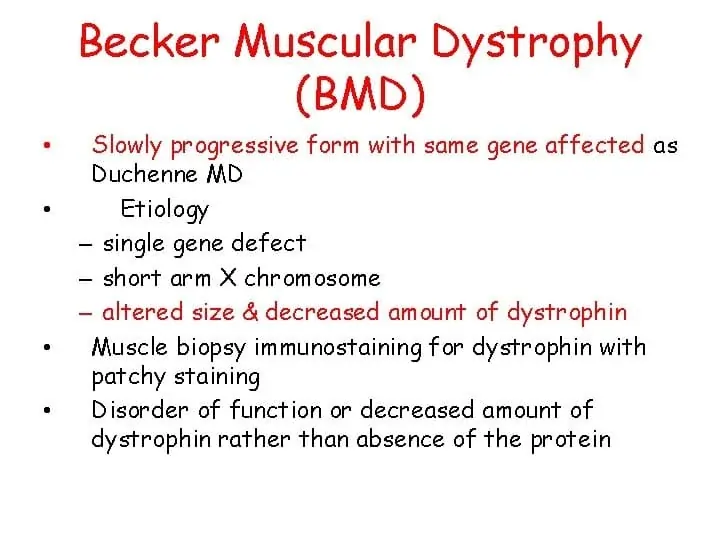
Medial Plica Syndrome:
Table of Contents
What is The Medial Plica Syndrome:
Plica syndrome may be a condition caused by inflammation within the lining of the knee.
It leads to achy knee pain which gets worse with activity, particularly up and down stairs, a sense of instability within the knee, and sometimes a catching or locking sensation.
Plicae are small folds within the synovium, the skinny structure that surrounds and contours the articulatio genus. Plica syndrome, aka plica synovial, can develop in any of the four knee plicas, the foremost common being within the medial plica.
Knee plica irritation occurs when the plica gets caught or pinched between the knee joint bones, usually thanks to a knee injury or overuse.
Definition:
Sometimes the plica located within the middle of your knee becomes irritated. this is often called plica syndrome.
Relevant anatomy:
A synovial plica may be a shelf-like membrane between the synovium of the patella and therefore the tibiofemoral joint. Plicae essentially contains mesenchymal tissue which is created within the knee during the embryological phase of development. This tissue forms a membrane that divides the knee into 3 compartments: the medial and lateral tibiofemoral compartments and therefore the suprapatellar bursa.
This tissue usually starts to involute (fold inward) at 8-12 weeks of fetal growth and is eventually resorbed, leaving one empty area between the distal femoral and proximal tibial epiphysis: one knee cavity. The movement of the fetus within the uterus contributes to the current resorption. Yet, in many individuals, the mesenchymal tissue isn’t fully resorbed and consequently, the cavitation of the genu remains incomplete. The result’s that in these individuals plicae will be observed, which represent inward folds of the membrane within the hinge joint. Various degrees of separation of the cavities are seen within the human knee. it’s estimated that plicae are present in about 50% of the population.
The synovial plica has an elastic nature which provides normal movement of the structures of the tibiofemoral joint without any restriction. Yet, when repeating the identical knee movement too often, like bending and straightening the knee, or in the case of trauma to the knee, these plicae can become irritated and inflamed. this could lead to a disorder called the plica syndrome. It refers to an inside derangement of the knee that prevents normal functioning of the knee.
It is a motivating problem, particularly seen in children and adolescents, and occurs when an otherwise normal structure within the knee becomes a source of knee pain thanks to injury or overuse. The diagnosis might sometimes be difficult because most symptoms of non-specific anterior or anteromedial knee pain can point to varied knee disorders. But if a plica has been diagnosed beyond any doubt as being the source of knee pain, it is treated correctly.
Types of Plica
In the knee, 4 sorts of plicae will be distinguished, looking at the anatomical location within the hinge joint cavities: suprapatellar, mediopatellar, infrapatellar, and lateral plicae. The last one isn’t seen and, therefore, there’s some controversy regarding its existence or its exact nature. The plicae within the knee can vary in both structure and size; they’ll be fibrous or fatty, longitudinal or crescent-shaped.
