Brachialis Syndrome
Table of Contents
Introduction
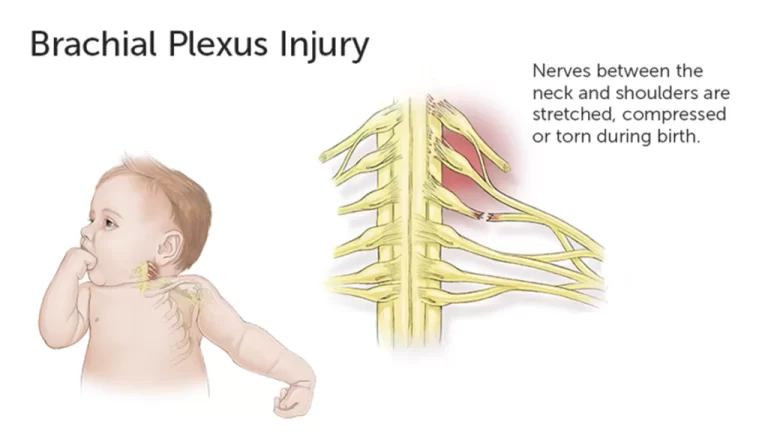
Brachialis syndrome, also known as anterior interosseous nerve syndrome, is a rare condition that occurs when the anterior interosseous nerve (AIN) is compressed or injured. The AIN is a branch of the median nerve, which originates from the brachial plexus in the neck and travels down the arm into the forearm.
The AIN supplies the deep flexor muscles of the forearm, including the flexor pollicis longus, flexor digitorum profundus (index and middle fingers), and pronator quadratus muscles.
Anatomy
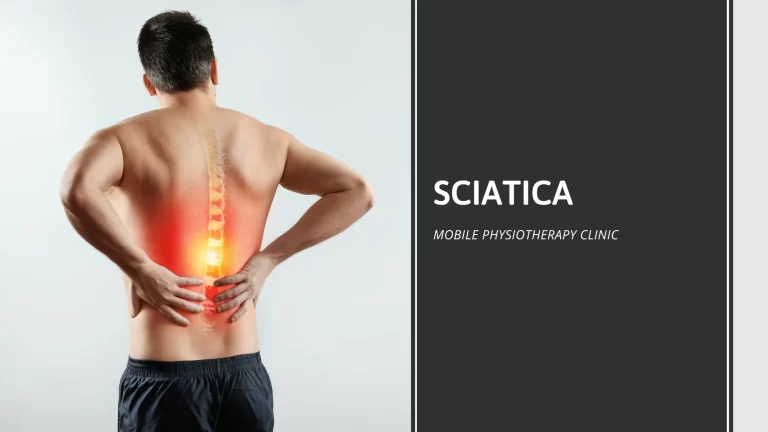
Anatomy of the Parsonage-Turner syndrome (PTS).
It is a network of nerves that travels from your spine through your neck, down your arms, and into each of your armpits. Motor neurons and axons are the primary targets of Parsonage-Turner syndrome (PTS). Movement is under the direction of these nerves. It causes muscle weakness because of this.
Anatomy of the anterior interosseous nerve (AIN)
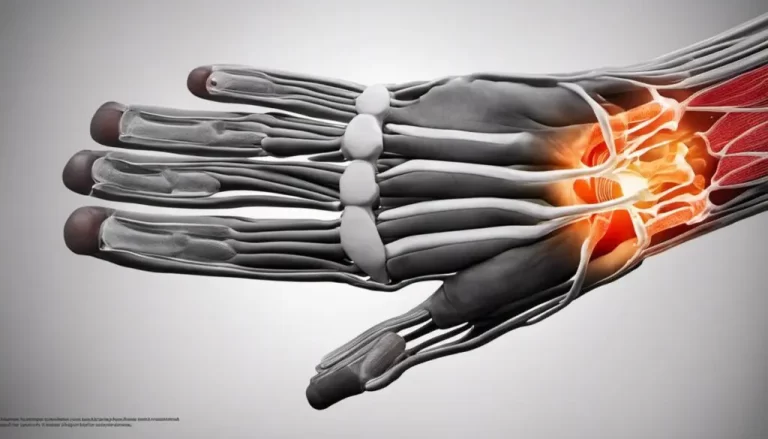
The AIN originates from the median nerve at the level of the brachialis muscle in the antecubital fossa, which is the area of the elbow joint. It then runs deep to the brachialis muscle and travels along the interosseous membrane, which is a thick fibrous sheet that connects the radius and ulna bones of the forearm. The AIN finally branches into three terminal branches, which innervate the deep flexor muscles of the forearm.
