Pes Anserine Bursitis
Table of Contents
What is the meaning of pes anserine bursitis?
Pes Anserine Bursitis is a swelling of the bursa which is located between the tibia and the tendons of the hamstring muscle at the inside of the knee. It happens when the bursa becomes irritated and produces too much fluid, which causes it to inflame and put pressure on the nearer parts of the knee.
Definition:
it occurs when the bursa — or fluid-filled sac which is inside your knee joint becomes irritated and produces too much fluid.
Relevant anatomy:
The Pes Anserine bursa may be a fluid-filled vesicle. It secretes synovia so as to cut back friction between tissues, and also works as a cushion for bones, tendons, and muscles. The inflammation of the bursa doesn’t appear suddenly, but rather progresses over a period of your time. Bursitis may occur within the shoulder, knee, hip, elbow, and massive toe.
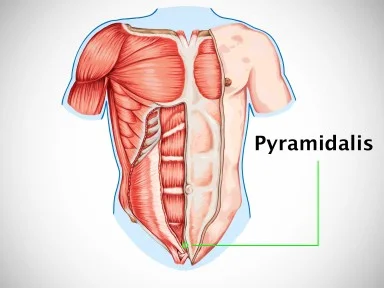
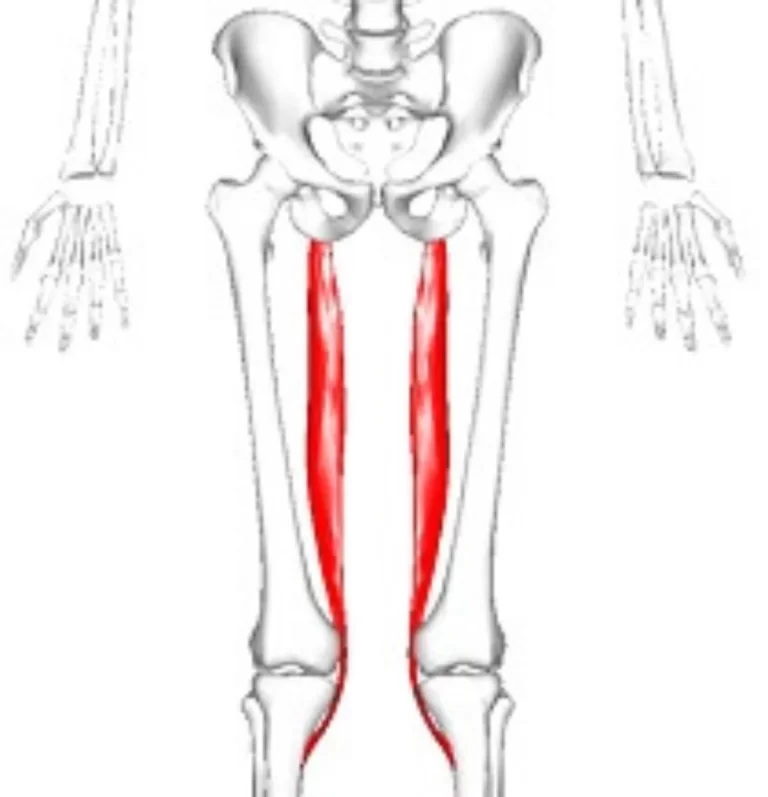
The Pes Anserine is also known as a”Gross foot”. It is the insertion of three muscles they are Semitendinosus, Sartorius, and Gracilis. It is located medially. The three tendons of the Pes Anserine are located superficial to the medial collateral ligament of the knee. The calf muscles are adductors of the leg. they help to pull the leg towards the median axis of the body. The semitendinosus muscle is a component of the hamstrings muscle group located at the rear of your upper leg. these three muscles (semitendinosus, and calf muscles) are primarily flexors of the knee and internal rotators.
Causes:
Pes Anserine bursitis often occurs when the muscle related to the pes anserine bursa is repeatedly used, by doing movements like flexion and adduction. This movement causes friction within the bursa and also increases pressure on the bursa. Bursitis can also occur by direct trauma, for example, a right away hit within the Pes Anserine region. A contusion to the current area leads to an increased release of secretion within the lining of the bursa. Then there is an inflammation in the bursa which is tender or painful and underlying Osteoarthritis of the knee.
