Diabetic Macular Edema
Table of Contents
What is a Diabetic Macular Edema?
Diabetic macular edema (DME) is a diabetes complication. People combined with type 1 or type 2 diabetes might get DME.
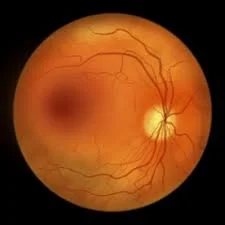
DME occurs when excess fluid accumulates in the eye’s macula. The macula helps us focus and see fine details. It is located in the centre of the retina, the blood vessel-rich lining at the back of the eyeball.
When excess fluid accumulates in the macula, it causes vision problems.
DME typically develops over time. High blood glucose levels can harm the blood vessels in the retina. Damaged blood vessels can leak fluid, resulting in swelling and other complications. This damage is known as retinopathy.
There are many treatment options for DME. It is simple to correct if diagnosed early and examined regularly by an eye doctor.
Causes of Diabetic Macular Edema
High blood sugar levels weaken the blood vessels in the eyes. This can cause them to leak or grow out of control in your retina, the light-sensitive area at the back of the eye. This is known as diabetic retinopathy.
When fluid enters your retina, it can cause diabetic macular edoema. The leaking causes swelling in your retina, which impairs the function of your macula, the special, sensitive part that provides you with sharp vision.
The medical term “edema” refers to swelling caused by excess fluid. So DME is a fluid buildup that causes your macula to swell due to diabetes.
Diabetes is the leading cause of macular edoema. However, it can also occur due to cataract surgery or other eye procedures, macular degeneration, uveal swelling (the middle part of your eye), blocked veins in your retina, or radiation damage.
Certain medications for diabetes, cancer, and multiple sclerosis can cause macular edoema.
Types of diabetic macular edema
There are two major ones.
Focal DME refers to small areas of fluid leakage.
Diffuse DME causes leaks and swelling throughout the macula.
With diffuse DME, your vision may worsen.
Pathophysiology
Normal retinal circulation is distinct in that retinal capillaries are not fenestrated, and capillary endothelial cells have tight junctions; normal capillaries do not leak fluid or blood. The retina lacks a lymphatic system, so leaking fluid can accumulate and cause edoema or swelling in the presence of retinal pathology. The retina responds to ischemia by stimulating growth factors to form new vessels (known as neovascularization).
DME is the result of microvascular changes in diabetes, which cause vessel incompetence and edoema. The hypoxic state stimulates VEGF, which causes more edoema.
Thus, two significant changes take place:
- Vessel permeability
Damaged endothelial walls become more porous.
Vessels leak fluid, lipids, and erythrocytes.
Fluid accumulation causes edoema (macular edoema if it occurs in the retina’s central region).
- Vessel closure.
The supply of oxygen and nutrients has decreased. The new brittle development occurs (due to ischemia).
Symptoms of diabetic macular edema
In the initial phases, there could be no signs. If you have diabetes, you should see an eye doctor at least once a year to have your eyes examined for changes. If there is any evidence of retinopathy or DME, prompt treatment can prevent or restore vision.
Tell your eye doctor if you have any of the following symptoms:
- blurred vision
- Seeing colours that appear washed out
- see more floaters in your vision.
- Double vision.
- Scotomas, or dark spots.
- Straight lines that appear to be bent or curved.
- Difficulty seeing in glare or bright light.
- When you look at an object with one eye and then the other, it appears to be of a different size.
Risk factors
Increased risk of DME is linked to:
- Poor glucose control over an extended period
- Increased time with diabetes- People with diabetes have a 10% chance of developing DME over their lifetime.
- Type of diabetes: After 20 years of diabetes, almost all type 1 diabetics and 60% of type 2 diabetics will suffer from diabetic retinopathy. Initially, it usually does not affect vision.
- Very high blood pressure.
- Fluid retention
- Kidney disease.
- High levels of fat in the blood (hyperlipidemia).
- Pregnancy – Women who develop diabetes while pregnant are at risk for diabetic retinopathy and DME.
Diagnosis
You cannot see swelling in your retina, but your eye care specialist can when they perform a thorough examination. This is one reason why you should have regular eye exams. Maintaining a regular eye exam schedule is especially important if you have diabetes.
In addition to the eye exam, which includes a slit lamp exam, your provider may perform the following tests to diagnose and monitor DME:
- Optical coherence tomography: This imaging test determines the thickness of your retina and optic nerve.
- Fluorescein angiography: This imaging test visualises the blood vessels in your retina.
- In a visual field test, the Amsler grid is used. This grid includes vertical and horizontal lines.
