Diabetic Neuropathy
Table of Contents
What Is Diabetic Neuropathy?
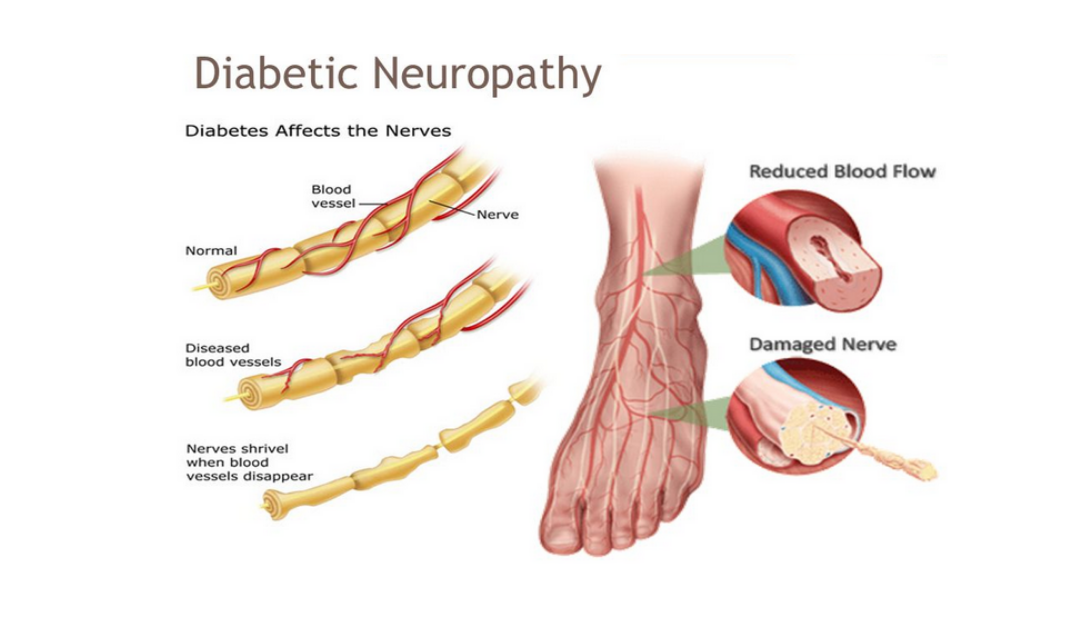
Diabetes can damage the nerves of the body, this damage is known as neuropathy which may be painful. Diabetic neuropathy is a type of nerve injury or damage that is caused by diabetes. Over time, high levels of fats, such as triglycerides in the blood from diabetes and long-term high blood glucose levels, also called blood sugar can damage a person’s nerves throughout the body.
Symptoms of this condition depend on which type of diabetic neuropathy patients have. Diabetes can affect nerves that control sensation, movement, and other functions. This most often damages nerves in the feet and legs. Diabetic neuropathy is a common and serious complication of type 1 and types 2 diabetes. The condition generally develops gradually, sometimes over the course of a few decades.
Various types of nerve damage cause various symptoms. Depending on the affected nerves, diabetic neuropathy symptoms include numbness and pain in the hands, legs, and feet. It can also cause problems with the functions of internal organs including various systems such as the digestive system, urinary tract, heart, and blood vessels. Few patients have mild symptoms. But for some patients, diabetic neuropathy can be disabling and quite painful. In cases of prolonged or severe diabetic neuropathy, patients may be vulnerable to infections or injuries. In serious cases, infection or poor wound healing can lead to amputation.
Diabetic neuropathy is a serious and harmful diabetes complication that may affect as half as 50% of patients with diabetes but patients can frequently slow its progress or prevent diabetic neuropathy with consistent blood sugar management and a healthy lifestyle. If someone has diabetes, they can develop nerve problems at any time. Sometimes, the first sign of diabetes can be neuropathy. Significant nerve problems such as clinical neuropathy can develop within the first 10 years after a diagnosis of diabetes. The risk of developing diabetic neuropathy increases the longer patients have diabetes.
What are the symptoms of diabetic neuropathy?