Suprapatellar plica
The suprapatellar plica also known as the plica synovial suprapatellar, superior plica, superomedial plica, medial suprapatellar plica, or septum could be domed shape, there is a crescent-shaped septum that presents in the tibiofemoral-joint of the knee between the suprapatellar bursa. it goes through the synovium at the anterior side of the femoral metaphysics, downwards to the posterior side of the quadriceps tendon before inserting above the patella. Its free border appears sharp, thin, wavy, or created in normal conditions. this kind of plica is often present as an arched or peripheral membrane around a gap, called porta. It often blends into the medial plica. because the suprapatellar plica has an anterior attachment to the quadriceps tendon, it helps in changing dimension and orientation when moving the knee.
According to arthroscopic investigations, the suprapatellar plicae can generally be differentiated by location and shape into differing types. Kim and Choe (1997) have given the subsequent 7 types:
- Absent No sharp-edged fold.
- Vestigial Plica with but 1 mm protrusion. Disappeared with external pressure
- Medial Plica present on the medial side of the suprapatellar pouch
- Lateral Plica present on the lateral side of the suprapatellar pouch
- Arch Plica does not present over the anterior femur but presents medially, laterally, or posteriorly.
- Hole Plica with a central defect extends completely across to the suprapatellar pouch.
- Complete Plica divides the suprapatellar pouch into two separate compartments
Medial patella plica
The medial patellar plica is additionally referred to as plica synovial mediopatellaris, medial synovial shelf, plica Alaris elongate, medial parapatellar plica, the meniscus of the patella, or after its first two descriptors as Lion’s band or Aoki’s ledge. it’s found along the medial wall of the joint. It attaches to the lower patella and therefore the lower femur and crosses the suprapatellar plica to insert within the synovium surrounding the infrapatellar fat pad. Its free border can have different appearances. because the medial plica is attached to the synovium covering the fat pad and ligament patellae, it also changes dimension and orientation during knee movement. The medial plica is thought to be the foremost commonly injured plica because of its anatomical location and it’s usually this plica that is implicated when describing the plica syndrome.
Similar to the suprapatellar plicae, the medial plicae can also be classified by appearance.
Kim and choe have defined the subsequent 6 types:
- Absent No synovial shelf on the medial wall
- Vestigial but 1 mm of synovial elevation which disappears with external pressure
- Shelf an entire fold with a pointy free margin.
- Reduplicated Two or more shelves running parallel. they’ll be of differing sizes.
- Fenestra The shelf contains a central defect
- High-Riding A shelf-like structure running anterior to the posterior aspect of the patella, during a position where I couldn’t touch the femur.
Each type is subdivided per size and regard to femoral condyle with flexion and extension of the knee into:
- A—Narrow non-touch which never makes contact with the femoral condyle.
- B—Medium touch which touches condyle with knee movement.
- C—Wide covering which covers the femoral condyle.
Infrapatellar plica
The infrapatellar plica is also known as ligament mucosum, plica synovial infrapatellar, inferior plica, or anterior plica. it’s a fold of synovium which originates from a narrow base within the intercondylar notch, extends distally before the anterior cruciate ligament (ACL), and inserts into the inferior of the infrapatellar fat pad. mostly it appears as a skinny,cord-like, fibrous band that resembles ACL that it becomes difficult to differentiate them. The infrapatellar plica is taken into account to be the foremost common plica within the human knee. Discussion is ongoing on whether this plica is structurally important to regular knee movement or whether it’s redundant.
A classification for infrapatellar plicae is as follows:
- Absent which means No synovial fold between the condyles of the femur.
- Separated an entire synovial fold which was cut loose the anterior cruciate ligament (ACL).
- Split Synovial fold that’s become independent from the ACL but is additionally divided into two or more cords.
- The vertical septum is a whole synovial fold that is attached to the ACL and divided the joint into medial and lateral compartments.
- Fenestra – is a vertical septum pattern that contains a hole or defect.
Lateral plica
The lateral plica is also known as the plica synovial lateralis or lateral para-patellar plica. it’s longitudinal, thin, and is found 1-2 cm lateral to the patella. it is formed as a synovial fold along the lateral wall which is above the popliteal hiatus, which extends inferiorly and has insertion into the synovium of the infrapatellar fat pad. Some authors doubt whether it’s a real septal remnant from the embryological phase of development or whether it’s derived from the parapatellar adipose synovial fringe.
