Peripheral neuropathy
Table of Contents
What is Peripheral Neuropathy?
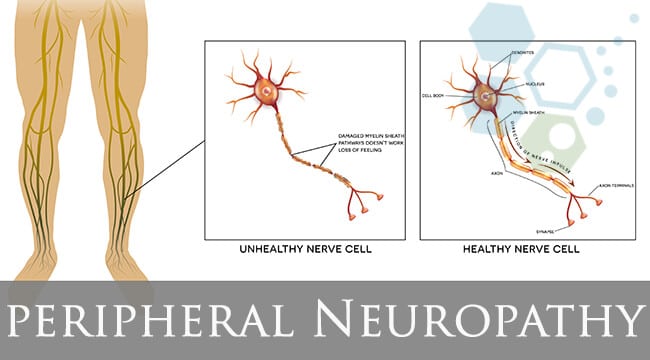
- Peripheral neuropathy, a result of damage or disease to the nerves located outside of the spinal cord and brain which is peripheral nerves, causes numbness, weakness, and pain, usually in the feet and hands. It can also affect other areas and body functions including circulation, digestion, and urination.
- The peripheral nervous system sends information from the central nervous system which includes the brain and spinal cord to the rest of the body. The peripheral nervous system sends sensory information to the central nervous system (CNS). The peripheral nerves make up an intricate network that connects the brain and spinal cord to the skin, muscles, and internal organs.
- Peripheral nerves come out of the spinal cord, which is arranged along lines in the body known as dermatomes. Generally, damage to a nerve will affect single or more dermatomes, which can identify specific areas of the body. Damage to peripheral nerves interrupts communication between the brain and other parts of the body and can prevent normal sensation in the arms and legs, impair muscle movement, and cause pain.
- Peripheral neuropathy can result from infections, traumatic injuries, metabolic problems, inherited causes, and exposure to toxins.
- The condition can affect a range of various nerves, so it can affect a variety of locations in various ways. It can affect several nerves or a single nerve at the same time.
- Peripheral neuropathy affects more than 20 million people in the United States (US). In general, the condition can cause inappropriate or distorted signals, or cause a loss of normal nerve signals.
What are the types of peripheral neuropathy?
There are higher than 100 types of peripheral neuropathy that stem from a variety of causes, each with its own set of prognosis and symptoms. They range from carpal tunnel syndrome, which is a traumatic injury common after chronic repetitive use of the wrists and hands, such as with computer use; to nerve damage linked to diabetes.
Motor neuropathy
This is damage to the nerves that control movement and muscles in the body, such as moving arms and hands or talking.
Sensory neuropathy
Sensory nerves control what feel, such as pain, temperature a light touch, these groups of nerves are affected by sensory neuropathy.
Autonomic nerve neuropathy
Autonomic nerves control unconscious functions, such as heartbeat and breathing. Damage to these groups of nerves can be dangerous.
Mononeuropathy
Damage or injury to a single peripheral nerve is known as mononeuropathy. Physical trauma or injury from an accident is the most common reason. Prolonged pressure on a nerve, because of long periods of being sedentary such as lying in bed or sitting in a wheelchair; or repetitive, continuous motions, can trigger a mononeuropathy
- The most common type of mononeuropathy is Carpal tunnel syndrome. It is known as an overuse strain injury, which occurs when the nerve that travels from the wrist is compressed. People whose work requires repeated motions with the wrist such as physical laborers, assembly-line workers, and those who use computer keyboards for prolonged periods are at greater risk.
- The damage to the nerve can result in tingling, numbness, unusual sensations, and pain in the first three fingers on the thumb side of the hand. The patient may wake up at night with numbness in their hand or discover that when they perform activities such as using a hairdryer, the numbness is more noticeable. In long term, carpal tunnel injuries can weaken the hand muscles. A patient may also feel pain, tingling, or burning in the shoulder and arm.
- Ulnar nerve palsy occurs when the nerve at the elbow that passes close to the surface of the skin is damaged. The numbness can be felt in the 4th and 5th digits of the hand.
- Radial nerve palsy can occur with fractures of the humerus bone in the upper part of the arm and also is caused by injury to the nerve that runs along the underside of the upper arm.
- Peroneal nerve palsy results when the nerve on the outside of the knee at the top of the calf is compressed. This leads to a condition known as “foot drop,” in which difficult to lift the foot.