It is common for symptoms of diabetic neuropathy to be seen slowly. In a large number of cases, the nerves of the feet are involved to occur the first type of nerve damage, which can lead to the symptom of sometimes painful “pins and needles” in the patient’s feet.
Symptoms vary, which depends on the areas affected. General symptoms and signs of the different types of diabetic neuropathy include:
- Loss of sensation of light touch
- High sensitivity to touch
- Problems with coordination while walking
- Pain or numbness in a patient’s feet or hands
- Burning sensation in feet, mostly during nighttime
- Increased heart rate
- Muscle wasting or weakness
- Bloating or fullness
- Nausea, vomiting, or indigestion
- Diarrhea or constipation
- Dizziness when a patient stands up
- Decreased or excessive sweating
- Erectile dysfunction
- Bladder problems, such as incomplete bladder emptying
- Vaginal dryness
- Vision problems, such as double vision
- Inability to sense low blood glucose
What are the different types of diabetic neuropathy?
Diabetic neuropathy can be differentiated into various types. This is because we have various kinds of nerves in our bodies that serve their own various functions. Patients’ symptoms and treatments depend on which type of diabetic neuropathy they have. A patient may have symptoms of several types or just one type. Most types of diabetic neuropathy develop slowly or gradually, and patients may not notice problems until a major issue or damage has occurred. Consult with a doctor if patients have any of the following symptoms. The earlier they can be diagnosed and treated, the better the chance of preventing or reducing more complications.
There are mainly four types of diabetic neuropathy:
- Peripheral neuropathy
- Autonomic neuropathy
- Proximal neuropathy
- Focal neuropathy
Peripheral Neuropathy
Peripheral diabetic neuropathy has various other names including, peripheral diabetic nerve pain and distal polyneuropathy. This is the most general form of neuropathy caused by diabetes. It affects nerves leading to patients’ extremities—to their feet, legs, arms, and hands. A patient’s legs and feet are frequently affected first, followed by their hands and arms. The nerves, which are going to the person’s feet are the longest in the body, after they branch off the spinal cord in the lumbar region or low back, they go all the way down the person’s legs and into the feet, quite a distance.
Symptoms can be varied and seen as mild to severe. Possible symptoms and signs of peripheral neuropathy include:
- Numbness or reduced ability to feel pain
- Insensitivity to cold and hot temperatures, mostly in patient’s toes and feet
- A burning or tingling sensation
- Sharp, jabbing pain or cramping that may be worse at night
- Extreme sensitivity to the lightest touch, which includes for some patients even the weight of a sheet can be agonizing
- Muscle weakness
- Loss of reflex response
- loss of coordination or balance
- Serious foot problems, such as infections, ulcers, foot deformities, amputations, and bone, and joint pain
- If someone has peripheral neuropathy, they may not feel a sore or an injury on their foot. A patient with diabetes generally has poor circulation, which makes it more complicated for wounds to heal. This combination raises the risk of infection. In extreme or severe cases, an infection can lead to amputation.
Autonomic Neuropathy
The second most common type of neuropathy in patients with diabetes is autonomic neuropathy.
Autonomic nerves are useful to keep a person’s body running as it should. The autonomic nervous system runs other systems in the body over which a person has no conscious control. Many muscles and organs are controlled by these nerves, including:
- sweat glands
- digestive system
- cardiovascular system
- sex organs and bladder
- oculomotor system
The autonomic nervous system controls the stomach, intestines, heart, lungs, bladder, sex organs, and eyes. There are many functions that happen in the body without individual thinking about them, such as a person’s heart pumps, can breathe, and the stomach digesting food. These all actions are controlled by the autonomic nervous system, which is also sometimes called the automatic nervous system.
The autonomic nervous system should maintain the human body’s homeostasis, which is its balanced, normal state. If the autonomic nerves are damaged by the effects of diabetes means by autonomic diabetic neuropathy, then the body may have difficulty maintaining homeostasis.
