Facet Joint Syndrome: Cause, Symptoms, Treatment, Exercise
Table of Contents
What is a Facet Joint Syndrome?
Facet joint syndrome is a common cause of back and neck pain. It is caused by wear and tear on a joint or joints between your vertebrae (small bones that make up your spine).
Facet joints link the vertebrae (small backbones) together in your spine. These joints stabilize the spine and allow you to bend and twist.
Like any joints in your body, facet joints can start to weaken, causing pain. This can be caused by an injury or by everyday wear and tear. When the facet joints weaken, the condition is known as facet joint syndrome. Another term for facet joint syndrome is osteoarthritis. Facet joint syndrome can cause pain and even disability for some people.
Excessive rotation, extension, or flexion of the spine (repeated overuse) can result in degenerative changes to the cartilage of the joint and may involve degenerative changes to other structures including the intervertebral disc.
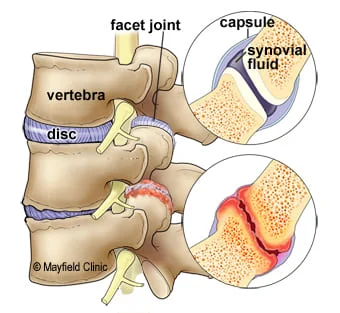
ANATOMY:
The spine is made of a column of moveable bones called vertebrae that connect to one another. Each vertebra functions as a three-joint complex with a large disc in the front and two facet joints in the back. This tripod design is strong — keeping the bones linked together while allowing our spine to bend and twist. Facets are synovial joints that are lined with cartilage, lubricated in synovial fluid, and covered by a joint capsule. Healthy facet joints glide and slide as the back moves, but prevent over-twisting.
Causes of Facet Joint Syndrome
Facet syndrome can be caused by trauma, such as a whiplash injury of the neck. Abnormal postures can overload spinal tissues, including the facet joints, and cause inflammation and pain in these joints. More commonly, degenerative changes in the cervical, thoracic, and lumbar spine can lead to abnormal stress and strain. This results in increased loads on the facet joints.
While primarily caused by natural wear and tear and degeneration, facet syndrome can also occur as a result of injury to the spine, or lifestyle choices.
These causes can include:
- Osteoarthritis
- Spondylolisthesis
- Obesity
- Smoking
- Malnutrition
- Trauma such as a car accident, fall, or sports injury.
Symptoms of Facet Joint Syndrome
Facet joint pain is felt locally as a unilateral back pain, which when severe can spread down the entire limb.
The joint capsule is more likely to generate pain than the articular cartilage or the synovium. All of the lumbar facet joints are capable of producing pain that can refer to the groin (this is more common with lower facet joint pathology).
Cervical facet syndrome includes the following symptoms:
-Axial neck pain (rarely radiating past the shoulders), most common unilaterally
-Pain with and/or limitation of extension and rotation
-Tenderness upon palpation
-radiating pain locally or into the shoulders or upper back, and rarely radiating in the front or down an arm or into the fingers as a herniated disc might.
Lumbar facet syndrome can be characterized by the following symptoms:
-Pain or tenderness in lower back (Low Back pain).
-Local tenderness/stiffness alongside the spine in the lower back.
-Pain, stiffness, or difficulty with certain movements (such as standing up straight or getting up from a chair.
-Pain upon hyperextension
-Referred pain from upper lumbar facet joints can extend into the hip and upper lateral thigh
-Referred pain from lower lumbar facet joints can penetrate deep into the thigh, laterally and/or posteriorly
-L4-L5 and L5-S1 facet joints can refer to pain extending into the distal lateral leg, and in rare instances to the foot.
Additionally, facet joint syndrome is more common in the elderly since changes at the joints develop with aging.
Acute episodes of lumbar and cervical facet joint pain are typically intermittent, generally unpredictable, and occur a few times per month or per year.
Typically, there will be greater aggravation of symptoms with lumbar extension than lumbar flexion. In lumbar cases, the standing may be somewhat limited but sitting and riding in a car are most provocative.