This type of plica is very rare to find; its incidence is below 1%.
Causes of Plica Syndrome:
Plica syndrome occurs when the synovial folds are irritated and become inflamed. this might flow from direct knee trauma, overuse or repetitive activities, or an underlying knee problem that affects the pliability of the tissue layer.
The knee plica may get caught on the femur or may get trapped or pinched between the knee bones. when this situation occurs the knee plica results in inflamed, gradually thick, and if left untreated turns into a hard structure.
Plica syndrome is often caused by:
- Plica syndrome is commonly caused by repetitive knee bending like on stair climbers
- Direct Trauma: A blow to the knee e.g. a fall on to the knee or an RTA where the knee hits the dashboard
- Repetitive Knee Movements: Activities where you repeatedly bend and straighten the knee are often in charge of knee plica syndrome e.g. running, cycling, rising and down stairs
- Sudden Increase In Activities: If you rapidly increase your exercise levels it can result in overloading of the synovial plica and thus they become inflamed
- Knee Injuries: particularly twisting injuries, meniscus tears, or anything that causes bleeding within the genu
- Prolonged Flexion: sitting for long periods or sleeping together with your knee bent often ends in pain with plica synovial
- Underlying Knee Conditions: like osteochondritis dissecans, fat pad irritation, or synovitis
- Muscle Weakness: because the plica are indirectly attached to the quadriceps, weakness within the quads muscles increases the force through the plica resulting in irritation and inflammation
Symptoms of Plica Syndrome:
The symptoms of plica syndrome may result suddenly from an injury or gradually increases from overuse, in one or both knees. Typical symptoms of knee plica syndrome include:
- Knee Pain: Pain from plica syndrome feels dull and achy instead of sharp or stabbing in nature. the situation of the pain will depend upon which plica is inflamed. Pain from plica synovitis is commonly worse at midnight time thanks to the build-up of inflammation
- Worse With Activity: activities where the knee bends and straightens like mounting and down stairs, squatting, and getting into and out of chairs cause pain with plica syndrome
- Clicking or Popping Noises: once you bend and straighten your knee
- Knee Locking: it should desire the knee catches or gets stuck sometimes, typically once you stand up after sitting for a long time
- Instability: People with plica synovial often complain that their knee looks like it’s visiting slip, particularly when walking on slopes or up and down stairs
- Swelling: There could also be localized swelling within the knee plica and/or the encircling area
- Reduced Knee Movement: because the synovial plica thickens, it loses its elasticity which may restrict knee movements.
Diagnosis of Plica Syndrome:
For the diagnosis of Medial Plica Syndrome orthopedic should perform a physical examination and imagining test to confirm the diagnosis.
Examination:
One of the foremost details in diagnosing medial synovial plica pathology is obtaining an appropriate history from the patient.
The pain is commonly described as a dull pain within the proximo-medial aspect of the knee and along the border of the patella. Frequently there’s is an enclosed hydrops and a string palpable. The pain increases with activity, and overuse and is practically bothersome in the dead of night.
Most patients have complaints when doing stairs, squats, and standing up from a chair because these movements create stress on the patellofemoral joint. The patient might also complain of pain following prolonged periods of sitting. About 50% of the patients allow us to know that they need to be doing exercises with repetitive flexion and extension. Injury or overuse of the opposite plica can cause identical complaints but these are seen less frequently.
Specific physical tests for the diagnosis of a medial plica include the plica and therefore the mediopatellar plica stutter tests. Yet, the plica stutter test won’t work when the joint is swollen. Other methods of examination that will indicate the presence of a medial plica include the medial subluxation test, McMurray’s, Appley’s test for instability, and Cabot’s test.
The MPP test is conducted with the patient in the supine position and therefore the knee extended. force is applied manually to the inferomedial part of the patellofemoral joint with the thumb, checking the presence of tenderness. If this tenderness clearly diminishes at 90° of flexion while applying the identical manual force, the test is taken into account positive. compared to arthroscopy, the sensitivity, and specificity of this test were 89.5% and 88.7%, respectively, with a diagnostic accuracy of 89.0%.
