Williams syndrome
Williams syndrome is a rare neurodevelopmental genetic disorder that features mild learning or developmental challenges, a high levels of calcium in the blood and urine, and a markedly outgoing personality.
Williams Syndrome (WS) is a genetic condition that is present at birth and can affect anyone. It is characterized by medical problems, including cardiovascular disease, developmental delays, and learning challenges. These often occur side by side with striking verbal abilities, highly social personalities, and an affinity for music.
WS occurs equally in males and females and in all cultures worldwide. The following resources will provide details about the many facets of Williams syndrome
Williams-Beuren syndrome (WBS) is a multisystem disorder with an incidence of 1 in 20,000 births and is caused by a microdeletion on chromosome 7, resulting in the loss of 26–28 genes.
Table of Contents
Other common names for William’s Syndrome
- Williams-Beuren Syndrome
- Beuren Syndrome
- Elfin Facies Syndrome
- Elfin Facies with hypercalcemia
- Hypercalcemia-Supravalvar Aortic Stenosis
- Infantile hypercalcemia
- Supravalvar aortic stenosis syndrome
- WBS
- WS
- WMS
cause and features :
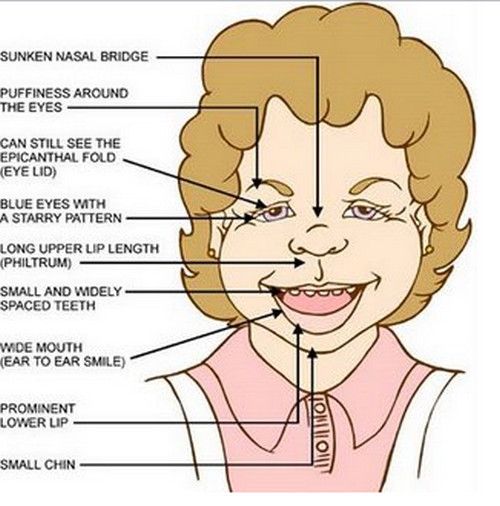
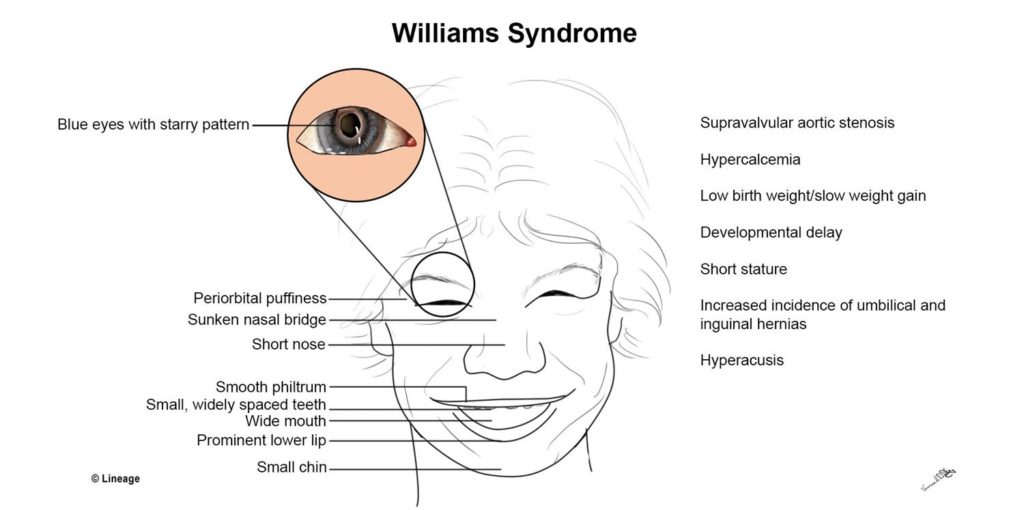
Facial characteristics include a small, upturned nose, long upper lip length, wide mouth, small chin, puffiness around the eyes, and full lips.
A white, lacy pattern may develop around the iris. Adults may have a long face and neck.
Heart and blood vessel problems can mean a narrowing of the blood vessels, including the aorta or the pulmonary arteries.
Surgery may be necessary. Hypertension, or high blood pressure, may eventually become a problem.
The patient will require regular monitoring. Hypercalcemia, or high blood calcium levels can lead to colic-like symptoms and irritability in infants.
Signs and symptoms normally ease as the child gets older, but there may be lifelong problems with calcium levels and vitamin D metabolism, and medications or a special diet may be necessary.
Day-night sleeping patterns may take longer to acquire.
Connective tissue. abnormalities increase the risk of a hernia, and joint problems, a soft, lax skin, and a hoarse voice.
Musculoskeletal problems may affect the bones and muscles. Joints may be lax, and there may be low muscle tone early in life.
Contractures, or joint stiffness, may develop. Physical therapy can help to improve muscle tone, joint range of motion, and strength.
Feeding problems may include a severe gag reflex, poor muscle tone, difficulty with sucking and swallowing, and tactile defensiveness. These problems tend to lessen with time.
Low birth weight may lead to a diagnosis of “failure to thrive.” A physician may be concerned that the infant does not gain weight fast enough.
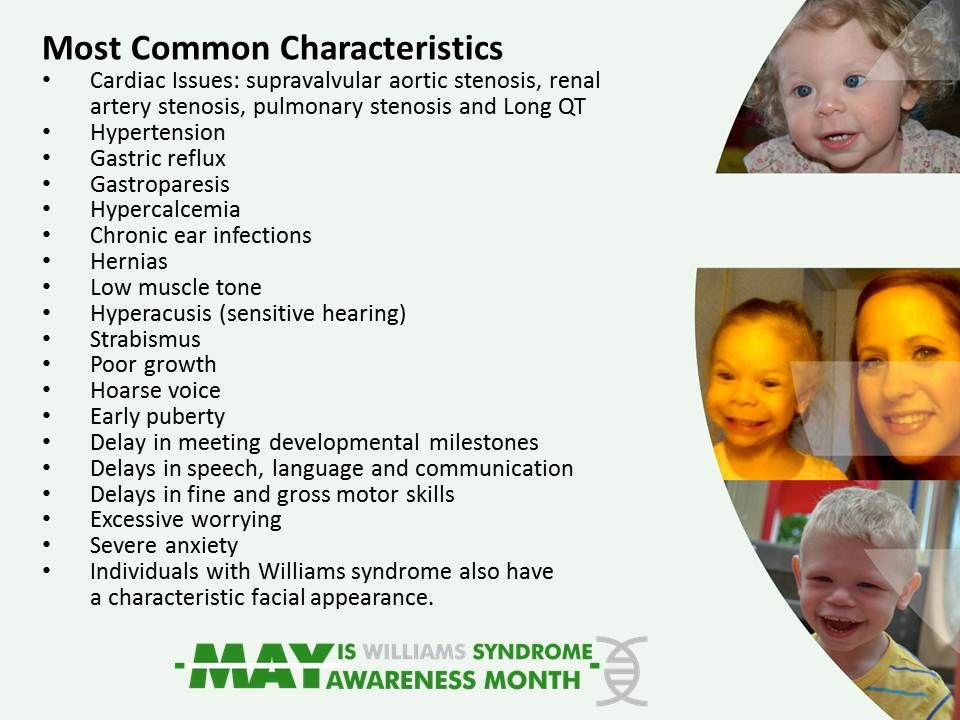
most adults with WS, stature is smaller than average. Cognitive and developmental features may involve mild to severe learning disabilities and cognitive challenges.
There may be difficulties with spatial relations and fine motor skills. Developmental delays are common, and it often takes longer than normal to learn to walk upright, talk, or become toilet trained. Kidney problems are slightly more common in people with WS.
Teeth may have an unusual appearance, being wide, slightly small, wand ith wider spacing than normal.
There may be abnormalities of occlusion, or the aligning tof he upper and lower teeth, for example, when chewing or biting.
Other Possible Symptoms
Curved spine, called scoliosis Farsightedness Hernia ; High levels of calcium in the blood ; Hoarse voice
pain in Joint and bone,
Kidney problems
Urinary tract infections,
Characteristics commonly seen during Infancy Often born post-term Small for the family background
Feeding difficulties – Gastro-esophageal (G-E) reflux, disordered suck and swallow, textural aversion, vomiting Failure to thrive Prolonged colic (>4 months) Chronic constipation
- Idiopathic hypercalcemia
- Strabismus Chronic otitis media
- Rectal prolapse
- Inguinal hernia
- Hypotonicity
- Hyperextensible joints
Systemic Involvement Cardiovascular pathologies