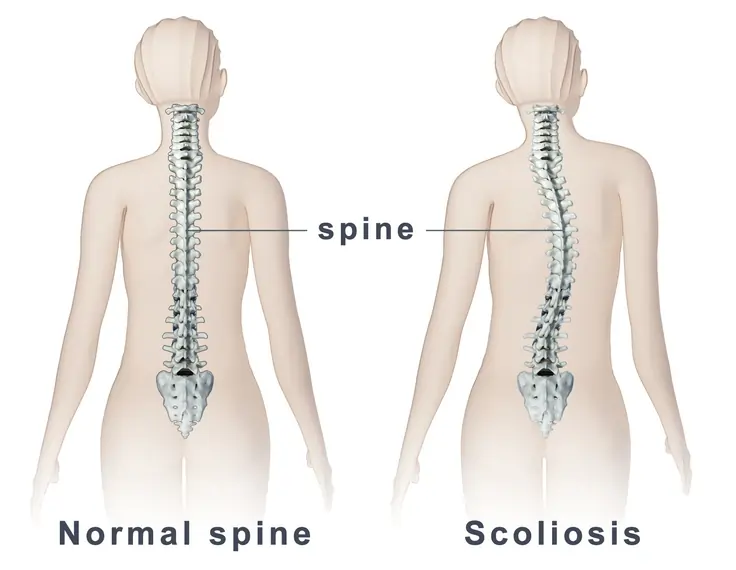
According to reports, anserine bursitis is more common in obese middle-aged females. The fact can explain that girls have a wider pelvis, leading to angulation of the knee within the frontal plane which leads to higher pressure on the bursa which increases the chances of pes anserine bursitis.
We can say that an inflamed bursa isn’t a primary pathology, but rather a consequence of an earlier complication.
Bursitis usually develops because of the results of overuse or constant friction and stress on the bursa. Pes anserine bursitis is common in sports people, particularly runners. reports suggest that people suffering from osteoarthritis of the knee have a chance of developing pes anserine bursitis.
Several factors can contribute to the event of pes anserine bursitis, including:
- Incorrect training techniques, like neglecting to stretch, doing excessive hill running, and sudden increases in mileage
- Tight hamstring muscles
- Being duck-footed or having knocked knees
- Osteoarthritis within the knee
- Sports like tennis or soccer require repetitive knee movements.
- Abnormal knee alignment (valgus).
- Being overweight.
- Overuse of the knee.
- Improper training techniques, like failing to warm up before working out.
- A person who is already suffering from MCL(medial collateral ligament)injury
Symptoms of Pes Anserine Bursitis:
Pes Anserine bursitis causes pain within the knee (mostly during running or taking stairs). The patient may suffer from spontaneous anteromedial knee pain while climbing or descending stairs and will also feel tenderness in the pes anserine region. As well, the region around the bursa is swollen or tender to the touch.
Other symptoms may include:
- Decreased muscle strength
- Gait deviations
- Decreased function
- Decreased ROM
- Postural dysfunction/impaired lower extremity biomechanics
- factors that increase the episodes of pain include activities that need movements like flexion and end rotation, in addition to exhortation and adduction. Pivoting, kicking, squatting, or quick movements from side to side, like within the sports mentioned above, may cause further irritation.
Diagnostic Procedures:
Lateral x-ray views of the patient’s knee are very useful for ruling out a fatigue fracture, arthritis, or maybe Osteochondritis Dissecans. An MRI is required to clarify damage caused to other regions of the medial side of the knee. Many times MRI findings help in correct diagnosis which can prevent arthroscopy. for accurate diagnosis MRI findings should be compared with those of physical symptoms. when other imaging modalities like MRI and CT fail to do proper diagnosis then Sinography (radiography of a sinus following the injection of a radiopaque medium) can be helpful, it,s a very reliable diagnostic source. A Lidocaine/Corticosteroid injection within the area of the bursa is able to help determine the contribution of this pathology to the patient’s overall knee pain.
Examination:
The pes anserine bursa is often palpated at some extent slightly distal to the tibial tubercle and about 3-4 cm medial thereto (about 2 fingerbreadths).
Examine hamstring length with the patient within the supine position. Bend the patient’s hip 90° and so extend the knee as far as possible. How far the knee will be extended will indicate hamstring length and tightness. If the patient’s knee is straightened completely then the hamstrings don’t seem to be tight.