DIAGNOSIS:
The diagnosis of facet joint syndrome usually begins with a complete history and physical exam.Your doctor may order other diagnostic tests as well.
X-RAY
X-rays may be recommended to determine whether there are abnormalities in your spine.
CT-SCAN
A CT scan can sometimes show more detail about your facet joint surfaces. If the X-rays suggest something may be affecting your facet joints, your doctor may recommend a CT scan to get a better look.
BONE SCAN
A bone scan can be useful in determining whether your facet joints are inflamed. An inflamed facet joint usually shows up as a hot spot on a bone scan.
EXAMINATION:
Inspection:
Inspection should include an evaluation of paraspinal muscle fullness or asymmetry, increase or decrease in lumbar lordosis, muscle atrophy, or posture asymmetry.
Patients with chronic facet syndrome may have flattening of the lumbar lordotic curves and rotation or lateral bending at the sacroiliac joint or thoracolumbar area.
Palpation:
The examiner should palpate along the paravertebral regions and directly over the transverse processes because the facet joints are not truly palpable. This is performed in an attempt to localize and reproduce any point tenderness, which is usually present with facet joint–mediated pain.
In some cases, facet joint–mediated pain may radiate to the gluteal or posterior thigh regions.
Range of motion:
Range of motion should be assessed through flexion, extension, lateral bending, and rotation With facet joint–mediated LBP, pain is often increased with hyperextension or rotation of the lumbar spine, and it might be either focal or radiating.
Flexibility:
Inflexibility of the pelvic musculature can directly impact the mechanics of the lumbosacral spine.
With facet joint pathology, the clinician may find an abnormal pelvic tilt and rotation of the hip secondary to tight hamstrings, hip rotators, and the quadratus, but these findings are nonspecific and can be found in patients with other causes of LBP.
Sensory examination:
Sensory examination (ie, light touch and pinprick in a dermatomal distribution) findings are usually normal in persons with facet joint pathology.
Muscle stretch reflexes:
Patients with facet joint–mediated LBP usually have normal muscle stretch reflexes. Radicular findings are usually absent unless the patient has nerve root impingement from bony overgrowth or a synovial cyst.
Side-to-side asymmetry should lead one to consider possible nerve root impingement.
Muscle strength:
Manual muscle testing is important to determine whether the weakness is present and whether the distribution of weakness corresponds to a single root, multiple roots, or a peripheral nerve or plexus.
Typically, manual muscle testing results are normal in persons with facet joint pathology; however, subtle weakness of the muscles of the pelvic girdle may contribute to pelvic tilt abnormalities. This subtle weakness may be appreciated with trunk, pelvic, and lower-extremity extension asymmetry.
Treatment of Facet Joint Syndrome
MEDICAL:
Pharmacological therapy commonly consists of the prescription of muscle relaxants prescribed by a physician to treat acute back pains secondary to facet joint syndrome.
Pain-relieving medicine includes nonsteroidal anti-inflammatory drugs(NSAIDS) and acetaminophen as a first-line intervention to help decrease LBP. Little evidence supports one particular drug over another.
treatment for facet joint syndrome pain includes intra-articular steroid injections and radiofrequency ablation of the medial branches innervating the joints. Yet there is much controversy in scientific articles related to this standard treatment.
SURGICAL:
FACET JOINT INJECTIONS:
Injections to the facet joint can be used to either diagnose or treat facet joint pain. The therapeutic injection is given to the medial branch of the facet nerve of the affected joint. It is the branch of the facet nerve that controls the innervation to the joint itself. Numbing this branch can alleviate the pain of all the downstream branches of the facet nerve significantly. The relief from facet joint injections is temporary, and there are limits on how frequently they can be administered.
NERVE ABLATION:
The goal of this procedure is to block the pain signals by destroying (ablation) the nerve endings surrounding the damaged facet joint (4). The nerve ablation can be done using several techniques including radiofrequency, thermocoagulation, and neurolysis. However, the nerve can grow back in time, and hence the procedure provides only a temporary solution.