Polyneuropathy
When multiple peripheral nerves throughout the body malfunction at the same time, It occurs. Polyneuropathy can have various types of causes, including exposure to certain toxins such as alcohol abuse, poor nutrition especially vitamin B deficiency, and complications from diseases such as kidney failure or cancer.
- Diabetic neuropathy is the most common form of chronic polyneuropathy, a condition that occurs in patients with diabetes. It is a more severe inpatient with poorly controlled blood sugar levels.
- Guillain-Barre syndrome is one of the most serious polyneuropathies, a rare disease that strikes suddenly when the body’s immune system attacks nerves in the body just as they leave the spinal cord. Symptoms usually appear quickly and worsen fast, sometimes leading to paralysis. Early symptoms include tingling and weakness that eventually may spread upward into the arms. Heart rhythm problems, blood pressure problems, and breathing difficulty may occur in the more severe cases. However, along with the severity of the disease, recovery rates are also good when patients receive treatment as soon as possible.
- Chronic inflammatory demyelinating polyneuropathy is a chronic form of Guillain-Barre in which the sign and symptoms happen for months and years. Early treatment and diagnosis are crucial for these patients, 30% of which risk eventually being confined to a wheelchair.
What are the symptoms of peripheral neuropathy?
Each nerve in the peripheral system has a particular function, so symptoms depend on the type of nerves affected. Symptoms of peripheral neuropathy vary depending on the location and type of the nerves involved. Symptoms can develop slowly over time, called chronic neuropathy, or appear quickly, which is called acute neuropathy. Nerves are classified into different categories, including:
Sensory neuropathy
This affects the sensory nerves, which impact the sensations of touch, pain, and temperature.
Symptoms:
- Decreased sensation of touch and vibration
- Pins and needle sensations, hypersensitivity
- Inability to feel pain or increased pain
- Loss of ability to detect changes in cold and heat
- Difficulty with balance and coordination
- Burning, stabbing, boring, lancing, or shooting pains, which may be worse at night
- Particularly in cases when the cause is diabetes, sensory neuropathy can also lead to leg and foot ulcers, infection, and gangrene.
Motor neuropathy
This affects the muscles of the body, which controls by the brain consciously..
Symptoms:
- Muscle weakness which leads to unsteadiness and difficulty performing small movements like buttoning a shirt
- Muscle shrinking
- Muscle wasting
- Muscle cramps and twitching
Autonomic neuropathy
This affects body processes which control by the brain involuntarily.
Symptoms:
- Problems with sweating such as excessive sweating or not being able to sweat
- Heat intolerance
- Problems with bladder include urination; bowels include constipation and diarrhea; and digestion includes bloating, nausea/vomiting
- Drops in blood pressure or abnormal heart rate, causing lightheadedness or dizziness when standing up, fainting
- Sexual function problems.
- Difficulty with swallowing
- Weight loss (unintentional).
General signs and symptoms of peripheral neuropathy might include:
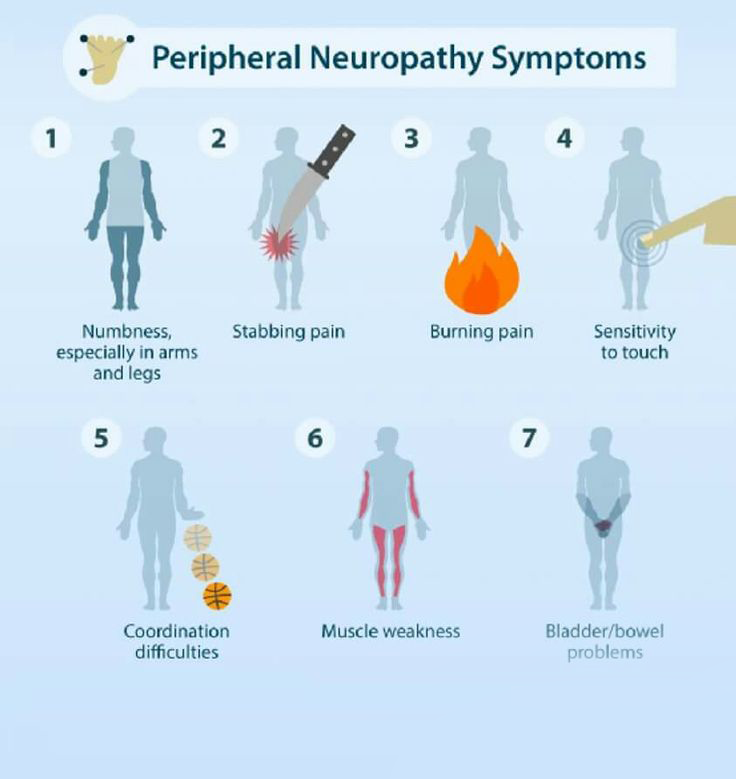
- Gradual onset of numbness, tingling, or prickling in hands or feet, which can spread upward into arms and legs
- Sharp, jabbing, throbbing or burning or electric-like pain
- Extreme sensitivity to touch or changes in sensation. Severe pain, especially during the night. Inability to feel pressure, pain, temperature, or touch.