With the sports-related variant of pes anserine bursitis, symptoms are also reproduced by means of resisted internal rotation and resisted flexion of the knee. With the chronic variant in older adults, flexion or extension of the knee usually doesn’t elicit pain.
outcome measures:
Lower extremity functional scale(LEFS):
Background
The lower extremity functional scale (LEFS) may be a valid patient-rated outcome measure (PROM) for the measurement of lower extremity function. it absolutely was first developed by Binkley et al. (1999) in a very group of patients with various musculoskeletal conditions. the size is originally developed in the English language and in step with civilization.
Objective
The objective of the Lower Extremity Functional Scale (LEFS) is to live “patients’ initial function, ongoing progress, and outcome” for a large range of lower-extremity
conditions.
Lower Extremity Functional Scale.png
Intended Population
The LEFS is meant to be used with adults, with lower extremity conditions.
Method of Use
The LEFS could be a self-report questionnaire. Patients answer the question “Today, does one or would you have got any difficulty in the slightest degree with:” with reference to twenty different everyday activities.
Patients select a solution from the subsequent scale for every activity listed:
Extreme Difficulty or Unable to Perform Activity
Quite a little bit of Difficulty
Moderate Difficulty
A Little little bit of Difficulty
No Difficulty
The patient’s score is tallied on the underside of the page. the most possible score is 80 points, indicating very high function. The minimum possible score of this test is 0 points, which indicates very low function. if the patient scores 0 then the patient has a very low function.
Reliability
Internal reliability for the LEFS is superb (a=0.96). Test-retest reliability estimates were R=.86 (95% lower limit CI=.80) for the whole sample (n=98) and R=.94 (95% lower limit CI=.89) for the subset of patients with more chronic conditions (n=31).
Validity
The LEFS may be a valid tool as compared to the SF-36
Responsiveness
if the change is over 9 points so it presents a real change in the patient’s current condition, so the minimal detectable change in LEFS is 9 points.
The minimal important difference (MCID) for the LEFS is 9 points.
The capacity of the LEFS to detect a change in lower-extremity function appears to be superior to it of the SF-36 physical function subscale, as indicated by higher correlations with an external prognostic rating of change.
Miscellaneous
The LEFS has a mistake of +/- 5 points.
Adaptation in numerous countries
LEFS has been translated and used in several countries like, Italian, French, Dutch, Arabic, Brazilian Portuguese, Malaysian, Finnish, Persian, Turkish, Taiwan, Chinese and Dutch translated and adapted versions have also been tested for validity and reliability.
Differential Diagnosis
Pes Anserine bursitis is commonly confused with other causes of medial knee pain:
Stress fracture of the shin bone on the proximal side will cause pain within the area of the Pes Anserine.
Patellofemoral syndrome
Medial meniscus lesion and osteoarthritis: Pain and sensitivity would be present within the medial compartment, while within the pes anserinus bursitis they’re located inferomedial to the medial joint interline. Stress maneuvers of the medial collateral ligament, which are present with or without instability, may often contribute to the diagnosis of lesions of the medial collateral ligament.
Knee pain secondary to L3-L4 radiculopathy is related to lumbago without pain on digital pressure of the anserine region.
Panniculitis occurs in obese individuals and causes painful inflammation of subcutaneous fat at midnight.
injury while running often results in semimembranosus tendinitis.
pain and tenderness on the medial side of the knee are sometimes caused by medial plica syndrome.
Extra-articular cystic lesions which are for examplesynovial cyst, ganglionic cyst, parameniscal cyst, pigmented villonodular synovitis, and synovial sarcoma.
Other than the conditions which are listed above some conditions also have differential diagnoses as pes anserine bursitis which includes:
Atypical medial meniscal cysts
Juxta-articular bone cysts
Semimembranosus bursitis
Tibial collateral ligament bursitis
Medical treatment for Pes Anserine Bursitis:
The initial treatment of pes anserinus bursitis should include the rest of the affected knee and non-steroidal anti-inflammatory drugs (NSAID). Additional modalities, including local injection of a corticoid like methylprednisolone, are indicated in a few cases. injection of local anesthetics, corticosteroids, or both combined can be given as the second line of the treatment.