However, the patient’s symptoms depend on what specific nerves in the autonomic nervous system are affected. The symptoms of this condition include:
- Decreased or increased sweating
- Problems regulating patient’s body temperature
- Changes in the way patient’s eyes adjust from light to dark
Nerve issues to the digestive system may cause:
- Uncontrolled diarrhea, constipation, or a combination of the two problems
- swallowing difficulty
- Gastroparesis, causes the stomach to empty too slowly into the small intestines, which causes a delay in digestion and can worsen over time, leading to frequent vomiting and nausea. A patient will typically feel full too fast and be unable to complete a meal.
- Delayed digestion frequently makes it harder to control blood glucose levels frequently alternating low and high readings.
- Symptoms of hypoglycemia, such as heart palpitations and sweating, can go undetected inpatient with autonomic neuropathy. This means not noticing when a person has low blood sugar, known as hypoglycemia unawareness, which increases the risk for a hypoglycemic emergency.
Sexual and bladder problems
- Autonomic neuropathy may cause sexual problems, such as erectile dysfunction in men, Vaginal dryness and other sexual difficulties in women, or difficulty achieving orgasm. Neuropathy in the bladder can cause urinary incontinence or make it difficult to fully empty the bladder, along with that problems including frequent urinary tract infections, or urinary retention
Cardiovascular problems
- Damage to the nerves that control blood pressure and heart rate can make patients respond more slowly. A patient may experience a drop in blood pressure and feel dizzy or lightheaded when they stand up after lying down or sitting known as orthostatic hypotension, or when the patient exerts themself. Autonomic neuropathy can also cause an abnormally increased heart rate even when a patient is at rest
Autonomic neuropathy can make it harder to identify a few of the symptoms of a heart attack. A patient may not feel any chest pain when his heart is not getting enough oxygen. If patients have autonomic neuropathy, they should know the other warning signs of heart attack, including:
- profuse sweating
- pain in the arm, neck, back, jaw, or stomach
- shortness of breath
- lightheadedness
- nausea
Proximal neuropathy
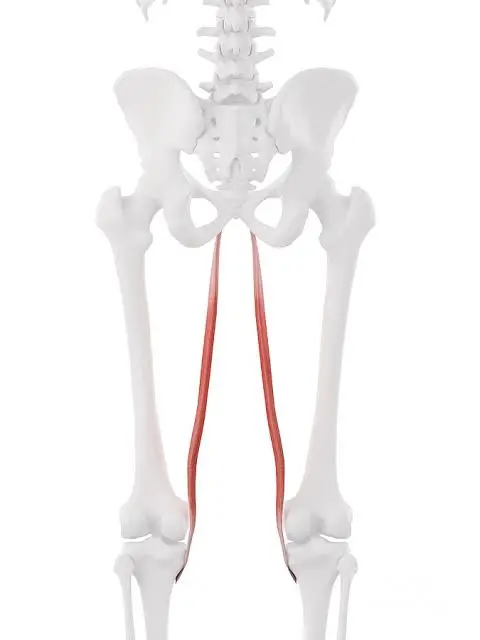
A rare form of neuropathy is proximal neuropathy, also known as diabetic polyradiculopathy and diabetic amyotrophy. This “myo” in the word means muscle, which can cause muscle weakness, so this is a form of neuropathy. It generally affects the muscles in the upper part of the patient’s leg, hips, and buttocks.
Sometimes, proximal neuropathy patients have nerve pain, especially pain that shoots and arises from the lower back and down the leg. The medical term for this pain is a radiculopathy, although most patients refers to it as sciatica. If there is also shooting nerve pain involved, this form of neuropathy can be known as polyradiculopathy-diabetic amyotrophy.
This type of diabetic neuropathy is more generally seen in adults over 50 years old with fairly well-controlled diabetes type 2 and is more frequent in men. It generally affects elderly patients with diabetes; in opposite to peripheral neuropathy, it usually resolves with treatment or time.
Symptoms are generally on one side of the body, however, in some cases, symptoms may spread to the other side, also. Most patients improve at least partially around six to 12 months.
This condition is often marked by symptoms and signs including:
- Sudden, severe pain in the patient’s hip and buttock or thigh
- Shrinking and weakness of the thigh muscles
- Difficulty in standing from a sitting position without assistance
Focal Neuropathy (Mononeuropathy)
All the types of diabetic neuropathy including peripheral, proximal, and, autonomic, are examples of polyneuropathy. The meaning of “Poly” is that they affect numerous nerves. Focal neuropathy involves damage to a specific nerve so that it is focused neuropathy, which is also known as mononeuropathy. It is most commonly seen in older adults.