Other provocation tests for the diagnosis of medial plica syndrome include the knee extension test or flexion test. For the active extension test, a fast extension of the tibia is performed as if making a kicking movement. The test is taken into account as positive when painful, due to the abrupt tension on the plica from the musculus quadriceps femoris muscle. The flexion test is performed by quickly swinging the tibia from a grip of full extension into flexion and interrupting the swing between 30 and 60° of flexion The test is again positive when painful because the plica is then stretched with eccentric contraction of the quadriceps muscle.
The plica snap test is often wont to verify if there’s irritation of the medial plica. For the palpation of the medial synovial plica, the patient should be in a supine position on the examining table with both legs relaxed. For the medial synovial plica, the examiner palpates the ligament by rolling the fingers over the plica fold, which is found between the medial border of the patella and also the adductor tubercle region of the medial femoral condyle. Under the finger, which rolls directly against the underlying medial femoral condyle, the ligament will happen as a ribbon-like fold of tissue. The test is positive when it reproduces the symptoms like a sensation of mild pain. But also compare it with the conventional knee to work out if there’s a difference in the amount of pain. it’s demonstrated that it is quite painful in some patients because the medial joint and synovium are well innervated.
McMurry’s test:
With the patient supine, the examiner holds the knee and palpates the joint line with one hand, thumb on one side, and fingers on the opposite, whilst the opposite hand holds the only of the foot and acts to support the limb and supply the desired movement through the range. with the knee in maximal flexion, try to extend the knee with internal rotation of the tibia which is a VARUS stress, then return to the end range of flexion position and extend the knee with external rotation of the tibia which is VALGUS stress. The IR of the tibia followed by extension, the examiner can test the complete posterior horn to the center segment of the meniscus. The anterior portion of the meniscus isn’t easily tested because the pressure to it a part of the meniscus isn’t as great.
IR of the tibia + Varus stress = lateral meniscus
ER of the tibia + Valgus stress = medial meniscus
If the test is positive following symptoms may see:
- pain
- snapping
- audible clicking or locking
Appley’s test:
Appley’s grinding test involves placing the patient within the prone position with the knee flexed to 90 degrees. The patient’s thigh then stabilizes on the examining table with the therapist’s knee. the examiner then rotates the tibia medially and laterally while applying distraction, And notices if there is any excessive movement, restriction, or discomfort present. after that therapist performs the same procedure but applies compression instead of a distraction. If rotation plus distraction is more painful or shows increased rotation relative to the traditional side, the lesion is possibly to be ligamentous. If the rotation plus compression is more painful or shows decreased rotation relative to the traditional side, the lesion is presumably to be a meniscus injury.
Imagining test:
Provocation test: A provocation test that simulates conditions that may cause the occurrence of symptoms may be applied. These results are going to be considered positive if the symptoms resulting from the tests are like the symptoms the patient is sometimes experiencing. Yet as similar symptoms may be related to other conditions of the hinge joint, this method won’t give an unambiguous result either.
Radiography is of no diagnostic value to see whether patients suffer from plica syndrome because the radiograph is negative. Yet, radiography may be helpful to rule out other syndromes where the symptoms are common with those of a plica syndrome (see differential diagnosis). If there are symptomatic plicae, it’ll demonstrate hypertrophy and inflammation. this may result in thickening and eventually fibrosis.
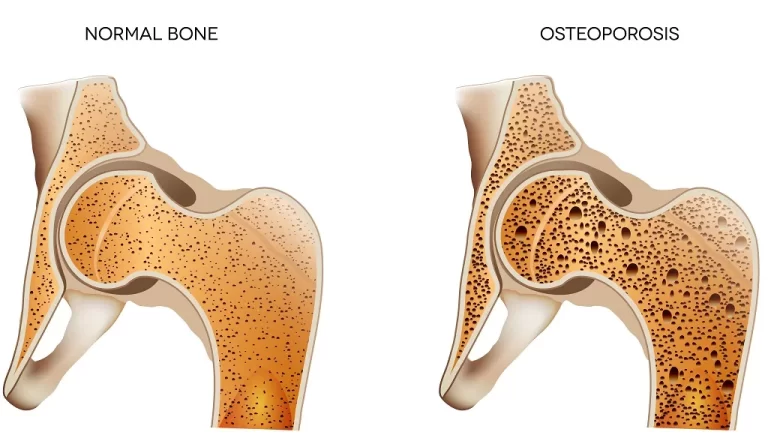
If fibrosis is important, changes within the articular surface and also the subchondral bone may occur.