Phases of Brachialis syndrome
The Brachialis syndrome typically progresses through three stages:
Phase 1 (acute pain phase): Usually affecting one shoulder, this phase is characterized by sudden, severe discomfort. Both the phase and the pain may persist for several days or weeks. Recovery generally takes longer the longer this phase lasts.
Step 2:. You experience muscle weakness, such as shoulder girdle weakness and arm weakness, after the pain goes away. Atrophy, or muscle loss, may result from this. Phase 2 may take longer than the usual six to eighteen months.
Step 3:. Your muscles recover their strength and functionality over time.
Cause of Brachialis syndrome
The most common cause of brachialis syndrome (BS) is prolonged elbow extension. This can occur during surgery or other medical procedures that require the patient to keep their arm extended for a long period. Prolonged elbow extension can cause the brachialis muscle to swell and compress the median nerve.
Other causes of Brachialis syndrome(BS) include:
Trauma to the elbow: This can cause swelling and inflammation of the brachialis muscle, which can compress the median nerve.
Inflammation of the brachialis muscle: This can be caused by a variety of factors, such as infection, autoimmune diseases, and certain medications.
Tumors: Tumors in the arm can compress the median nerve and cause BS.
Anomalies of the median nerve: Certain abnormalities of the median nerve, such as a nerve sheath tumor, can make the nerve more susceptible to compression.
Traumatic injury: This is the most common cause of brachialis syndrome. It can happen from a direct blow to the forearm, a fall on an outstretched arm, or from repetitive overuse of the hand and forearm muscles.
Compression: The AIN can be compressed by bone spurs, ganglion cysts, or tumors. It can also be compressed by tight muscles or fascia.
Postoperative: This is a rare cause of brachialis syndrome. It can occur after surgery to the elbow, forearm, or wrist.
In some cases, the cause of BS is unknown. This is called idiopathic BS.
The specific cause of Parsonage-Turner syndrome is unknown to investigators. The primary cause, according to them, is an abnormal immune-mediated response. They have two possibilities.
- Your brachial plexus is directly affected by bacterial, viral, or parasitic infections, which results in the symptoms.
- In the process of attacking the bacteria, virus, or antigen, your immune system harms your brachial plexus.
The most frequent cause of PTS is a recent viral infection. The most common viral illnesses involved are the following ones:
- The coxsackie B virus is responsible for several illnesses, including viral hepatitis, myocarditis, pneumonia, aseptic meningitis, and encephalitis.
- Human immunodeficiency virus, or HIV.
- The fifth illness (B19 parvovirus).
- Mumps.
- Variola major and minor smallpox.
Symptoms Brachialis syndrome
Brachialis syndrome, also known as Parsonage-Turner syndrome, is a rare condition caused by compression of the median nerve, a major nerve in the arm. This compression can lead to several symptoms, such as:
The primary signs of Parsonage-Turner syndrome are sudden pain followed by muscle weakness. Their effects may include:
- Arm.
- Upper limb.
- Front arm.
- Gripping or wrist
The symptoms of brachialis syndrome can vary depending on the severity of the injury. They may include:
- Pain and numbness in the forearm: This is the most common symptom, and is typically located in the middle of the forearm.
- Weakness in the grip: This is another common symptom, and is caused by the weakness of the deep flexor muscles of the forearm.
- Difficulty flexing the thumb, index, and middle fingers: This is also a common symptom, and is caused by the weakness of the flexor digitorum profundus muscles.
- Difficulty pronating the forearm: This is a less common symptom, and is caused by the weakness of the pronator quadratus muscle
Approximately 80% of the time, it only affects one arm (unilaterally), usually your dominant arm or hand. About 20% of cases are bilateral, affecting both arms. In rare cases, it may also impact your lower extremities and trunk.