Focal neuropathy, which comes on suddenly, most frequently affects nerves in the head or face particularly ones that go to the eyes. It can also affect the legs and torso.
Although mononeuropathy can cause severe and sudden pain, it generally can not cause any long-term issues. Symptoms generally lessen and disappear on their own over a few months or weeks. Symptoms and signs depend on which nerve is involved, and it may include:
- Difficulty in focusing eyes, aching behind one eye, and double vision
- Paralysis on one side of the patient’s face, known as Bell’s palsy
- Pain in patient’s foot or shin
- Pain in the front of the patient’s thigh
- chest or stomach pain
- pain in isolated areas, such as the lower back, front of the thigh, pelvic region, stomach, chest, inside the foot, outside the lower leg, or weakness in the big toe
Sometimes mononeuropathy or focal neuropathy occurs when a nerve is compressed. Carpal tunnel syndrome is a mostly seen type of compression neuropathy in patients with diabetes. Although the most patient doesn’t feel the symptoms of carpal tunnel syndrome, approximately 25 percent of patients with diabetes have few degrees of nerve compression at the wrist. The sooner treatment starts, the better the chance of reduction of complications.
Symptoms and signs of carpal tunnel syndrome include:
- Numbness or tingling in patient’s hands or fingers, particularly in patient’s index finger, middle finger, ring finger, and thumb.
- Loss or reduction of strength with a sense of weakness in the patient’s hand and a tendency to drop things
What causes diabetic neuropathy?
The exact cause of every type of neuropathy is unknown. Any person who has diabetes can develop diabetic neuropathy. But below given risk factors make nerve damage more easily:
Poor blood sugar control
Uncontrolled blood sugar raises the chances of risks of each diabetes complication, including nerve damage and interferes with their ability to send signals, which leads to diabetic neuropathy. High blood sugar also weakens the walls of the small blood vessels means capillaries that supply the nerves with nutrients and oxygen.
Diabetes history
The risk of diabetic neuropathy increases the longer a patient has diabetes, particularly if blood sugar is not well controlled.
Metabolic factors
In addition to glucose levels, high cholesterol and triglyceride levels are also associated with a higher risk of neuropathy.
Kidney disease
Diabetes can injure the kidneys. Kidney damage sends toxins or infiltrated materials into the blood, which can lead to nerve damage.
Mechanical injury
It includes injuries caused by carpal tunnel syndrome
Being overweight
If a person has a body mass index (BMI) of 25 or higher may increase the risk of diabetic neuropathy. Patients who are obese or overweight are also at increased risk of having neuropathy.
Smoking
Smoking hardens and narrows the arteries, reducing blood flow to the feet and legs. This damages the peripheral nerves and makes it harder for wounds to heal. lifestyle factors, such as alcohol use or smoking
Low levels of vitamin B-12
This can also lead to neuropathy. Metformin, a common medicine used to treat diabetes, can decline levels of vitamin B-12.
What are the Stages of the severity of diabetic neuropathy?
A common staging scale of diabetic polyneuropathy is as follows:
Stage 0: No signs and symptoms
Stage 1: Signs but no symptoms of neuropathy
Asymptomatic neuropathy
1a: No signs and symptoms but nerve conduction velocity abnormalities or autonomic test abnormalities
1b: N1a criteria+ neurological examination abnormality. Vibration detection threshold abnormality
Stage 2: Symptomatic neuropathy
2a: Symptoms, signs, and tests abnormality*
2b: N2a criteria+ significant weakness of ankle dorsiflexion
Stage 3: Disabling polyneuropathy
*Tests include nerve conduction, quantitative sensory testing, and quantitative autonomic testing
What are the possible complications of diabetic neuropathy?
Diabetic neuropathy can cause a number of dangerous complications, including:
Hypoglycemia unawareness
Blood sugar levels below 70 milligrams per deciliter (mg/dL) mean 3.9 millimoles per liter (mmol/L) is generally cause sweating, shakiness, and a fast heartbeat. however, patients who have autonomic neuropathy may not feel these warning signs.