- Pain during activities that can not cause pain, such as pain in your feet when they are under a blanket or when putting weight on them
- Lack of coordination and falling
- Muscle weakness, difficulty walking or moving legs or arms.
- Muscle twitching, spasms, and/or cramps.
- Not being able to feel things in your hands and feet – feeling like you are wearing gloves or socks when you’re not.
- Paralysis if motor nerves are affected along with loss of muscle tone, loss of muscle control, or dropping things out of hand.
What are the causes of peripheral neuropathy?
Peripheral neuropathy is nerve damage caused by a number of various conditions. Health issues that can cause peripheral neuropathy may include:
Autoimmune diseases
Sjogren’s syndrome, Rheumatoid arthritis, lupus, Guillain-Barre syndrome, chronic inflammatory demyelinating polyneuropathy, and vasculitis are autoimmune disorders that can cause neuropathy.
Diabetes
This is a leading cause of peripheral neuropathy in the United States. Among 60% to 70% of patients with diabetic peripheral neuropathy. Diabetes is the most common cause of small fiber type of neuropathy, which causes painful burning sensations in the feet and hands.
Infections
These include certain viral or bacterial infections, including Lyme disease, shingles, leprosy, Epstein-Barr virus, hepatitis B and C, diphtheria, chickenpox, and human immunodeficiency virus (HIV), herpes, syphilis, leprosy, West Nile virus can cause neuropathy.
Inherited disorders
Charcot-Marie-Tooth (CMT) disease is the most commonly seen hereditary type of neuropathy. This condition causes weakness in the lower leg and foot muscles and can also affect the muscles in the hands. Fabry disease Familial amyloidosis and metachromatic leukodystrophy are other examples of inherited disorders that can cause neuropathy.
Tumors
Growths, cancerous or malignant and noncancerous or benign, can press on nerves or develop on the nerves. Along with that, polyneuropathy can develop as a result of some cancers related to the body’s immune response.
Bone marrow disorders
These include an abnormal protein in the blood known as monoclonal gammopathies, a form of bone cancer that means myeloma, lymphoma, and the rare disease amyloidosis.
Other diseases
These include liver disease, kidney disease, connective tissue disorders, and an under-active thyroid means hypothyroidism.
Other causes of neuropathies include:
Alcoholism
Chronic alcoholism, which typically results in a lack of a well-rounded diet or Poor dietary choices, robs the body of thiamine and other important nutrients needed for nerve function. Along with that, it is directly toxic to peripheral nerves.
Exposure to poisons
Toxic substances including heavy metals such as lead and mercury and industrial chemicals, especially solvents can also affect nerve function. Exposure to toxic chemicals like glue, or insecticides, either through chemical abuse or in the workplace, can cause nerve damage.
Medications
- Some medications may cause nerve damage, which include:
- anticonvulsants, which patients take to treat seizures
- antibiotics, drugs to fight bacterial infections
- some blood pressure medicines
- medications used to treat cancer, such as chemotherapy and radiation
- HIV medications
- statins, a class of drugs used to prevent cardiovascular disease and lower cholesterol, cause neuropathy.
Injury or pressure on the nerve
Injuries, like motor vehicle accidents, fractures, falls or sports injuries can damage peripheral nerves. Nerve pressure can result from using crutches or having a cast or repeating a motion such as typing many times or narrowing the space through which nerves run, are other causes.
Vitamin deficiencies
B vitamins include B1, B6, and B12 — vitamin E and niacin are important to nerve function health.