Most of the time, the pain starts suddenly. It is intense and sharp, and it usually gets worse at night. Hours or even weeks can pass during periods of severe pain. Your afflicted arm’s muscles will begin to weaken after the pain subsides.
Your forearm and hand may also be affected, but your shoulder and upper arm will probably feel the most weakness. Sometimes, weakness can cause problems with your diaphragm or chest. When your muscles are weak, you gradually lose muscle mass (muscle atrophy).
Because PTS affects specific nerves, the severity of symptoms varies greatly from person to person. Additional PTS symptoms may consist of:
- Reflex problems with the arm that is affected.
- Numbness or unusual pain (paresthesia) in the affected arm. This could have a burning, prickling, or tickling sensation.
- Dislocation of the shoulder in part.
- Abnormal mobility in the affected joints.
- Winged scapula: an extension of the shoulder blade.
- Contraction of the tendons or muscles in the affected arm.
- Hands that are spotted, red, or purple (from poor circulation).
- Swelling in your hands.
- Breathing difficulty (dyspnea). It’s uncommon.
- Numbness, tingling, or burning pain radiating down the arm, into the hand and fingers. This pain is often described as an electrical shock or burning sensation
- Weakness or loss of muscle function in the hand and fingers. This can make it difficult to grasp objects, make fine motor movements, or extend the thumb.
- Loss of sensation or reduced ability to feel temperature changes, light touch, or vibrations.
- Difficulty moving or flexing the wrist and fingers.
The symptoms of brachialis syndrome usually develop within hours or days of a prolonged elbow extension event. Prolonged elbow extension can occur during surgery, anesthesia, or other medical procedures that require the arm to be kept in an extended position for an extended period.
It is important to note that the symptoms of brachialis syndrome can also be caused by other conditions, such as carpal tunnel syndrome, cubital tunnel syndrome, or cervical radiculopathy. Therefore, it is essential to see a doctor for a proper diagnosis to determine the underlying cause of your symptoms.
Here are some additional symptoms that may be associated with brachialis syndrome:
- Muscle cramps or spasms in the arm and hand
- Increased sensitivity to touch
- Difficulty sleeping due to pain or discomfort
- Alterations in the affected area’s skin tone or texture
Diagnosis
Diagnosis of brachialis syndrome (BS) typically involves a combination of medical history, physical examination, and diagnostic tests. Here’s a step-by-step overview of the diagnosis process:
- Medical History:
Your doctor will begin by gathering a detailed medical history to understand your symptoms, potential risk factors, and any underlying medical conditions you may have. This will help rule out other possible causes of your symptoms and narrow down the diagnostic possibilities.
- Physical Examination:
The diagnosis of brachialis syndrome is based on a physical examination and nerve conduction studies. The physical examination may reveal weakness in the muscles of the forearm, especially the flexor pollicis longus and flexor digitorum profundus (index and middle fingers). Nerve conduction studies can help to confirm the diagnosis by measuring the speed of electrical impulses traveling through the nerve.
During the physical examination, your doctor will thoroughly assess your neurological function, focusing on the areas innervated by the median nerve. This may include testing your:
Sensory function: Ability to feel light touch, temperature changes, and pain in the hand and fingers.
Motor function: Strength and coordination of your hand and fingers, including the ability to grasp objects, pinch, and make fine movements.
Reflexes: Response of your muscles to specific stimuli.
- Diagnostic Tests:
Depending on your symptoms, physical examination findings, and doctor’s assessment, additional diagnostic tests may be recommended to confirm the diagnosis of BS and rule out other conditions. These tests may include:
Electromyography (EMG): EMG measures the electrical activity of your muscles and nerves, helping to identify any abnormalities in the median nerve.
Nerve Conduction Study (NCS): NCS assesses the speed and quality of electrical signals traveling through the median nerve, providing further insight into nerve function.
Imaging Studies: In some cases, imaging tests like MRI or CT scans may be ordered to visualize the brachialis muscle and surrounding structures, looking for any signs of inflammation, compression, or other abnormalities.