Loss of a leg, foot, or toe sensations
Nerve damage can cause a loss of feeling in the leg and feet, so even minor cuts can turn into ulcers or sores without being seen. In severe cases, an infection can lead to tissue death or spread to the bony part. Removal means amputation of a foot, toe, or even part of the leg may be required. Smoking leads to the risk of foot problems in patients with a few types of diabetic neuropathy. A doctor can give advice on quitting smoking and a podiatrist can help with foot care.
Urinary tract infections and urinary incontinence
If the nerves that control the bladder are injured or damaged, they no longer respond normally as the bladder fills with urine, as a result, the bladder may not empty completely while urination. Urine remains in the bladder or is released without warning signs. Bacteria can build up in the kidneys and bladder, which causes urinary tract infections. Nerve damage can also affect to control of the muscles that release urine or the ability to feel the need to urinate, leading to leakage or incontinence.
A sharp decrease in blood pressure
Damage to the nerves that stimulate blood flow can impact the body’s ability to adjust blood pressure. This can cause a sharp drop in blood pressure while standing after lying down or sitting, which may lead to fainting and lightheadedness, and dizziness when standing. In a few cases, the nerves in the heart are also affected. They may not work properly to help the patient’s heart keep normal blood pressure when patients stand up.
Digestive problems
If nerve damage occurs in the digestive tract, diarrhea or constipation, or both can possibly occur. Diabetes-related nerve problems can lead to gastroparesis, which is a condition in which the stomach empties too slowly or not at all. It may lose the ability to move food down easily into the small intestine. This can cause bloating, vomiting, and indigestion. It changes how quickly the body absorbs food. It can make it harder to compensate insulin dose to food portions. A patient may have diarrhea if the nerves that control their small intestine are damaged. Diarrhea mostly occurs at night. A patient may also have constipation because of damage to nerves in the intestines.
Sexual dysfunction
Autonomic neuropathy frequently damages the nerves that affect the sex organs. Females may have difficulty with arousal and lubrication. Male may feel erectile dysfunction. Neuropathy may cause erectile dysfunction if it affects the nerves which control erections. This means patients may have trouble keeping or having an erection. This problem does not generally affect the desire for sex.
Increased or decreased sweating
Nerve damage can damage the work of the sweat glands and make it harder for the body to control its temperature properly.
Changes in vision
Vision can be affected. Patients may develop retinopathy. This initiates with changes in blood vessels of the retina. The retina is at the back of the eye, the light-sensitive tissue. In a few cases, the blood vessels can leak or swell fluid. In other cases, new blood vessels may develop on the surface of the retina. Over time, this can lead to total vision loss. The patient’s eye care provider may treat retinopathy to make tiny burns by using a laser. These burns seal the blood vessels of the eyes. This stops them from leaking and growing. Other times, one or more of the nerves that move the patient’s eyes in a coordinated way may have a loss of blood supply, like during a stroke, which can cause double vision. Also, injury to the nerves that control the diameter of the patient’s pupils can lead to difficulty seeing in low light.
How is diabetic neuropathy diagnosed?
A doctor or health care provider can generally diagnose diabetic neuropathy by performing a physical exam and carefully reviewing the patient’s symptoms and medical history. Early diagnosis of diabetic neuropathy gives patients the best chance of proper and effective treatment. But not all limb or foot pain means diabetic neuropathy, accurate and proper diagnosis is essential to ensure appropriate treatment.