Arthroscopy is often helpful because plica syndrome is commonly confused with chondromalacia or a medial meniscal tear. Lateral pneumoarthrography and double contrast arthrography are used with varying success. together with CT, it cannot only visualize the plica, but it also demonstrates whether or not impingement is present.
However, currently, it’s gone out of use due to problems to get reproducible and reliable results and also exposure to radiation.
Nowadays, the simplest results are obtained through MRI Scans. Most cases of plica syndrome don’t absolutely require MRI, but it can help to rule out other pathologies that may cause knee pain. An MRI can exclude bone bruises, meniscus tears, ligament injuries, cartilage defects, and OCD lesions,… which will masquerade as plica syndrome. MRI is beneficial to gauge the thickness and extension of synovial plicae and it can even detect a pathologic plica, particularly if an intra-articular effusion is present.
Differential Diagnosis of Medial Plica Syndrome:
- Patellar femoral syndrome
- Patella bipartite
- Patellar maltracking
- Degenerative joint disease
- Hoffa syndrome
- Sinding-Larsen-Johansson disease
- Medial collateral ligament sprain
- Osteochondritis dissecans
- Pes anserinus bursitis
- Meniscal tears
Treatment of Medial Plica Syndrome:
Treatment of Medial Plica Syndrome includes medical treatment, physiotherapy treatment, and surgical treatment.
Medical treatment of Medial Plica Syndrome:
Treatment for knee plica syndrome normally involves a mix of:
Rest: you must rest from aggravating activities like cycling and running to permit the plica synovitis to cool down
Ice: Regularly applying ice packs helps to cut back pain and inflammation
Anti-Inflammatory Medication: NSAIDs like ibuprofen also can help reduce pain and inflammation
Corticosteroid Injections: If pain is stopping you from exercising, your doctor may offer you a steroid injection into the synovial plica to cut back the pain and inflammation in order that you’ll be able to start rehab. Injections mustn’t be utilized in isolation as they only temporarily improve symptoms
Physiotherapy treatment for Medial Plica Syndrome:
Once the acute inflammation is reduced, physiatrics is often initiated, aiming at decreasing compressive forces by stretching exercises and by increasing quadriceps strength and hamstring flexibility.
This treatment is sometimes recommended for the primary 6-8 weeks after the initial examination.
It consists of strengthening and improving the pliability of the muscles adjacent to the knee, like the quadriceps, hamstrings, adductors, abductors, M Gastrocnemius, and M Soleus.
The key components of the program will involve flexibility, cardiovascular condition training, strengthening, and return to ADL.
Supine passive extension exercise while placing the foam roller under the ankle helps to regain flexibility in extension. Gravity will be a helpful factor to stretch the knee in a maximal extension position. Gradually you will be able to perform this exercise while putting weights on the anterior sight of the knee.
Quadriceps sets
Passive knee extension in a prone lying position, while laying on the belly, with foot unsupported and knee supported over the bench.
Straight leg raises
Leg presses
Also, mini-squats, a walking program, the utilization of a recumbent or stationary bicycle, a swimming program, or possibly an elliptical machine are the foremost successful rehabilitation programs.
Rehabilitation programs will have the best success when focussing on strengthening the quadriceps muscles which are directly attached to the medial plica, and when avoiding activities that cause medial plica irritation.
The most important part of the quadriceps to coach is that the m. vastus medial. A full range of quadriceps training isn’t recommended because these create excessive patellar compression at 90°. Besides, straight leg raises and short-arc quadriceps exercises at 5°-10°, also hip adductor strengthening should be performed. Other exercises to be performed are squad, rising and down the steps, and lunging forward. Other important components of this treatment are a stretching program for the muscles named quadriceps, hamstrings, and gastrocnemius and knee extension exercises.
The goal of those knee extension exercises is the strengthening of the tensor musculature of the joint capsule. But if the patient has an excessive amount of pain when reaching terminal extension, then this could be avoided. This conservative treatment is effective in most cases and the patient does not need surgery but in some patients surgery is critical. In this case, post-operative therapy is important. The postoperative treatment is similar to the conservative treatment and is typically started 15 days after the surgery. the most goal of physiotherapy in plica syndrome is to scale back pain, maximize the ROM and increase the strength of the muscles.
