by ascending. The anterior scalene muscle receives blood sustenance from the inferior thyroid artery, which is the first terminal branch.
The blood supply to the medium and posterior scalene is directed by the second terminal branch, also referred to as the ascending or superficial cervical artery.
Venous Drainage
The venous trunk that’s accountable for collecting blood from the scalene muscles is the brachiocephalic venous trunk. The latter originates from the vertebral vein, a branch.
There are over 300 lymphatic nodes in the area surrounding the cervical tract. The back triangle of the neck is always home to those who are in charge of removing lymph from the scalene muscles. The drained lymph enters the left and right jugular lymphatic trunks. Additionally, the lymph gathered in the left portion will terminate in the thoracic duct, while the lymph collected in the right portion will go into the right lymphatic duct.
Actions
Elevation of first and second ribs.
Structures and Function
As supplementary respiratory muscles, the scalene muscles raise the first two ribs during a forced inspiratory act. The scalene muscles are actually electrically active at all times, including during spontaneous breathing. When the arm is elevated and the body is supine, the scalene muscles are highly active, even when they are not used as respiratory muscles. They function as postural muscles to keep the cervical tract in place or to actively participate in neck motions. They have the ability to tilt the neck and impede the first rotation of the head. A neck flexion is made possible by a bilateral scalene contraction.
The intercostal muscle afferents (between the eighth and tenth ribs, anteriorly) are closely related to one another. The scalene muscles contract bilaterally in response to their unilateral activation. The exact nature of the link is unknown. Most likely, an inspiration requiring the lower ribs to step in would activate the scalene muscles to help in breathing.
Relations
Located in the lateral region of the neck, the scalenus anterior muscle is situated behind the phrenic nerve and in front of the subclavian artery. It has connections to numerous neck structures;
It is associated with the pleura, the roots of the brachial plexus, the subclavian artery, and the suprapleural membrane posteriorly.
The omohyoid, sternocleidomastoid, subclavius, and clavicle muscles are located anteriorly to the muscle.
The phrenic nerve is formed by the spinal roots C3 to C5, which create the prevertebral fascia, the lateral portion of the carotid sheath, the transverse cervical, suprascapular, and ascending cervical arteries, the subclavian vein, and the right anterior side of the scalenus anterior.
The anterior boundary of the interscalene (scalene) triangle is formed by the scalenus anterior muscle. The scalenus medius forms the space’s posterior border, while the first rib makes up its inferior border. This area is significant because the third segment of the subclavian artery and the trunks of the brachial plexus pass through it.
Embryology
In the seventh week of the embryo’s gestation, the myoblasts of the hypaxial section of the cervical myotomes give rise to the scalene muscles, prevertebral muscles, and geniohyoid muscles. Myoblast migration through connective tissue determines the pattern of muscle development. The somitic mesoderm and the cervical region of connective tissue are not the same.
Anatomical Variations
Like any other anatomical district, the scalene muscles have a variety of anatomical characteristics.
The anterior scalene muscle may not include C6 or may have its origin in C2. Insertion of the muscle could involve not just the first rib but also the second or third thoracic rib. The anterior scalene muscle might travel below the subclavian artery, either homolaterally or bilaterally (right and left). It was also located behind the first thoracic nerve. The anterior scalene muscle is missing on one side or bilaterally in several situations reported in the literature.
When inserted into the transverse processes of the atlas cervical vertebra, the middle scalene muscle may veer, ultimately landing on the second thoracic rib. A middle scalene muscle auxiliary that forms a bridge with the anterior scalene muscle has been identified in certain research studies. A thoracic outlet syndrome-related symptom picture may result from this anatomical variation.
Some of the fibers of the posterior scalene muscle can unite with the middle scalene or the first intercostal muscle to form a single muscular tissue that may involve the cervical vertebrae from C3 to C7. Finally, it may come into contact with the third thoracic rib. This muscle might not exist in certain individuals. Brachial plexus branches like C7 and C8, which end on the posterior scalene muscle, have the potential to pierce the middle scalene. A dorsal and a ventral part are the possible two layers that make up the posterior scalene muscle, according to multiple authors.
The thoracic outflow may be extensively affected by the flattened minimum scalene. The C6 and C7 vertebrae may be involved in the genesis of this muscle.
Surgical Importance
Secondary to direct or indirect mechanical compression of the brachial plexus and/or subclavian arteries between the clavicle, scalene muscles, and first rib, thoracic outlet syndrome (TOS) develops. The most frequent clinical symptoms that occur are upper extremity paresthesias, discomfort, and exhaustion.
Diagnosing dynamic, postural-based symptoms can often be difficult. The latter happens when the upper extremity is elevated to a greater degree and as a result of neurovascular compression. Patients with the previously listed symptoms may be suspected of having TOS, and an additional indication for a diagnosis of TOS is the existence of a cervical rib, which occurs in 0.5% of cases.
Case reports exist describing different types of TOS that result from hypertrophy of the anterior scalene muscle. Sometimes it is necessary to remove the scalene, either the middle or anterior muscles (a procedure known as a scalenectomy). Should the patient exhibit aberrant muscle bundles that have the potential to compress the vascular-nervous brachial package—a condition known as the “wedge-sickle sign”—muscular excision is required.