Health care provider or doctor typically checks patient:
- Overall muscle tone and strength
- Tendon reflexes
- Sensitivity to pain, light touch, temperature, position, and vibration
Besides the physical exam, a doctor may advise or perform specific tests to help diagnose diabetic neuropathy, such as:
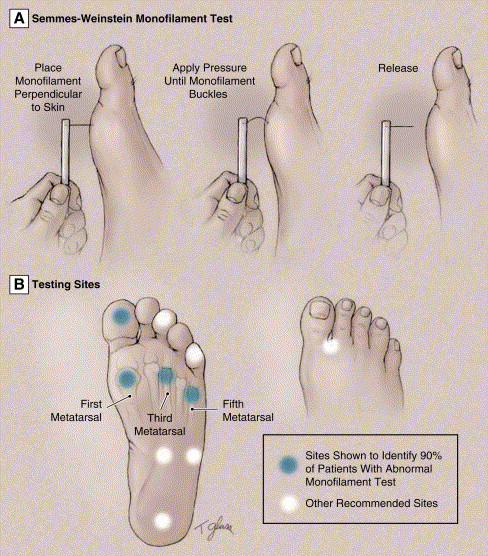
Filament testing
A soft nylon fiber known as monofilament is brushed over areas of patients’ skin to test their sensitivity to light touch.
Sensory testing
This non-invasive test is used to tell how a patient’s nerves respond to changes in temperature and vibration.
Nerve conduction testing
This test measures how quickly the nerves in the patient’s legs and arms conduct electrical signals. It is useful to check the flow of electrical current by a nerve.
Electromyography
It is also called needle testing, this test is usually done along with nerve conduction studies. It measures electrical discharges produced in a patient’s muscles and determines how muscles respond to electrical impulses.
Autonomic testing
Special tests may be done to determine how patients’ blood pressure changes while they are in various positions, and whether their sweating is within the standard range.
A comprehensive evaluation
It includes a review of blood pressure, blood glucose, and cholesterol screenings, which combined with more advanced screening, helps the doctor rule out other causes and identify the main problem.
Ultrasound
It is used to determine how parts of the urinary tract are functioning for the evaluation of the kidney.
Skin biopsies
It is useful to evaluate cutaneous nerve innervation of the body.
Nerve and muscle biopsies
They are for histopathological evaluation of the body.
How to treat diabetic neuropathy?
Diabetic neuropathy has no known cure and particular treatment plan. The goals of treatment for this condition include:
- Slow progression
- Relieve pain
- Manage complications and restore function
Slowing progression of the disease
Consistently keeping patients’ blood sugar within their target range is the key to delaying or preventing nerve damage. Fine blood sugar treatment may even improve some of the patient’s current symptoms. A doctor will figure out the best target range for patients based on factors including patients’ age, how long they have had diabetes, and their overall health. Blood sugar levels need to be personalized. But, in common, the American Diabetes Association (ADA) recommends the following target blood sugar levels for most patients with diabetes:
- Before meals, between 80 and 130 mg/dL (4.4 and 7.2 mmol/L)
- Two hours after meals, less than 180 mg/dL (10.0 mmol/L)
- The American Diabetes Association (ADA) generally recommends an A1C of 7.0% or lower for most patients with diabetes.
Other important ways to help prevent or slow neuropathy from getting worse include keeping the patient’s blood pressure under control, getting regular physical activity, and maintaining a healthy weight.
Pain relief treatment
Pain-relieving prescription treatments may include:
Anti-seizure drugs
Some medicines used to treat seizure disorders meaning epilepsy are also used to ease nerve pain. The ADA recommends initiate with pregabalin (Lyrica). Gabapentin (Neurontin, Gralise) also is used.
Side effects may include dizziness, drowsiness, and swelling in the feet and hands.
Antidepressants
Some antidepressants ease nerve pain, even if a patient is not depressed. Tricyclic antidepressants may be useful for mild to moderate nerve pain. Drugs in this, include nortriptyline (Pamelor), amitriptyline, and desipramine (Norpramin).
Side effects can be problematic and include constipation, dry mouth, drowsiness, and difficulty in concentration. It may also cause dizziness while changing position, such as from lying down to standing, known as orthostatic hypotension.
Serotonin and norepinephrine reuptake inhibitors (SNRIs) are other types of antidepressants that can help with nerve pain. The ADA recommends duloxetine (Drizalma Sprinkle, Cymbalta) as an initial treatment. Possible side effects include sleepiness, nausea, dizziness, constipation, and decreased appetite.
Sometimes, an antidepressant drug may be combined with an anti-seizure drug. For example, the Patient may find relief from ibuprofen (Advil, Motrin IB, others) or acetaminophen (Tylenol, others), or a skin patch with lidocaine (a numbing substance).