Differential Diagnosis:
It is crucial to distinguish BS from other conditions that can cause similar symptoms, such as:
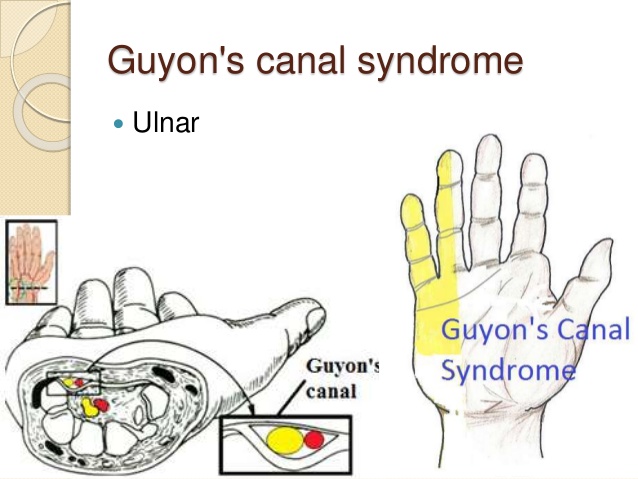
- Carpal Tunnel Syndrome: Compression of the median nerve in the wrist causes carpal tunnel syndrome.
- Cubital Tunnel Syndrome: Compression of the median nerve at the elbow.
- Cervical Radiculopathy: Compression of a nerve root in the neck, causing symptoms in the arm and hand.
Ruling Out Other Causes:
In order to rule out further possible reasons for your symptoms, your doctor might also prescribe tests like these:
- Electrolyte imbalances: Imbalances in electrolytes like potassium can affect nerve function.
- Vitamin deficiencies: Deficiencies in vitamins like B12 can cause nerve damage.
- Medications: Certain medications can have side effects that mimic the symptoms of BS.
Once all other potential causes have been ruled out, a diagnosis of BS can be confirmed based on the medical history, physical examination findings, and supporting diagnostic test results.
Treatment of Brachialis Syndrome
Treatment for brachialis syndrome typically involves a combination of nonsurgical and surgical interventions.
Nonsurgical Treatment
Nonsurgical treatment is the first line of therapy for brachialis syndrome. The goals of nonsurgical treatment are to relieve pain, improve the range of motion, and prevent further damage to the median nerve. Nonsurgical treatment options may include:
- Rest: Avoid activities that aggravate the pain, such as overhead lifting or repetitive movements.
- Ice application: Apply ice packs to the affected area for 15-20 minutes at a time, several times a day.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Taking over-the-counter NSAIDs, such as ibuprofen or naproxen, to reduce pain and inflammation.
- Physical therapy: Working with a physical therapist to develop a stretching and strengthening program to improve range of motion and muscle function.
- Corticosteroid injections: Receiving injections of corticosteroids into the affected area to reduce inflammation and pain.
BS has no known cause or cure; it typically goes away on its own. However, rapid diagnosis and supportive care may improve your prognosis.
Your physician will suggest specific treatments to help you manage your symptoms. You might be collaborating with a team of specialists to develop a care plan. On this team could be:
- Doctors of primary care (PCPs).
- Orthopaedists.
- Neuroscientists.
- Experts in neuromuscular diseases.
- Therapists for the body.
Among the treatments for the acute pain stage are:
- Analgesics (pain medication, such as NSAIDs sold over-the-counter).
steroid oral doses. - Using a shoulder stabilizer or minimizing the use of your arm will immobilize it.
- Herbal medicine/ Acupunture
Your healthcare provider will probably suggest the following treatments after the acute phase has passed:
Co-analgesics: These are drugs designed especially to relieve pain in the nerves. Amitriptyline, carbamazepine, and gabapentin are a few examples.
If nothing else has relieved your symptoms, your doctor might suggest surgery in extreme circumstances. Surgical techniques include nerve grafting and tendon transfers.
Physiotherapy treatment of Brachialis Syndrome
Patients may be referred for physical therapy in addition to medication therapy. The therapist’s main goals in physical therapy are to maintain periscapular motion through strengthening exercises, patient education, upper-extremity range of motion, and adjunct pain relief modalities. An important part of treating this condition is physical therapy.
TENS is one modality that can aid in pain management. The degree of muscle denervation, the degree of weakness, the degree of altered biomechanics, and the patient’s premorbid functional level of activity have an effect on when and how strengthening exercises should be performed.