Vascular disorders
Neuropathy can occur when blood flow to the legs and arms is slowed or decreased by inflammation, blood clots, or other blood vessel disorders. lower blood flow deprives the nerve cells of oxygen, causing nerve cell death or nerve damage. Vascular problems can be caused by smoking, vasculitis, and diabetes.
No known cause
Some cases of neuropathy have idiopathic or no known cause.
How the peripheral neuropathy is diagnosed?
Peripheral neuropathy has many feasible causes. Along with a physical exam, some tests include blood tests, diagnosis usually requires:
A complete medical history
The doctor will review a thorough medical history, including symptoms, current and past medications, lifestyle, exposure to toxic substances, diet and drinking habits, and a family history of the nervous system means neurological diseases, history of trauma, line of work, or social habits (looking for repetitive motions).
Neurological examination
The doctor might check tendon reflexes, muscle strength, tone, a person’s ability to feel certain sensations such as light touch or cold, patient’s posture, coordination, and balance.
Tests
The doctor may order tests, which include:
Blood tests
These tests can detect vitamin deficiencies and mineral imbalances, electrolyte imbalances, indicators of kidney problems, diabetes, other health issues; thyroid problems, toxic substances, antibodies to certain autoimmune diseases or viruses, and other possible conditions that may cause peripheral neuropathy.
Imaging tests
MRI or CT scans can look for tumors, herniated disks, pinched or compressed nerves, or other abnormalities affecting the bones and blood vessels.
Electrodiagnostic assessment (EDX): The doctor might send the patient to a nerve specialist for an EDX to find the degree and location of nerve damage. Electrodiagnostic assessment (EDX) includes two tests:
Electromyography (EMG)
An EMG can identify the health of a muscle, and determine if there is any disconnection between the muscle and nerve by measuring the electrical activity within the muscle while it is working. During electromyography (EMG), a very thin needle electrode is inserted through the skin into the muscle. After that, the muscle is used for a particular movement and the electrical activity of the muscle is recorded on a graph, which is known as an electromyogram.
Nerve conduction study (NCS)
In this, flat electrodes are placed on the skin over muscles and nerves on different parts of the patient’s body, usually, legs or arms and a low electric current stimulates the nerves. The test measures the size of the response and how quickly the nerve is carrying the electrical signal. Both sensory and motor nerves can be studied by this method.
Other nerve function tests
These might include a sweat test called a QSART test that measures your body’s ability to sweat, an autonomic reflex screen that records the work of autonomic nerve fibers, and sensory tests that record how you feel touch, pain, and vibration, cooling, and heat.
Nerve biopsy
This involves removing a small portion of a nerve, generally a sensory nerve, to find out for abnormalities in them.
Tissue biopsy
In some cases, a muscle, nerve, or skin biopsy is required to confirm the diagnosis. During a biopsy, a small sample of affected tissue is removed for examination for a reduction in nerve endings under a microscope.
Genetic testing
A genetic test may be required if the doctor suspects a genetic condition is causing the patient’s peripheral neuropathy.
What are the treatment options for peripheral neuropathy?
Treatment starts by identifying and treating any underlying medical issue, such as infections or diabetes. Few cases of peripheral neuropathy can be treated easily and sometimes cured. In this condition, treatment is aimed at relieving and controlling symptoms and preventing and managing further nerve damage. If the patient’s lab tests indicate no underlying condition, the doctor might advise watchful waiting to see if the patient’s peripheral neuropathy improves.
Medications
Along with medicines used to treat conditions related to peripheral neuropathy, medicines used to manage peripheral neuropathy symptoms and signs include:
Pain relievers
Over-the-counter pain medicines, such as non-steroidal anti-inflammatory drugs (NSAIDs), can relieve mild symptoms of pain. The doctor may prescribe painkillers, for more severe symptoms.
Medications containing opioids, such as oxycodone ( Roxicodone, Oxycontin, others), or Tramadol (Ultram, Conzip, others) can lead to addiction and dependence, so these drugs usually are not advised unless all other treatments fail.
Anti-seizure medications
Medications such as pregabalin (Lyrica) and gabapentin (Neurontin, Gralise, Horizant), may relieve nerve pain, which is mainly developed to treat epilepsy. Side effects of these medicines can include dizziness and drowsiness.