When the conservative treatment fails orthopedics suggests surgery.in some cases, symptoms can be improved by a simple incision or drainage of the bursa. The bursa is also removed if chronic infection can’t be cleared up with antibiotics. After surgery, if the bursa is removed, follow the identical steps of rehabilitation and recovery outlined under physiatrics management. in the case of infection when standard antibiotics can not work properly a surgical decompression of the bursa can be performed.
Home Remedies
RICE Therapy (Rest, Ice, Compression, Elevation) – When it involves handling pain within the knee, the primary step is often the same: Rest. This also applies when it involves pes anserine bursitis. it’s important to avoid further strain by allowing your body to rest and avoiding excessive strain on the knee. try and avoid activities that trigger pain. cold therapy with an ice pack or towel wrapped around the ice for 20 minutes in the painful area of the knee also helps in relieving pain.
Weight Management – Maintaining a healthy weight can make sure that excessive strain isn’t placed on your knee.
Wear a brace – you’ll speed up your healing process and forestall further injury once you retreat to running with the Bauerfeind Sports Knee Support. This knee support stabilizes the ginglymoid joint and relieves pain while offering comfort and adaptability.
Physiotherapy Treatment of Pes Anserine Bursitis:
Exercise is crucial to assist heal most injuries. When it involves pes anserine bursitis, strengthening and stretching exercises can reduce your pain, improve function, and most significantly, prevent the injury from happening again.
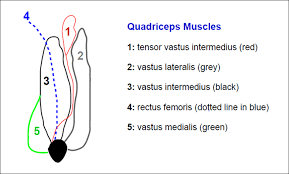
Strengthening exercises may specialize in the muscles surrounding the knees and hips. Improper movement patterns or weakness of those muscles may cause injury, including bursitis. The quadriceps, hamstrings, and glutes, are the foremost muscles that are worked on in a very pes anserine bursitis rehab exercise program.
The hamstring muscles are frequently targeted for stretching exercises since they’re located on the rear of your thigh, and help to bend the knee. When the hamstrings become tight, they’ll pull on surrounding structures, resulting in injury and pain. so this is the reason that hamstring stretches are very important and helpful in any pes anserine bursitis rehabilitation program.
Some exercises may include leg stretching exercises like a hamstring stretch, standing calf stretch, standing quadriceps stretch, hip adductor stretch, heel slide, quadriceps isometrics, and hamstrings isometrics. Progression of those exercises may involve closed-kinetic chain exercises like single-knee dips, squats, and leg presses. Resisted leg pulls using elastic tubing are included.
The closed-kinetic chain exercises also are a recommended method to stop the event of collateral knee instability, which occurs to be a risk factor for Pes Anserine bursitis.
Hamstring stretch:
Lie on your back and convey one leg straight up. It stretches the hamstring muscle and helps to decrease contractions.

The ultimate goal of this posture is to bring your leg up high enough that you can touch your toes. With repetition, you’ll be ready to bring your straight leg towards your head.
Standing hamstring stretch
Extend one leg out by placing the heel on a rather raised surface, like a stair or curb. Keeping the spine straight, bend at the hip and bring the chest toward the thigh. the opposite leg that’s not being stretched also will bend slightly at the knee. Hold this stretch for 10 to 30 seconds.

Standing calf stretch:
Toes on Wall Stretch
Keep your front heel firmly locked into the ground here to actually make the foremost of this calf stretch—and take care to wear sneakers so you’ll be able to maintain an edge on the wall!