- Quadriceps sets:
Quad sets facilitate your build and maintain strength within the muscles on top of your thigh. With this action, you’re “setting” these quadricep muscles by holding them tight. Perform 8 to 12 repetitions many times during the day.
Sit on the ground along with your injured leg straight and get in front of you.
Tighten the muscles on top of your thigh by pressing the rear of your knee flat right down to the ground.
Remain in this position for about 6 seconds, then take a rest for up to 10 seconds.
If you are feeling discomfort under your kneecap, try putting a tiny low towel roll under your knee during this exercise.
2. Prone knee extension:
Performing the prone hang exercise is easy to try and do at home or within the physiotherapy clinic.
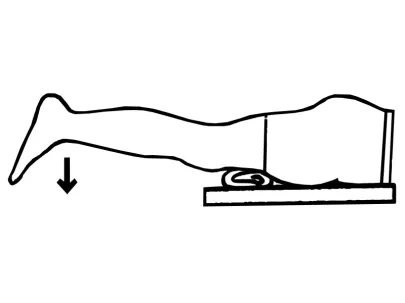
Locate a bed that has a minimum of one side with an ample amount of room around it.
Lie on the bed on your stomach.
Slide down on the bed to the sting so your leg is hanging over the top. Your thigh should be placed on the bed, but your lower leg should be hanging off the bed.
Place a rolled-up towel underneath your thigh just above your kneecap. This helps to stay from placing an excessive amount of pressure on your kneecap.
Hold this position for 30 to 60 seconds. Allow gravity to tug your lower leg down towards the ground so your knee straightens out.
You may feel some discomfort during this position. If you are feeling intense knee pain, stop the exercise and get in touch with your healthcare provider or therapist.

you will find other ways to enhance your knee ROM.
You can repeat this same exercise for 5 to 10 repetitions. Simply bend your knee to require some pressure off of your leg, so return to the straight knee position another time. If you’ve got difficulty bending your knee, you’ll have an addict or loved one gently bend it for you.
Sometimes assistance of gravity alone isn’t enough to totally straighten your knee. If this is often the case, you’ll place a 1 or two-pound cuff weight around your lower leg or ankle to feature a small amount of force to the exercise. Use caution; an excessive amount of weight could over-stress your knee. Add merely enough weight to make a mild stretching feeling. Your PT can facilitate your determining the correct amount of weight to feature.
After performing the prone hang exercise, your knee is also a bit sore. This soreness is natural since you’re stretching tissues around your knee. Applying an ice pack to your knee for 10 to fifteen minutes may help alleviate a number of this soreness. Again, if you are feeling pain in your knee, immediately contact your healthcare provider or physiotherapist.
The prone hang exercise is often performed several times every day to figure on improving your knee extension ROM. it’s an easy yet effective method to assist get your knee straight to enhance your overall function associated with walking, sitting and standing, and navigating stairs.
3. Straight leg raise:
How to do it:

Lie on your back together with your hips square and your legs laid out comfortably on the bottom.
Bend the knee of your non-injured leg at a 90-degree angle, planting the foot flatly on the bottom.
Stabilize the muscles of your affected leg by contracting your quadriceps (the group of muscles on the front of your thigh).
Inhaling slowly, lift the straight leg six inches or to the extent of your unaffected leg off the underside.
Hold for 3 seconds.
Exhaling slowly, lower the leg to the bottom with control.
Relax and repeat 10 times more.
When done correctly, you’ll feel the strain in your hip, thigh, and abdomen throughout the movement
- Heel press:

Lay on a bed with a pillow under the heel. try and put the pressure on the pillow along with your heel, and hold this position for 10 seconds. repeat the identical procedure 10 to twenty times.
- Mini squats:

Instructions:
The feet and shoulder should be slightly apart and holding onto something for balance
Perform a mini squat to place pressure on the quads
Holding at the identical knee angle, ensure you’ve got even pressure through the feet
Keep holding whilst maintaining a solid body position
Hold for an allocated time and knee angle
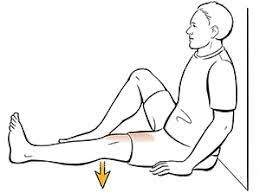
- Hamstring stretch:
How to do it:

- In the sitting position, rest your heel on the bottom together with your knee straight.
