Oculopharyngeal Muscular Dystrophy: Cause, Symptoms, Exercise
Table of Contents
What is oculopharyngeal muscular dystrophy?
Oculopharyngeal muscular dystrophy (OPMD) is a rare genetic muscle condition with onset during adulthood most often between 40 and 60 years of age, which is characterized by slowly progressive muscle disease means myopathy affecting the muscles of the upper eyelids and the part of the throat called the pharynx.
Affected individuals may develop drooping of the eyelids that is ptosis, trouble moving their eyes called ophthalmoplegia, and/or difficulty swallowing means dysphagia and talking. Double vision known as diplopia is uncommon.
Symptoms
The condition usually involves the muscles of the upper eyelids and throat. You may first notice drooping eyelids, a condition known as ptosis, which gradually leads to tipping the head backward to see properly, along with that they tend to choke frequently and have trouble swallowing called dysphagia. Mostly, OPMD gets worse very slowly.
Common symptoms include:
- Eyelid drooping.
- Choking or swallowing problems are called dysphagia. Dry foods may be the first to cause difficulty.
- limitation of upward gaze
- Tongue shrinking with weakness
- wet voice due to pooling saliva
- Facial muscle weakness
- Proximal leg and arm weakness
In the autosomal dominant form of OPMD which is inherited from one parent, initial symptoms typically occur between 43 to 60 years of age whereas, In the recessive form of OPMD which is inherited from both parents, initial symptoms typically occur after age 60.
Causes
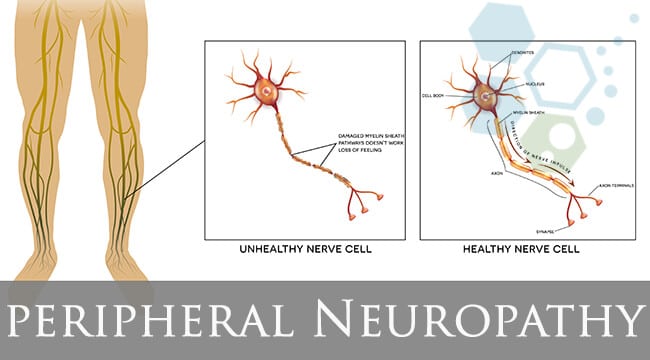
OPMD is mainly caused by a genetic problem in the body. The problem is in a gene that has the information regarded to make a protein namely polyadenylate-binding protein (PABPN1). This defect leads to the production of a nonfunctional protein of PABPN1 in the muscle cells. The PABPN1 clumps inside the muscle cells causing the cells to die, which leads to muscle weakness in the body.
The defective gene that causes OPMD is passed down from a parent to their child, which affects men and women equally. Mostly, a person with the condition has only one copy of the gene problem. Rarely, a person can get two copies of the gene, one from each parent, which leads to more severe OPMD and the condition will get worse more quickly.
OPMD is more common in:
- Hispanic people living in northern New Mexico
- Ashkenazi Jewish people
- People of French-Canadian descent
Diagnosis
The doctor will take your detailed health history, and ask about your recent symptoms, past health conditions, and family health history. The doctor will do a thorough physical examination or clinical evaluation, including checking the muscles around your eyes.
Your available test may include:
- DNA tests or blood tests to look for gene defects (i.e., mutation of the PABPN1 gene)
- Timed swallowing tests to identify the presence of dysphagia (inability to drink 80cc of cold water in less than 8 seconds)
- Video studies of swallowing
- Presence of ptosis or previous corrected surgery for ptosis, in that one or both palpebral fissures smaller than or equal to 8mm, the average is 10 mm vertically.
- Nerve conduction studies and electromyography (EMG)
- Imaging with magnetic resonance imaging (MRI) may play a significant role in identifying fatty degeneration of extraocular muscles, however, it may be both a non-specific and late radiologic feature
- Muscle biopsy to look for OPMD PABPN1 clumps. This is often not needed if the genetic tests are clear.
- Blood tests to help rule out other conditions
Indications for DNA testing of the symptomatic individuals are:
- Evaluation of the size of the mutation as a possible indicator of condition severity
- To confirm the diagnosis in a family never tested
- To confirm a clinical picture that presents a diagnostic dilemma
- To confirm those who may suffer from recessive OPMD
- To evaluate a compound heterozygote status in a patient with a severe earlier-onset form
Oculopharyngeal muscular dystrophy treatment
The treatment of OPMD is mainly focused on the specific symptoms that are seen in each person with this condition.
Ptosis may be treated cautiously with plastic surgery on the eyelids which is known as blepharoptosis repair. The aim of surgery is to raise the eyelids above the visual axis so that, the patient can see. The patient may not be able to completely close their eyelids after surgery, due to the muscles, which are close to the eyelids being weak.
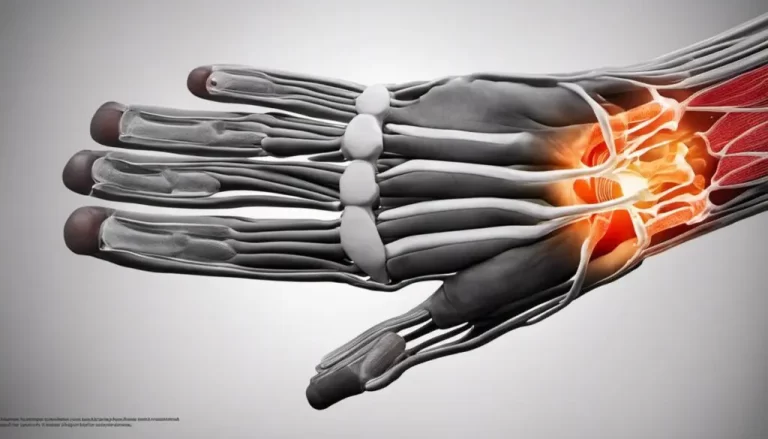
In some cases Changing the texture material of foods may make the patient easier to swallow. If difficulty in swallowing means dysphagia is severe, a surgical procedure known as cricopharyngeal myotomy may be used. In this type of procedure, the cricopharyngeal muscle of the throat is cut, and through this swallowing occurs. The muscle remains relaxed allowing the passage of food or liquid. Sometimes, a feeding tube can be placed directly into the small intestine to bypass swallowing. A doctor widens the muscle with a dilating tool by injecting botulinum toxin into the muscle for relaxation.
Orthopedic devices like leg braces, canes, or walkers can help patients who have difficulty walking.
Genetic counseling is beneficial for affected individuals and their families.
Physiotherapy and occupational therapy help in strengthening and stretching muscles along with maintaining function and range of motion (ROM).
Speech therapy is useful for those who have problems swallowing.
Corticosteroids, such as deflazacort and prednisone may slow disease progression
Heart assist devices, like pacemakers which treat heart rhythm problems and heart failure
Respiratory care, like respirators and cough-assist devices
Medical devices, for example, walkers and wheelchairs, can improve mobility and prevent falls.



What exercises can I do to improve my movement and muscles of OPMD?