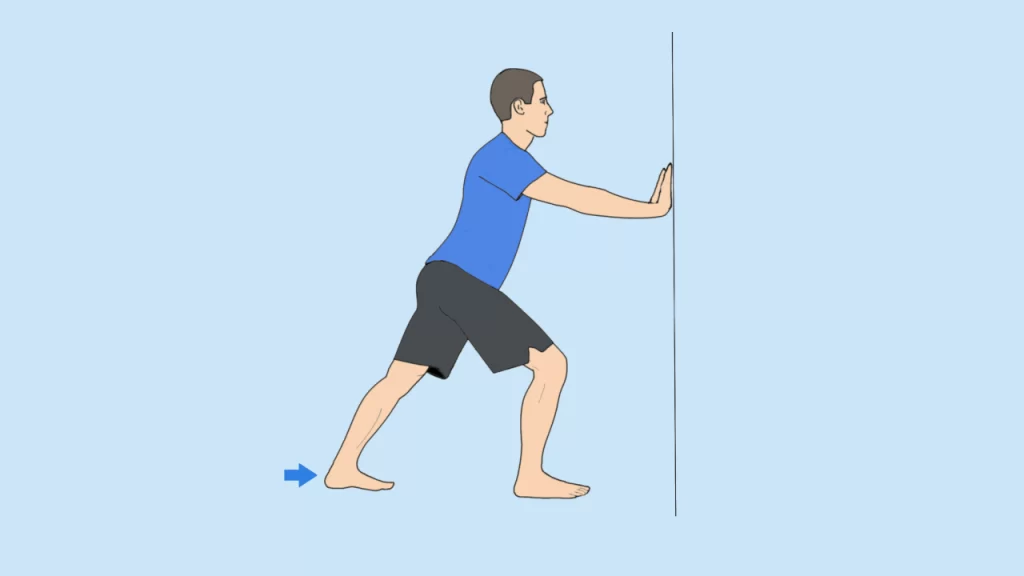
Stand with an enclosed front of you in an exceedingly staggered stance, one foot near the wall and one a couple of feet back. Place your palms on the wall for support.
Bring your front foot near the wall, putting your hell on the ground and your toes up against the wall. Put your weight into your front foot so you’ll feel the stretch in the lower part of your front leg. (To intensify the stretch, you’ll be able to rise on the toes of your back foot and convey your chest closer to the wall.)
Hold for a collection amount of your time, then switch sides and repeat.
Stand facing a pair of feet off from a wall. If you’re not near a wall, you’ll be able to also just do that along with your hands on your hips (pictured above).
Place your hands on the wall for support and the first step foot back to a mini lunge, bending your front leg and keeping your back leg straight.
Lean into the wall and press your back heel down so it’s flat on the bottom. The further apart your feet are, the deeper the stretch is going to be.
Once you’ve held this stretch, change the angle of your foot positioning, suggests Otey—you’ll probably find that different parts of your calf feel tighter than others, counting on your movement patterns, the shoes you wear, and your lifestyle.
Repeat on the opposite side.
Standing quadriceps stretch:
Stand on your one leg, one knee touching the other knee. hold a chair or the wall for balance if needed.
Grab your right foot, using your manus, and pull it towards your butt. take care to push your chest up and hips forward. Try to not worry about pushing your foot too near your backside; your focus should air feeling the stretch in your quad muscle and pushing your hips forward to induce an honest hip flexor stretch. Hold this position for 20 to 30 seconds, then repeat the same procedure on another leg.

Hip adductor stretch:
Standing Side Lunge
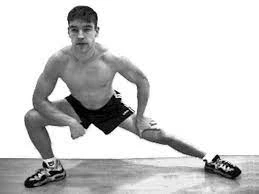
Instructions:
Start from a standing position.
Have your feet wide apart.
Keep your feet facing forwards.
Lunge towards the side as far as you’ll be able to go.
Aim to feel a stretch within the groin.
Hold for 30 seconds.
Repeat on the opposite side.
Butterfly Stretch

Instructions:
Sit down on the ground.
Rest your back against a wall.
Bring the underside of your feet together ahead of you.
Use your hands to tug your feet as near you as possible.