- Gently lean forward until you feel a stretch behind your knee and thigh keep your knee straight.
- Why it helps: This stretch is usually useful to boost knee extension if it’s limited.
- Standing calf stretch:
How to do it:
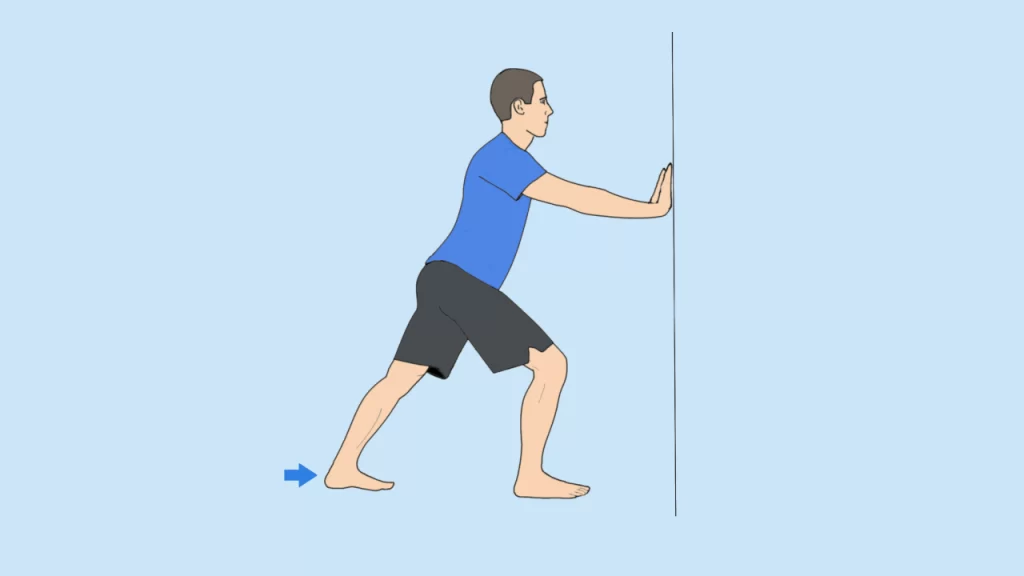
- Start by standing near a wall.
- Step forward with one foot and keep both feet facing toward the wall.
- Keep the knee of your back leg straight.
- Bring your body forward toward the wall and support yourself together with your on-the-wall arms as you Permit your front knee to bend until you’re feeling fragile by the rear of your straight leg.
- Move closer or farther off from the wall to manage the stretch of the rear leg.
- Why it helps: after you’ve got a Baker’s cyst, the backside of the leg is going to be tight. This stretch will help release a variety of strains within the lower leg.
- Side-stepping:
How to do it:
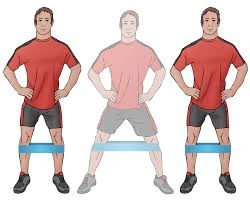
Begin with or without a resistance band around your ankles and your knees should be slightly bent.
Keep your weight on your heels as you slowly take a get out to the side and permit the other leg to follow without losing tension within the band.
Why it helps: This exercise helps in strengthening the gluteal muscles, which helps stabilize your hip and knee.
- Toe raise:
How to do seated toe raises
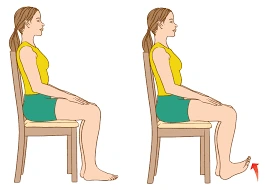
Start seated together with your feet flat on the ground. Rest your hands on your lap or the perimeters of your chair.
Lift your toes on your right foot, keeping the left foot planted firmly on the bottom.
Hold for 3 to five seconds.
Lower your toes.
Repeat 10 to fifteen times on each foot for a complete of three sets.
To ease into this exercise, you’ll start by lifting only your toes, and flexing the ball of your foot. Once you are feeling comfortable, you’ll try a full toe raise, which involves lifting your foot so only your heel stays on the bottom.
How to do standing toe raises
For standing toe raises, find an area that you simply can stand on securely. that may be:
- on the ground
- on a step together with your toes hanging out over the sting
- on an incline together with your toes less than your heels
- From there, lift and lower, following the identical steps from the seated toe raise.