Depending on the nature and extent of the injury, different physiotherapy treatments are recommended for BS injuries. In less severe cases, bracing and surgery may be required; in more severe cases, physiotherapy and rehabilitation will aid in recovery. Returning to one’s prior level of function and avoiding future disability are the two constant goals.
Goals of physiotherapy treatment.
- Development of coordination, stamina, strength, and flexibility.
- Preserving range of motion through passive motion, physical therapy, splinting, and the positioning and defense of denervate dermatomes. Adoption of adaptive devices and functional training, if necessary.
- TENS and acupuncture are used to control pain.
- Using massage treatment, compression clothing, and education to manage chronic edema.
Depending on the muscles involved, range of motion exercises are obviously important and may need the help of a physical or occupational therapist. For obvious reasons, strengthening exercises are not recommended for muscles that have lost all innervation. Without voluntary movement, resistance training is also not possible.
Depending on which nerve or region of the brachial plexus is affected, strengthening the rotator cuff, other upper limb muscles, or scapular stabilization may be recommended if complete denervation is not achieved. Resistance training needs to be modified based on the patient’s level of pain and ability to exercise locally.
Although its use is still uncertain electrical stimulation (ES) should be taken into account when the denervated state lasts longer than four months. If the right stimulation pattern is selected, electroshock therapy (ES) can be a helpful procedure for maintaining or returning the denervated muscles’ normal characteristics. The best time to begin ES treatment is as soon as possible following a muscle nerve injury; the less recovery there is, the longer the time between the beginning of denervation and the beginning of stimulation. ES indicates an increase in muscle mass and quality without significantly impeding axon regeneration or muscle reinnervation.
Surgical Treatment
Surgical treatment is typically considered for brachialis syndrome which does not respond to nonsurgical treatment. The goal of surgery is to decompress the median nerve by releasing the compressed area. Surgical options may include:
Neurolysis: Releasing the median nerve from scar tissue or other compression.
Fasciotomy: Releasing the fascia, a sheath of tissue that surrounds the muscles, to reduce pressure on the median nerve.
Nerve graft: Replacing a damaged section of the median nerve with a graft from another part of the body.
Recovery
The recovery time for brachialis syndrome varies depending on the severity of the injury and the type of treatment. In most cases, nonsurgical treatment can resolve symptoms within a few weeks or months. Surgical recovery may take longer, and some patients may experience permanent nerve damage.
note: The best way to prevent brachialis syndrome is to avoid prolonged arm positioning during surgery. If arm positioning is necessary, surgeons should take steps to protect the median nerve, such as using padding and avoiding excessive pressure.
Risk factors
Certain circumstances and conditions may increase your risk of developing Parsonage-Turner syndrome, according to researchers. These consist of:
- Recent anesthesia or surgery.
- Ehlers-Danlos syndrome.
- Autoimmune conditions like lupus, temporal arteritis, and polyarteritis nodosa.
- Injured shoulder traumatically.
- Exercise that is hard on your shoulders.
- Vaccinations, or shots.
- Pregnancy as well as delivery.
- Radiation treatment.
- Spinal tap, or lumbar puncture.
- Getting contrast dye for a medical examination
Here are some risk factors that can increase the likelihood of developing Brachialis syndrome:
Prolonged elbow extension: Prolonged elbow extension is the most common risk factor for Brachialis syndrome. This can occur during surgery, anesthesia, or other medical procedures that require the arm to be kept in an extended position for an extended period.
Obesity: Obesity is another risk factor for Brachialis syndrome. This is because obesity can increase the amount of fat around the median nerve, making it more susceptible to compression.
Diabetes: Diabetes can also increase the risk of Brachialis syndrome. This is because diabetes can damage the nerves, including the median nerve.
History of trauma to the elbow: A history of trauma to the elbow can also increase the risk of Brachialis syndrome. This is because trauma can damage the brachialis muscle or the median nerve.
Repetitive arm movements: Repetitive arm movements, such as those involved in certain occupations or hobbies, can also increase the risk of Brachialis syndrome. This is because repetitive movements can irritate the median nerve.