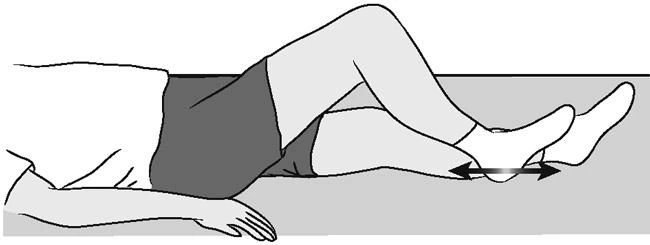
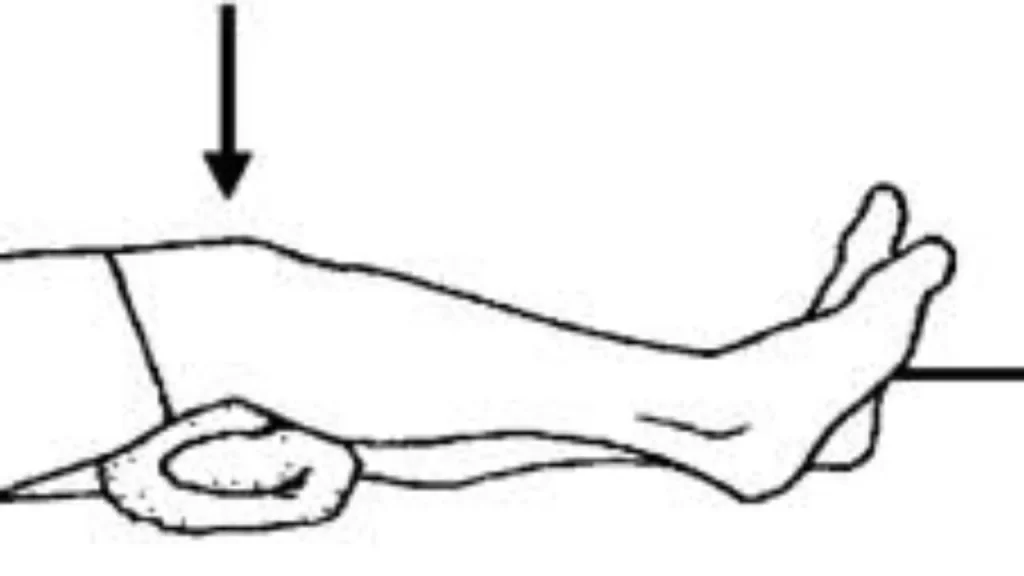
Heel slide exercise:
For this exercise, you have to lie straight on a bed or plinth and with your leg straight for the initial position. then you have to slide your heels towards the buttocks while bending your knees.
Try to touch the buttocks with heels.
Once you reach up to maximum knee bending then hold this position for 5 to 7 seconds, then slowly straighten your knee while sliding your heels to fully extend the knee.
Quadriceps isometrics:
Patients lay in a very supine position with a rolled-up towel or sponge ball under the knee. They were instructed to maximally activate their thigh muscles so as to straighten their knee and hold the contraction for five seconds.
Isometric hamstring exercise:
Lay on a bed with a pillow under the heel. try to put the pressure on the pillow together with your heel, and hold this position for 10 seconds. repeat the identical procedure 10 to twenty times.

Squats:
Start standing with feet wider than shoulders, toes clad so inner thighs point forward.
Clasp hands ahead of the chest.
Tuck pelvis, keep head over hips, and bend knees to sink into a squat, lowering until thighs are parallel to the ground.
Return to start out.
That’s one rep. Perform 15 reps, then continue on to your next move, resting PRN. After you’ve finished all of your exercises (three total), repeat the whole workout twice more for the completion of three rounds.

Surgical management:
In rare cases, if the pain fails to settle with the above treatments your doctor may advise surgery to get rid of the pes anserinus bursa. You normally go back the identical day and will have to use crutches for the primary few weeks. usually, it takes around four to five weeks for the patient to return to their normal lifestyle.
When the pain gradually decreases patient will be able to start performing his/her normal activities, rehabilitation program should start with non-weight bearing exercises like cycling and swimming. If you wish to return to running, start with short distances alternating between running and walking, and gradually increase. a decent rule to follow is the 10% rule where you increase your training by a maximum of 10% every week, be that distance or time.
Remember, you won’t always notice pain once you do an activity, often the pain will come on later that day or the subsequent, so allow yourself adequate rest. If at any point you begin noticing the pain again, that’s your body’s way of telling you you’re overdoing it, so reduce your training until it’s pain-free.
It usually takes two to 3 months for the symptoms of pes anserinus bursitis to completely settle by which era you ought to be able to return to your usual activities.
Recovery Time For Pes Anserine Bursitis:
Typically, pes anserine bursitis will heal within 6-8 weeks or sooner, counting on its severity, adequate treatment, or rest. Typically, it’s best to prevent all activities that involve the knee until the injury has fully healed, and therefore the bursa is no longer inflamed. Failure to try and do so may lead to an extended recovery period, or perhaps other injuries. In other words, there aren’t any shortcuts when it involves recovery and healing.
Taking care of your body may be a gradual process, but if you’re patient and diligent along with your exercises, you’ll see longer-lasting positive effects and changes in your body.