FACET FUSION:
A facet fusion procedure is the most reliable form of treatment for facet pain. The procedure is performed to permanently cure facet-mediated pain. A spacer is placed into the facet joint to stabilize it and stop the joint from rubbing on the nerve, thus stopping the pain. This is a simple outpatient procedure with quick recovery; most patients are back to work within a week.
Physiotherapy of Facet Joint Syndrome
PREVENTION:
Poor posture plays a major role in the development of Facet Syndrome. Prolonged sitting and bending postures, where the lumbar spine is ‘flexed’ should be avoided as they increase the pressure on the discs.
Positions of side bending can also put excess pressure on the Facet joints and cause excess load and injury. This can lead to disc degeneration and a loss of disc height. As the discs shrink the Facet joints come into contact with each other and start to bear weight.
The curves increase the load-carrying capability of the spine compared to if the spine was just straight. The lumbar part of the spine consists of a forward curve and as long as this is maintained, posture will be reasonably good, reducing the strain on individual joints and discs.
It is important that this improved posture is maintained during all activities, particularly when sitting for long periods – slumping should be avoided.
Sitting with cross legs or looking to the side should be avoided as they place asymmetrical stress on the spine. A computer, TV, or laptop should be positioned straight in front of the body so you don’t have to sit at an angle.
A Lumbar Roll placed at the bottom of the back or a Seating Support can be effective when sitting to maintain the natural curve of the lumbar spine.
Driving for long periods should be avoided if possible and where it is unavoidable regular breaks with stabilizing exercises and stretches, particularly in a backward (extension) motion to counteract the forward position of sitting, can be a good idea.
MASSAGE:
it will improve blood circulation in that area and remove waste products from the blood and reduce pain. also, it brings good nutrients to that particular area and helps in reducing pain.
ULTRASOUND:
Focused ultrasound is an early-stage, noninvasive, therapeutic technology with the potential to improve the quality of life and decrease the cost of care for patients with back pain, as a common cause is arthritis of the facet joints. This novel technology focuses beams of ultrasound energy precisely and accurately on targets deep in the body with minimal damage to surrounding normal tissue. Where the beams converge, the ultrasound produces precise destruction of tissue. With regard to the treatment of back pain, the sensory nerves that transmit pain signals are targeted which in turn diminishes the sensation of back pain in the treated patient.
TENS (Transcutaneous Electrical Nervous stimulation)
With TENS a small electrical current is used to help reduce muscle spasms and theoretically help to block some of the painful messages sent to the brain by peripheral nerves.
HOT AND COLD THERAPY:
Applying heat to the lower back improves circulation, which reduces muscle spasms and tension and improves mobility.
Ice packs can reduce inflammation and numb mild pain.
It can be helpful to apply heat before physical activities to relax the muscles and to apply ice after activity to minimize inflammation.
EXERCISES:
- STRETCHING:
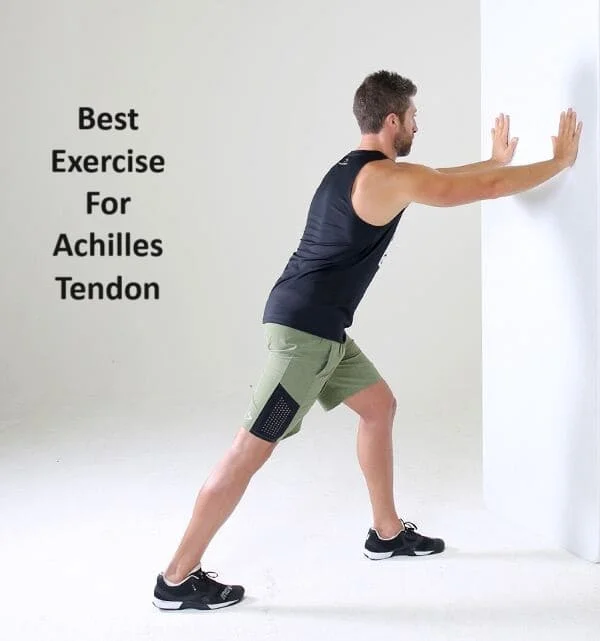
CALF STRETCH:

- Stand near a wall with one foot in front of the other, front knee slightly bent.