- Heel raise:
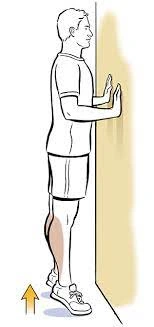
Place your one or both hands on a supportive surface for balance.
Stand with equal weight on both feet.
Raise both heels.
Lower both heels simultaneously in a controlled manner.
Gradually build to 3 sets of 15 repetitions.
Allow a minimum of a 2-minute rest between sets.
At the top of all of your sets and reps, follow up with a calf and soleus stretch.
11. Lunges:
Start in a very standing position along with your feet hip-width apart.
Step forward longer than a walking stride so one leg is sooner than your torso and also the other is behind. Your foot should land flat and remain flat while it’s on the bottom. Your rear heel will rise off of the bottom.
Bend your both knees to approximately 90 degrees as you lower yourself. Remember to stay your trunk upright and core engaged.
Then, forcefully push from your front leg to return to the starting position.

Points to remember:
Your lead knee shouldn’t go past your toes as you lower toward the bottom.
Your rear knee shouldn’t touch the bottom.
Aim to stay your hips symmetrical (at the identical height, without dropping the hip of your back leg or hiking the hip of your front leg).
Contract your abdominals during the movement to assist keep your trunk upright.
Your feet should stay at a distance of hip-width apart during the landing and return.
Surgical management of Medial plica syndrome:
It is rare that patients need arthroscopic surgery to treat isolated medial plica pathology because the medial plica may be a part of the joint lining and resection of it’ll lead to the joint lining growing back. Since the body heals back this sort of resection with a scar, the tissue may heal back with a painful scar and therefore the patient may have more symptoms.
Since the treatment of a painful plica after an arthroscopic resection can often cause patients to own more pain than they did before the arthroscopic resection, it’s important to create sure that a patient has the pathology of this area that isn’t alert to an exercise program, and possibly injections, before consideration of resection of this tissue. it’s important to acknowledge that surgery for an irritated plica is rare, and historically it comprised only 2–5% of all arthroscopic surgery at a time when resonance imaging scans weren’t commonly used and more surgeries were performed for diagnostic reasons. we’ve got found that arthroscopic resections of irritated plicas are rarely performed today.
the same old instances where one may have some the benefit of resection of a medial synovial plica could also be where the plica is acting as a shelf which is catching over the medial femoral condyle and causing some erosion of the articular cartilage during this area. In these circumstances, patients may have good pain relief and decreased catching sensations in their knee after arthroscopic resection of their medial plica. during this instance, it’s usually not recommended to divide the pathologic plica and resect it totally because the pathologic plica may grow back, and also the patient may have a recurrence of their symptoms.
it’s also been noted that the results of arthroscopic plica excision are more successful in adolescents than in older patients. Indirect treatment of the medial plica irritation can also be very beneficial to patients. In these conditions, the pathology is deep within the knee. Treatment of some conditions like localized areas of arthritis, meniscal tears, or other knee pathologies, may help to decrease the pain and swelling of the knee which leads to secondary irritation of the medial plica. In these situations, it is beneficial for the patient to perform surgery for the treatment of the secondary reason behind plica irritation. In these circumstances, it’s not recommended to resect the medial synovial plica, because there’s a really good chance that it’ll retrieve with an exercise program after surgery and patients might not have pain relief from their plica irritation if it’s resected arthroscopically.
Complication after the surgery:
Like any other surgery, complications can occur after arthroscopic resection. These may include:
Infection.
Artery damage.
Nerve damage.
Blood clots.
Excessive bleeding.
A hypersensitivity to anesthesia.
Numbness at the incision sites.
To reduce your risk of post-surgical complications, see your healthcare provider about your anamnesis. you should also tell them about any medications or supplements you’re currently consuming.
How much time does it take to recover from arthroscopic resection surgery?
After arthroscopic resection surgery, the majority need about six weeks to recover. Healing could take longer reckoning on the severity of your condition.
Prevention:
Though you can’t prevent plica syndrome altogether, there are many kinds of stuff you can do to cut back your risk. For example:
- Avoid overuse of your ginglymoid joint.
- Before starting your new exercise routine you should know your body limits.
- Try to maintain strength and mobility in your legs, ankles, and feet.