Certain medications: Certain medications, such as corticosteroids, can also increase the risk of Brachialis syndrome. This is because corticosteroids can weaken the muscles and tendons, making them more susceptible to injury.
Here are some additional tips to help reduce your risk of developing Brachialis syndrome:
Avoid prolonged elbow extension: Whenever possible, avoid keeping your arm in an extended position for long periods of time. If you must keep your arm extended for a medical procedure, talk to your doctor about ways to reduce the risk of Brachialis syndrome.
Maintain a healthy weight: If you are overweight or obese, losing weight can help reduce your risk of Brachialis syndrome.
Control your blood sugar: If you have diabetes, it is important to control your blood sugar levels to help prevent nerve damage.
Avoid repetitive arm movements: If you perform repetitive arm movements at work or for a hobby, take frequent breaks to rest your arms.
Talk to your doctor: If you are concerned about your risk of Brachialis syndrome, talk to your doctor. They can help you assess your risk factors and recommend preventive measures.
Remember, early diagnosis and treatment of Brachialis syndrome are crucial for preventing permanent nerve damage. If you are experiencing any symptoms of Brachialis syndrome, consult a doctor promptly to receive an accurate diagnosis and appropriate treatment.
Complication
Brachialis syndrome (BS) is a rare condition that causes compression of the median nerve, a major nerve in the arm. The compression is caused by swelling of the brachialis muscle, which is located in the front of the upper arm. The swelling is caused by prolonged elbow extension, which can occur during surgery or other medical procedures.
If left untreated, BS can lead to several complications, including:
Permanent nerve damage: If the median nerve is compressed for a long period of time, it can be permanently damaged. This can cause permanent numbness, tingling, weakness, and pain in the hand and fingers.
Muscle atrophy: The muscles in the hand and fingers that are controlled by the median nerve can atrophy, or waste away if they are not used properly. This can make it difficult to grasp objects, make fine motor movements, and extend the thumb.
Painful contractures: The muscles in the hand and fingers can also contract, or shorten if they are not used properly. This can cause painful contractures that can make it difficult to move the fingers and hand.
In severe cases, BS can also lead to:
Sudeck’s atrophy: This is a complex condition that causes pain, swelling, and stiffness in the hand and fingers. It is caused by damage to the sympathetic nervous system, which is responsible for regulating blood flow and temperature in the extremities.
Complex regional pain syndrome (CRPS): This is a chronic pain condition that can affect any part of the body, but it is most common in the arms and legs. It is caused by damage to the nervous system, and it can cause intense pain, swelling, and changes in skin texture and temperature.
Prevention
Preventing brachialis syndrome is crucial to avoid the potential complications associated with this condition.
Here are some effective measures to reduce your risk of developing brachialis syndrome:
Minimize Prolonged Elbow Extension: Avoid keeping your arm in an extended position for extended periods. This is particularly important during medical procedures or activities that require prolonged elbow extension. If you must keep your arm extended, consult your doctor about ways to mitigate the risk of brachialis syndrome.
Maintain a Healthy Weight: Excess weight can increase the pressure on the median nerve, making it more susceptible to compression. Losing weight can help reduce the risk of brachialis syndrome.
Control Blood Sugar Levels: If you have diabetes, maintaining optimal blood sugar control can help prevent damage to the nerves, including the median nerve, and reduce the risk of brachialis syndrome.
Minimize Repetitive Arm Movements: Repetitive arm movements, especially those involving forceful grasping or twisting motions, can put a strain on the median nerve and increase the risk of brachialis syndrome. If your work or hobbies involve repetitive arm movements, take frequent breaks to rest your arms.
Maintain Proper Posture: Maintaining good posture, especially when sitting, can help reduce strain on the nerves in the arms and shoulders. Avoid slouching or hunching over, and keep your forearms and wrists straight.
Warm Up Before Exercise: Warming up properly before engaging in physical activities can help prepare your muscles and reduce the risk of injury, including brachialis syndrome.
Stretch Regularly: Stretching your arm and hand muscles regularly can help improve flexibility and reduce muscle tightness, which can contribute to brachialis syndrome.
Seek Prompt Medical Attention: If you experience any symptoms of brachialis syndrome, such as numbness, tingling, or pain in the arm, hand, or fingers, seek medical attention promptly. The prompt diagnosis and intervention can help avert irreversible nerve injury.