Alternative therapies
There are some alternative therapies that may help with pain relief in combination with medications or on their own. But check with a doctor before using any dietary supplement or alternative therapy to make sure that the patient does not have any potential interactions.
For diabetic neuropathy, a patient may want to try:
Capsaicin
Capsaicin cream, applied to the skin, can reduce pain sensations in some patients. Side effects may include skin irritation and a burning feeling.
Alpha-lipoic acid
This powerful antioxidant is seen in some foods and may help relieve nerve pain symptoms in a few patients.
Acetyl-L-carnitine
This nutrient is available as a supplement and is naturally made in the body. It may relieve nerve pain in some patients.
Transcutaneous electrical nerve stimulation (TENS)
This prescription therapy may help avoid pain signals from reaching the brain. TENS send tiny electrical impulses to particular nerve pathways through small electrodes placed on the skin.
Acupuncture
Acupuncture may help relieve the pain of neuropathy and mainly does not have any side effects. A patient may not get immediate relief with acupuncture and might require more than 1 session.
Manage complications and restore function
To manage complications, patients may require care from various specialists. These may include a heart specialist (cardiologist) and a specialist who treats urinary tract problems (urologist) who can help treat or prevent complications.
The treatment patients will need depends on the neuropathy-related complications they have:
Urinary tract problems
Some drugs affect bladder function, so a doctor may recommend changing or stopping medications. A strict urination schedule or urinating every few hours means timed urination while applying gentle pressure to the bladder area, below the patient’s belly button can help some bladder problems. Other management, including self-catheterization, may be required to remove urine from a nerve-damaged bladder.
Digestive problems
To relieve mild symptoms and signs of gastroparesis that are belching, indigestion, nausea, or vomiting, eating smaller, more often meals may help. Diet changes and medications may help relieve diarrhea, gastroparesis, constipation, and nausea.
Low blood pressure on standing means orthostatic hypotension
The treatment initiates with simple lifestyle changes, such as drinking plenty of water, not using alcohol, and changing positions such as from sitting to standing slowly. Sleeping with the head of the bed up 4 to 6 inches helps avoid high blood pressure overnight. A doctor may recommend compression support for the patient’s abdomen and thighs (abdominal binder and compression stockings or shorts). Some medicines, together or alone, may be used to treat orthostatic hypotension.
Sexual dysfunction
Medicines taken by injection or mouth may improve sexual function in a few men, but they aren’t safe and effective for all. Mechanical vacuum devices may raise blood flow to the penis. Vaginal lubricants may benefit women.
Lifestyle modification and home remedies
These below-given measures can help patients feel better in general and reduce their risk of diabetic neuropathy:
Keep patient’s blood pressure under control
If patients have high diabetes and blood pressure, they have an even greater risk of complications. Try to keep their blood pressure in the range their doctor recommends, and be sure to have checked it at every clinic visit.
Make healthy food choices and preferences
Eat a balanced diet that includes a variety of healthy foods specifically fruits, vegetables, and whole grains. Limit portion sizes to help maintain or achieve a healthy weight.
Be active every day
Exercise helps improves blood flow, lowers blood sugar, and keeps the patient’s heart-healthy. Make a goal for 75 minutes of vigorous aerobic activity or 150 minutes of moderate a week, or a combination of vigorous and moderate exercise. It is
also a good idea to get a few fast bursts of activity to take a break from sitting every 30 minutes. Talk with the patient’s doctor or physiotherapist before starting exercising. If a patient has decreased feeling in their legs, some types of exercise including walking may be safer than other types of exercises. If a patient has a foot sore or injury, stick with exercise that does not require putting weight on their injured foot.
Stop smoking
Using tobacco in any form makes patients more likely to produce poor circulation in their feet, which can cause problems with healing. If patients use tobacco, talk to their health care provider about finding ways to stop it.
Physiotherapy treatment for diabetic neuropathy
Regular exercise and physiotherapy treatment can help control blood sugar levels and help reduce neuropathic pain. Diabetic patients must tightly monitor their blood sugar levels during exercise time to prevent major fluctuations or changes. This may involve to given education on conditions to patients and monitoring blood sugars, ideally by a multi-disciplined approach in rehabilitation.