• Supravalvular aortic stenosis
• Hypertension
• Ventricular septal defect
• Patent ductus arteriosus
• Stenosis of outlying arteries (renal, cerebral, carotid, coronary,) brachiocephalic, subclavian, mesenteric, lung)
• Stenosis of the abdominal aorta
• Arteriovenous shunt
• Interruption of the aortic arch
• Vein aplasia
• Aortic aneurysm
• Pulmonary arterial stenosis
• Left and right ventricular hypertrophy
• Aortic coarctation
• Mitral valve prolapse
• Aortic valvular insufficiency Endocrine abnormalities
• Hypercalcemia
•Abnormalglucosemetabolis
• Thyroid hypoplasia
• Hypothyroidism Dental anomalies
• Small, abnormally shaped teeth
• Absent teeth
•MalocclusionGastrointestinal problems
• Dysmotility
• Reflux
• Constipation
•DiverticulardiseaseMusculoskeletal anomalies
• Joint laxity
• Joint stiffness as patient ages
• Tight heel cords
• Scoliosis
• Cervical kyphosis
• Exaggerated lumbar lordosis
• Radioulnar synestosis
• Gait – wide BOS, toe-walk forward posture Senses
• Sensorineural hearing loss
• Farsightedness
• Hyperopia
• Strabismus
• Otitis media Genitourinay anomalies
• Urinary frequency
• Bladder diverticuli Neurological problems
• Abnormal tone
• Hyperreflexia
• Cerebellar dysfunction
• Developmental delays
• Learning disabilities
DIAGNOSIS :
Diagnosis of the syndrome can be made at birth based on physical characteristics, but a true medical diagnosis is confirmed following a diagnostic test called fluorescence in situ hybridization (FISH).
The test reveals a recurring micro-deletion, with a size of 1,551,83 Mb, on chromosome band 7q11.23, which contains 24-28 gene
The deleted part of the chromosome band includes the elastin gene, which leads to serious cardiovascular complications
Elastin is a protein responsible for tissue elasticity. According to the Williams Syndrome Association, diagnosis of Williams syndrome begins with the recognition of physical symptoms and markers, which is followed by a confirmatory genetic test.
The physical signs that often indicate a suspected case of Williams syndrome include puffiness around the eyes, a long philtrum, and a stellate pattern in the iris.
Physiological symptoms that often contribute to aWilliams syndrome diagnosis are cardiovascular problems, particularly aortic or pulmonary stenosis, as well as feeding disturbance in infants.
Developmental delays are often taken as an initial sign of the syndrome, as well.
If a physician suspects a case of Williams syndrome, the diagnosis is confirmed using one of two possible genetic tests: micro-array analysis or the fluorescent in situ hybridization (FISH) test.
The FISH test examines chromosome #7 and probes for the existence of two copies of the elastin gene. Since 98-99% of individuals with Williams syndrome lack half of the 7q11.23 region of chromosome #7, where the elastin gene is located, the presence of only one copy of the gene is a strong sign of the syndrome
This confirmatory genetic test has been validated in epidemiological studies of the syndrome and has been demonstrated to be a more effective method of identifying Williams syndrome than previous methods, which often relied on the presence of cardiovascular problems and facial features (which, while common, are not always present
Some diagnostic studies suggest that reliance on facial features to identify Williams syndrome may cause a misdiagnosis of the condition.
Among the more reliable features suggestive of Williams are congenital heart disease, periorbital fullness (“puffy” eyes), and the presence of a long smooth philtrum.
Less reliable signs of the syndrome include anteverted nostrils, a wide mouth, and an elongated
Researchers indicate that even with significant clinical experience, it is difficult to reliably identify Williams syndrome based on facial features along:
TYPICAL AREAS WEAKNESS FOUD
- Trunk/core
- Shoulder, Hand
- Hip
- Foot and ankle.
Therapeutic Exercises used to treat the above weaknesses include:
Strengthening
stretching ex
Neuromuscular Re education
Neuromuscular Stabilitization ,
Functional Training (self-care and home management)
Functional Training in job/school/pl
The following muscles or muscle groups were targeted during strengthening treatment sessions:


1 -Abdominal exercise
Transverse Abdominus –Obliques –Lower Abdominals .
2 – Back
– back Extensors
3 -Shoulder girdle and attachments
- –Middle Trapezius
- –Lower Trapezius
- –Rhomboids
Muscles of or influencing the elbow, hand, hip, knee, ankle, and foot
Examples of methods for treating weaknesses include using the following:
For infants, toddlers, childreTREATPhysioball activities for trunk and core Increase resistance with t-band, weight, objects
For older children, adolescents, young adults–Physioball
–Resistance bands
–Free weights
–Machines
PHYSIOTHERAPY TREATMENT
Physical Therapy (PT); can be used to support the students with Williams Syndrome (WS) as they begin to participate in play-ground and gym activities.

Therapists need to work collaboratively with a student’s teacher, parents, and the school-based team to provide appropriate support for the the child to access the school environments (ex. classrooms, hallways, school bus, bathrooms, gym, playground, and school trip destinations) as well as assist balanced muscle tone and endurance.

Children with WS have low muscle tone, weak muscles, and difficulty with balance. With targeted interventions and individualized goals for these children, physical therapy can provide benefit in the following areas:
Gross and fine motor skilS
Enhance Strengthening of muscle and coordination of body movements
Increase classroom/school independence (ex. dressing, able to carry items while walking to cafeteria and playground)
Improve physical well being, balance, and self-confidence Enhance strengthening of body movement skills through activities that incorporate music
Children with WS generally have an affinity for music. Recognizing their strengths and interests in music, activities that teach different body movements through songs and video clips can lead to positive and enjoyable learning experiences for these children in a classroom setting.

examples of activities that can be initiated in a classroom are:
Teaching simple dance movements that consist of hopping, walking, jumping, and marching. (Other movements can be added to the list to gradually increase the level of difficulties).
Children with WS can select their favourite song as they are practicing these dance movements.
Engage in a class rhythm bands. This can be done using either real instruments (ex. drums or recorder) or by making musical instruments out of recyclable materials, such as using pans with spoons to make drums, empty plastic bottles with rice or beads inside to make shakers or cut-out tissue boxes with strings to make guitars

Encourage children with WS to imitate your action or act and move like various animals (ex. slither like a snake, waddle like a duck, hop like a rabbit, crab-walk) while changing the pace and speed of the song.