Treatment of diabetic macular edema
There are effective treatments for DME. Annual eye exams can detect changes at an early stage. If you have DME, treatments can help you keep your vision and even reverse vision loss.
The doctor treating your eyes may suggest several treatments.
Laser therapy
This therapy option is typically available in a clinical setting, such as your eye doctor’s office.
Laser therapy targets damaged areas of the retina with tiny lasers. This procedure seals leaking blood vessels and inhibits abnormal blood vessel growth.
Laser therapy can help you keep your current vision and prevent further loss of vision.
To repair eye damage, you will most likely need multiple laser treatments over time. If you sustain further eye damage, you may require additional treatments.
Drugs for diabetes-related macular edoema
One way that providers treat DME is to administer a series of intravitreal injections of medications. These medications include:
Aflibercept (Eylea®).
Avastin® (bevacizumab).
Faracimab-svoa (VABYSMO®).
Ranibizumab (Lucentis®).
Dexamethasone (ozurdex®).
Fluocinolone Acetonide (Iluvien®).
Ozurdex and Iluvien are steroid implants that your doctor will inject into your eye.
Protecting Your Eyes
Diabetes is a lifelong condition, so maintaining a healthy lifestyle and monitoring your blood sugar, blood pressure, and cholesterol levels are critical to preventing eye damage.
The following can help to preserve your vision.
- Monitor your blood sugar levels regularly, aiming to stay within the range recommended by your doctor or nurse.
- Maintain an appropriate weight and blood pressure.
- Consume plenty of fruits and green vegetables.
- Drink only a small amount of alcohol.
- Take regular exercise.
- Don’t smoke.
You must attend your diabetes clinic appointments. Your diabetes care team will oversee and manage your diabetes treatment plan. Make sure to get your eyes checked at least once a year to catch any problems early.
If you wear glasses or contact lenses, continue to see your optician regularly and inform them that you have diabetes.
Summary
Diabetic macular edema (DME) is a complication of diabetes, resulting from excess fluid accumulation in the eye’s macula. This condition can occur in people with type 1 or type 2 diabetes and can be caused by high blood glucose levels, cataract surgery, macular degeneration, uveal swelling, blocked veins, or radiation damage.
DME can be caused by microvascular changes in diabetes, leading to vessel incompetence and edoema. Symptoms include blurred vision, double vision, scotomas, bent lines, and difficulty seeing in glare or bright light. Risk factors include poor glucose control, prolonged diabetes, type of diabetes, high blood pressure, fluid retention, kidney disease, high-fat levels, and pregnancy.
Treatment options for DME include laser therapy, which targets damaged retina areas with tiny lasers, and medications like Aflibercept, Avastin, Faracimab-svoa, Venibizumab, Dexamethasone, and Fluocinolone Acetonide.
Maintaining a healthy lifestyle and monitoring blood sugar, blood pressure, and cholesterol levels are crucial to preventing eye damage. Regular eye exams and regular eye care are essential for early detection and treatment.
FAQs
DME begins when your blood sugar is not under control. Consistently high blood sugar damages blood vessels throughout your body, including those in your heart, as well as the small blood vessels in your retina – the back of the eye.
Laser therapy (photocoagulation) may be used by providers to seal the blood vessels in your eyes, preventing leakage. Your doctor may also recommend a vitrectomy. This procedure can remove scar tissue and cloudy vitreous fluid from your eye.
optical coherence tomography (OCT).
This test allows the doctor to see the back of your eye by taking pictures of the retina and other parts of the eye using a special machine. This can help your doctor determine how much swelling there is.
The primary pathophysiologic process is the breakdown of the blood-retinal barrier, which normally prevents water movement in the retina and allows fluid to accumulate in the retinal tissue via special water fluxes. Inflammatory processes and increased vascular permeability play a key role.
References
- Professional, C. C. M. (n.d.). Diabetes-Related Macular Edema. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/24733-diabetes-related-macular-edema
- Rd, C. W. (2020, October 12). Diabetic Macular Edema: What You Need to Know. Healthline. https://www.healthline.com/health/eye-health/diabetic-macular-edema-symptoms-treatment
- Stuart, A. (2014, September 11). Diabetic Macular Edema. WebMD. https://www.webmd.com/diabetes/diabetic-macular-edema
- Diabetic Macular Edema (DME) – Prevent Blindness. (2023, October 24). Prevent Blindness. https://preventblindness.org/diabetic-macular-edema-dme/
- Diabetic Macular Edema Causes and Symptoms. (n.d.). WebMD. https://www.webmd.com/diabetes/diabetic-macular-edema-causes-symptoms
- Diabetic macular oedema (DMO). (n.d.). https://www.macularsociety.org/macular-disease/macular-conditions/diabetic-macular-oedema/