Physiotherapy treatment can reduce dependency on pain relief medicine therapies. Some physiotherapy techniques can help alleviate symptoms brought on by diabetic neuropathy such as deep pain in the legs and feet, burning or tingling sensation in limbs, muscle weakness, muscle cramps, sexual dysfunction, and diabetic foot. Exercise programs with manual therapy can help to prevent muscle spasms, contractures, and atrophy. A good physiotherapist will confirm that exercises for patients with diabetic neuropathy do not hurt the feet, which can be sensitive.
Specific exercise programs should include:
Flexibility training
It includes progressive stretching and self stretches. These programs may include general muscle stretching to maintain a patient’s range of motion and muscle length.
Strengthening exercises
General muscle strengthening exercises can help to maintain and improve muscle strength and reduce muscle wasting.
Muscle strengthening by using a variety of modes as appropriate such as isometric, graded weight progression with weight cuff, dumbbells or therabands, and close and open-chain strength training can moderately improve muscle function in patients with diabetic neuropathy.
Aerobic activity
Aerobic exercise for 30 minutes 4 times a week, such as using a stationary bicycle and swimming can help diabetic neuropathy, but activities that place excessive pressure on the feet such as walking for long distances, and running may be contraindicated.
Balance training
The major consequence of diabetic neuropathy is an increase in the risk of falls. This training program may help with fall prevention and stability.
For static balance training:
Tandem leg stance for first 2 weeks and then it was progressed to heel stance and single leg stance toe.
Marching
Balance board exercises
For dynamic balance training:
Sideways walk the backward walk and tandem walk.
Gait training
It can improve or re-learning walking or gait patterns in patients with diabetic neuropathy. Posture training, gait training, and teaching these patients the basic principles of off-loading can help stabilize and/or prevent foot complications such as foot ulcers and injuries. Off-loading techniques can include the use of foot splints or mobility aids such as crutches. Gait re-training can also be beneficial for patients who have lost limbs known as amputation, because of diabetic neuropathy, and then wear a prosthesis.
Pelvic floor muscle exercises
These exercises can improve sexual dysfunction caused by diabetic neuropathy.
Electrical nerve stimulation
An electrical modality, a type of physiotherapy might help to reduce feelings of stiffness and improve the healing of foot ulcers and injuries.
Splint
Physiotherapy may also involve splinting for muscle weakness such as Ankle foot orthoses or for mononeuropathies eg. carpal tunnel syndrome.
Tight glucose control
Treatment of early manifestation of sensorimotor polyneuropathy involves improving glycemic control of patients with diabetes. Tight control of blood glucose can reverse the changes of diabetic neuropathy, but only if diabetes and neuropathy are recent in onset. Conversely, painful symptoms of neuropathy in uncontrolled diabetics tend to subside as the numbness and disease progress.
Massage therapy
A massage therapist, or chiropractor, can carry out manual therapy or regular massages to stretch the muscles. Massage can inhibit muscle spasms, contractions, and atrophy due to poor blood supply.
Physiotherapeutic treatment of Pain in Diabetic Neuropathy
Interferential current therapy (IFT) and Transcutaneous electrical nerve stimulation (TENS)
They use a painless electric current and the physiological effects of low-frequency electrical stimulation to relieve stiffness, relieve neuropathic pain, improve mobility, reduce edema, and heal resistant foot ulcers or injuries.
Therapeutic ultrasound
It is another type of physiotherapy modality that uses very high-frequency sound waves to stimulate the tissue under the skin. This can help some patients to regain sensitivity in their feet.
Low-intensity laser therapy
Static magnetic field therapy
Monochromatic infrared light
It is a non-invasive painless modality that effectively treats diabetic neuropathy as well as other neuropathies. Infrared light therapy is effective in helping restore or produce a normal sensory threshold back to the feet of neuropathy patients within 30 days to 60 days, depending upon the severity.
Heat and hot wax are also useful for treating diabetic neuropathy.




3 Comments