- Keep your back knee straight, your heel on the ground, and lean toward the wall.
- Feel the stretch all along the calf of your back leg.
- Hold this stretch for 20-30 seconds.
- Switch legs, then alternate for a total of 3 repetitions.
HAMSTRING STRETCH:
- lying flat on your back with both legs flat on the floor.
- Next, bring your right knee towards your body and support your right thigh with your hands—or wrap a towel around your thigh and firmly hold each end of the towel.
- Raise your right foot towards the ceiling with the goal of placing your right leg in a perpendicular position. You can gently pull on the towel to bring your leg closer to your body.
- Hold this position for 30 seconds, and then repeat on your opposite leg.
PIRIFORMIS STRETCH:

- lying on your back on the floor.
- Cross the right leg over the left, with the right ankle resting on the left knee.
- Slowly lift the left foot off the floor and toward you while you apply gentle pressure to the inside of the right knee.
- Hold 20 to 30 seconds, and repeat on the other side.
KNEE TO CHEST:

- Lie on your back with your feet flat on the floor.
- Bring your right knee toward your chest, using your hands to hold your leg in the stretched position. Hold for 10 seconds.
- Lower your right leg and repeat the exercise with the left knee. Hold for 10 seconds.
- Repeat with each leg 3 to 5 times.
- After stretching each leg individually, perform the exercise by holding both knees in the stretched position. Hold for 10 seconds and repeat 3 to 5 times.
2. STRENGTHENING EXERCISE:
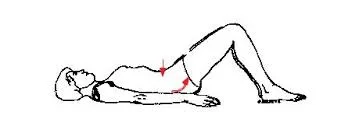
BRIDGING:-
- Lie on your back with bent knees hip distance apart and feet flat on the mat stacked under the knees.
- Engage the core and squeeze your glutes as you lift your hips to a bridge. Hold, squeezing tight, and return to the mat with control.
- Perform 8-12 Repetitions. Rest for 1 Minute.
STATIC ABDOMINAL:
- Lie on your back with your feet flat on the floor.
- As you exhale, squeeze your abdominal muscles, push your belly button toward the floor, and flatten your lower back.
- Hold for 5 seconds. Relax.
Repeat 10 times, holding for 5 seconds each time.
PRONE SLR:
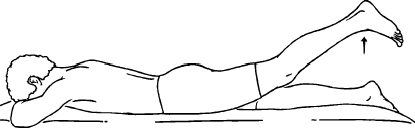
- Lie face down (prone) on the floor.
- Gently tighten your core muscles by keeping your abdominal muscles engaged. You should still be able to breathe while doing this.
- Keeping your abs engaged and your knees straight, slowly lift one leg up backward. You should keep your knee straight as your thigh lifts from the floor.
- Hold your straight leg up in the air for two seconds, and then slowly lower your leg back to the floor. Be sure you do not rotate your back or your pelvis while lifting your leg.
- Perform the exercise slowly for 10 to 15 repetitions, and then repeat the exercise for the opposite leg.
FOREARM SUPPORT:

- Lie in a prone position(face down)
- Put your forearm at 90 degrees with your arm and stretch your body up without lifting your elbow from the floor.
- Hold this position for 10-15 sec and then relax.
Repeat this for 10 times.
CAT AND CAMEL:
- Get onto your hands and knees, with your knees spaced hip-width apart and your hands directly beneath your shoulders.
- Tighten your abdominal muscles and arch your spine upward toward the ceiling.
- Hold the position for at least 10 seconds, then slowly relax your back.
- Allow your stomach to fall toward the floor, bring your shoulders together and stretch your back downwards into a swayback position.
- Hold for 10 seconds, then return to the starting position.
Repeat the entire sequence at least three more times.