In some cases, injections of type A botulinum toxin (botox) can be used to treat symptoms acutely when the disease is related to the scalene muscle itself. These are also beneficial for elderly individuals who might have to postpone surgery. In specific circumstances of spasmodic torticollis or cervical dystonia, botox injections can help alleviate symptoms as well.
Neck Mass Dissections
The scalene muscle can develop tumors; one type of tumor is called a myopericytoma. Because of its extreme rarity, this tumor frequently requires surgical removal. Intramural dissection is a surgical procedure used to remove a tumor or mass that resects the tumor bed either slightly or significantly.
Myxoma, a rare mesenchymal tumor of the head and neck, is another type of tumor. Benign tumors, like fibromatosis inside the muscle, are more commonly discovered and frequently surgically removed. To determine the type of tumor, biopsies on the lymph nodes of the scalene muscles are an option.
Splenectomy may be necessary in some circumstances in order to provide room for the removal of deeper malignancies, like a cervical schwannoma. Lastly, a direct trauma may have subsequent mass effects, leading to an intramuscular hemangioma.
Nerve Blocks and Catheter Considerations
The importance of nerve blocks and nerve catheters is rising as the healthcare system continues to move toward more procedures that are performed as outpatients. Nerve blocks have a variety of uses, some of which include treating depressive-type symptoms or alleviating neurological pain.
Because continuous interscalene has been shown to have reduced rates of toxicity and reported levels of symptomatic rebound after the anesthetic wears off, it is recommended in the literature above single-injection blocks. The pharmacological inhibition of the stellate ganglion is another invasive procedure that involves inserting a needle through several tissues, including the anterior and middle scalene.
Clinical Importance
Instrumental Evaluation
To examine the function of the scalene muscles, electromyography can be utilized to discover contractile abnormalities. Sonography, or ultrasound, as well as other more costly devices like magnetic resonance imaging and CT scans, can be used for this.
To assess whether vascular compromise exists, there are no acceptable manual techniques to identify the affected location or determine if the source is arterial or venous. To diagnose vascular disease at the scalene level, an echo-color Doppler examination is the only method available.
In clinical circumstances where thoracic outlet syndrome is suspected, electromyography may be utilized. It has been demonstrated that individuals with temporomandibular joint dysfunction exhibit more electrical activity in the anterior scalene compared to those without mandibular joint issues.
Both the osteopath and the physiotherapist might find this information helpful. We are aware that a mandibular issue may be a symptom rather than the underlying cause of a patient’s reduced ventilatory capacity due to malfunction of the scalene muscles.
Manual Assessment of Scalene Muscles
Palpation is an important diagnostic, classification, and assessment tool. The tactile sensitivity of the fingertip can be utilized to assess micron-scale things. Physicians can use palpation to assess the posture of the joints, identify uncomfortable locations, and detect anomalies in the tissue, such as warmth, tone, and hardness on the surface and deep within the different layers.
From the perspective of osteopathic medicine, tissue damage invariably results in a “mnemonic tattoo.” This enables medical professionals to detect the path of the tissue toward the original lesion at the touch level right away. This lesional tattoo is the result of the cells’ modified preferred vector and shape as well as their altered behavior in response to touch pressure.
The literature states that in order to confirm the status of the scalene muscles through palpation, we must ask the patient to laterally flex their neck in the opposite direction from our fingers—that is, to touch the right while flexing their neck to the left. In this method, the scalene muscles are put in tension, and it is simpler to palpate them.
With repeated breathing efforts, the posterior scalene and other scalene musculature can get fatigued, especially in patients with chronic obstructive pulmonary disease. These contractile regions are frequently hypertonic and overstimulated as compared to healthy persons.
To measure tone and the tissue quality of the scalene muscles, the examiner must place himself behind the patient, who is supine (best) or seated. They maintain the eminence hypothenar in the supraclavicular fossa anatomical area by holding and controlling the patient’s neck with one hand as he attempts to keep the first thoracic rib from rising. This last position is required to prevent improper tension of the muscles and to stop the first rib from migrating during neck movement.
The patient’s head bends to the right and tilts to the left for the anterior scalene.
Respecting the functional anatomy, the head of the middle scalene bends to the left without rotating. When the muscle’s insertion location is being stretched, the hand on the ribs is helpful, along with an extra passive movement of the head. Reduced excursion is the outcome of aberrant muscular tension and frequently uncomfortable motions. Tension and soreness in the anterior and middle scalene muscles can be frequent causes of thoracic outlet syndrome.
Try to rotate the head to the left, but keep the neck slightly inclined to avoid elevating the first rib due to the posterior scalene.
The same positions utilized to evaluate any constraints on each part of the scalene muscles can also be employed for stretching exercises. The patient is unable to comprehend the movement of the first rib during the little movements permitted by each scalene muscle, hence the exercise needs to be done under the supervision of an operator.