Remember, prevention is key to managing brachialis syndrome and avoiding its associated complications. By adopting these preventive measures and maintaining a healthy lifestyle, you can significantly reduce your risk of developing this condition.
Prognosis
Most people with brachialis syndrome recover completely with treatment. But at times the symptoms might still be present. If the symptoms are severe or do not improve with treatment, the person may need to have surgery to repair the damaged nerve.
Prognosis for different severity levels:
Mild BS: In cases of mild BS, where the nerve compression is relatively minor, most patients experience complete recovery within a few weeks or months with conservative treatment.
Moderate BS: With moderate BS, the nerve compression may cause more pronounced symptoms, and recovery may take longer, typically several months or a year. However, full recovery is still possible with appropriate treatment.
Severe BS: Severe BS, characterized by significant nerve compression and extensive nerve damage, may require surgical intervention to decompress the median nerve. Recovery in severe cases may take longer and may result in some residual numbness or tingling in the hand and forearm.
Outlook
The outlook for brachialis syndrome (BS) is generally favorable with prompt diagnosis and treatment. Most patients make a full recovery, although some may experience residual numbness or tingling in the hand and forearm.
Factors that influence the outlook for BS:
The severity of nerve compression: The severity of nerve compression determines the extent of damage to the median nerve and the likelihood of residual symptoms.
Time to diagnosis and treatment: Earlier diagnosis and treatment lead to better outcomes and reduce the risk of permanent nerve damage.
Patient adherence to treatment: Following the recommended treatment plan, including rest, physical therapy, and medication, can significantly improve recovery.
Overall health and lifestyle: Maintaining a healthy lifestyle, including managing weight, controlling blood sugar levels, and avoiding repetitive arm movements, can promote healing and prevent recurrence.
Overall, the outlook for BS is positive with timely diagnosis and proper management. Early intervention and adherence to treatment recommendations can significantly improve the chances of a full recovery.
FAQs
Tingling or loss of sensation in the arm or hand. incapacity to move or control the hand, wrist, arm, or shoulder. An arm left hanging, lifeless. a sharp, burning, or abruptly intense pain in the arm or shoulder.
In the meantime, your doctor might prescribe corticosteroids to treat your discomfort. The brachial plexus region’s nerves may be repaired surgically if the brachial neuritis is the consequence of an accident and the procedure can be completed quickly.
If at all possible, we advise starting 24 to 48 hours after the onset of pain and weaning off the oral prednisone (1 mg/kg/day) over a further two weeks. The initial pain can be fairly severe and paralyzing, therefore it’s important to manage it properly.
Brachial neuritis, also known as Parsonage-Turner syndrome, is a neurological disorder that produces abrupt, excruciating shoulder and upper arm discomfort. If the pain doesn’t go away, it might take a few days to a few weeks. Pain is followed by muscle weakness in your forearm, hand, shoulder, or arm.
It could be necessary for you to rest the injured area until it heals. Nerves heal gradually; full healing could take several months or even years. Regular check-ups are necessary to ensure that your recovery progresses as planned. Your doctor will address the underlying medical condition if it is the cause of your injury.
The nerve may occasionally sustain bruising and eventually heal on its own. On the other hand, surgical intervention can be necessary to help improve or restore function to the hand or arm if a nerve is cut or crushed. Certain diseases can occasionally damage nerves and result in symptoms that are comparable in the upper extremities.
References
- Parsonage-Turner Syndrome. (n.d.). Physiopedia. https://www.physio-pedia.com/Parsonage-Turner_Syndrome
- Professional, C. C. M. (n.d.). Parsonage-Turner Syndrome. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/15390-parsonage-turner-syndrome
- Koehler, S. M., Meier, K. M., Lovy, A. J., Fitzpatrick, D., Kim, J., & Hausman, M. R. (2016, May 1). Brachialis syndrome: a rare consequence of patient positioning causing postoperative median neuropathy. Journal of Shoulder and Elbow Surgery; Elsevier BV. https://doi.org/10.1016/j.jse.2015.12.023
- Brachial Neuritis. (2019, November 19). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/brachial-neuritis