An operator stands or sits behind the patient to distinguish between a sternocleidomastoid muscle (SCM) malfunction and an issue with the scalene muscles. The patient’s shoulders are immobilized by the operator, who puts his hands on them and requests a deep breath. In this manner, the initial ribs can be elevated and the sternocleidomastoid muscle’s intervention is disregarded. The issues with the scalene muscles will be emphasized if they are uncomfortable or restricted in any way. Conversely, by resting the thumbs during a forced inhale, the elevation of the first ribs is avoided, drawing attention to SCM.
Clinical Implications
Distant symptoms could be caused by an increase in the anterior scalene muscle’s tone or thickness. A subclavian artery clot would cause cyanosis, pallor, and cold sensation in the limbs, as well as difficulties moving the arm. In non-physiological circumstances (hypertrophy, shortening), C5-C6 may cross the muscle and result in paresthesia, anesthesia, or weakening in the muscles these roots innervate.
There may be symptoms including tingling, discomfort, and weakness in the hand and interosseous muscles if the root of C8 runs back to the anterior scalene, the site of the two attacks. Headaches may arise from the mixing of the longus capitis muscle and the anterior scalene tendon.
The middle scalene (hypertonic and hypertrophic, shortened) is where the suprascapular nerve passes through. This can cause symptoms like weakness in the supraspinatus and infraspinatus muscles, paresthesia, and pain in the shoulder and scapular region. The scapulohumeral joint’s arthrokinematics can then change. If the transverse cervical artery’s deep branch goes through a muscle, it may result in complex symptomatology or make diagnosing the issue more challenging.
An increase in posterior scalene muscle thickness may cause pain or weakness in the anterior serratus muscle, scapula elevator, and rhomboid muscles, as well as change the path of the long thoracic nerve and the scapular dorsal nerve.
Minimum scalene may cause symptoms associated with thoracic outlet syndrome by reducing the passage space for the brachial plexus, the subclavian artery, and the subclavian vein.
Chronic Obstructive Pulmonary Disease (COPD)
The diaphragm muscle weakens and flattens in COPD patients, which makes the auxiliary respiratory muscles work harder to intervene during inhalation. How do the muscles of the scalene get along? It has been shown that there is an inverse link between the diaphragm muscle’s thickness and the scalene muscles’ thickness, with the diaphragm muscle’s thickness decreasing and the scalene muscles’ hypertrophy increasing. Usually, the latter has a higher concentration of red or aerobic fibers; but, while under continuous strain and with a heavier load, the red fibers become more massive in terms of proteins, mitochondria, enzymes, and capillaries.
The scalene muscles increase tone and volume for both hypertrophy and the chronic shortening of the muscles themselves, which exacerbates the aggravating nature of COPD. The initial ribs are in an inspiratory position, with the pulmonary dome in continual strain. The dome will find it difficult to descend during inspiration, which will make breathing even more difficult by lowering pulmonary vital capacity.
It has been demonstrated that a forward-leaning head posture affects the lung’s essential capacity for the same scalene muscle reasons previously mentioned: shortening and increased tone. This occurs regardless of the existence of respiratory conditions.
Clinical studies have demonstrated that stretching is a useful strategy for minimizing the non-physiological adaptation of the lung caused by the scalene muscles during shortening.
Myofascial Pain
Pain can sometimes come from the scalene muscles. Muscle bulk can, on the one hand, cause unpleasant variations and trigger points. Conversely, the same fascia that binds the muscle to its surrounding tissues, viscera, and joints, as well as the connective tissue that covers and surrounds the muscle itself, can manifest as painful abnormalities. A sore cervical tract might be caused by the scalene muscles. Pain might be felt directly, or it can be the source of farther-off symptoms like migraines.
These fascial anomalies or changes in the contractile tissue can arise from diseases that change the thoracic conformation, like scoliosis, which can result in a non-physiological cervical biomechanical environment, or from traumas such as whiplash or incorrect daily attitudes.
Lung vital capacity may be lowered by this persistent pain. Research indicates that combining breathing techniques with scalene muscle retraining can help reduce or even completely remove a patient’s pain.
Osteopathy using indirect or fascial techniques is another method for decreasing myofascial pain. Numerous researches demonstrate how these mild methods might lessen regional discomfort when there is systemic involvement. Both the sympathetic nervous system’s activity and the blood readings of the inflammatory indices decrease.
Physiotherapists’ taping or dry needle therapy are two other more modern methods that have been documented in the literature. Despite the promising outcomes, the mechanisms of action of these final two therapeutic methods remain poorly known.
Anti-inflammatory medications merely address the symptoms; they do not correct the structural defects. There is a significant likelihood that the pain will return when the analgesic effect wears off.
In patients showing a posture with a forward head position, they demonstrate a greater pain sensitivity, notably for the trapezius and the scalenus medius; these muscles also demonstrate a decreased range of motion in such circumstances.
It’s likely that a manual technique to increase the scalenus medius’ (and trapezius’) functional ability could enhance everyday head and neck posture. Cervicogenic headache discomfort may be associated with a forward head posture.
References
Bordoni, B. (2023, April 10). Anatomy, Head and Neck, Scalenus Muscle. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK519058/

3 Comments