Topical treatments
Capsaicin cream, which contains a substance seen in hot peppers, can cause proper improvements in peripheral neuropathy symptoms. The patient might have irritation and skin burning where the cream is applied, but this generally decreases over the time period, however, some patients can not tolerate it.
Lidocaine patches
These are another treatment patient can apply to their skin that may offer pain relief. Side effects can include dizziness, drowsiness, and numbness at the site of the patch.
Antidepressants
Certain tricyclic antidepressants, such as doxepin (Silenor, Zonalon), amitriptyline, and nortriptyline (Pamelor), have been found to help relieve pain by interfering with chemical processes in a patient’s spinal cord and brain that cause the patient to feel pain.
The norepinephrine and serotonin reuptake inhibitor duloxetine (Drizalma Sprinkle, Cymbalta) and desvenlafaxine (Pristiq) and the extended-release antidepressants venlafaxine (Effexor XR) also might relieve the pain of peripheral neuropathy caused by diabetes.
Side effects of antidepressants may include nausea, drowsiness, dry mouth, dizziness, changes in appetite, constipation, and weight gain.
Therapies
Various procedures and therapies might help reduce the symptoms and signs of peripheral neuropathy.
Transcutaneous electrical nerve stimulation (TENS)
This treatment involves placing electrodes on the skin at or near the nerves which cause pain. A gentle, low-level electrical current at different frequencies is delivered through the electrodes to the skin. Treatment schedule includes, how often and how many minutes, is determined by a physiotherapist, which is usually applied for 30 minutes daily for about a month. The goal of TENS therapy is to discontinue the pain signals so they can’t reach the brain.
Immune suppressing or immune-modulating treatments
Various treatments are used for patients whose peripheral neuropathy is because of an autoimmune disease. These include IV infusion treatments, oral medications, or also procedures like plasmapheresis where antibodies and other immune system cells are removed from a patient’s blood and the blood is then returned to their body. The goal of these therapies is to discontinue the immune system from attacks on the nerves.
Plasma exchange and intravenous immune globulin
These treatments, which help suppress immune system activity, might benefit patients with certain inflammatory disorders. Plasma exchange involves removing of patient’s blood, after removing antibodies and other proteins from the blood and returning the blood to the body. In immune globulin therapy, patients get high levels of proteins that work as antibodies such as immunoglobulins.
Physical therapy
If the patient has muscle weakness, physiotherapy can help improve the movements. a physiotherapist can prescribe a walker or a wheelchair for mobility purposes. Mechanical aids, such as hand or foot braces and specially designed shoes, splints, and casts can help reduce pain by keeping the affected nerves in proper alignment or providing support.
Surgery
Surgery is advised for patients with compression-related neuropathy caused by pressure on nerves such things as a herniated disc in the neck or back, infections, tumors, or nerve entrapment disorders, such as carpal tunnel syndrome.
Occupational therapy
It can help patients cope with the loss of function and pain, and teach them skills to make up for this type of loss.
Proper nutrition
It involves eating a healthier diet and making sure to get the right balance of vitamins and other nutrients.
Adopting healthy living habits, including exercising quitting smoking, limiting alcohol intake, improving muscle strength, and maintaining a healthy weight.
Complementary treatments
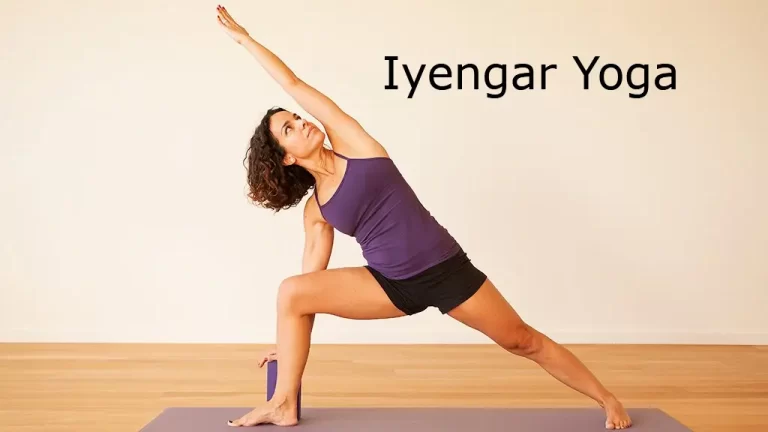
Acupuncture, massage, herbal products, alpha-lipoic acid, meditation or yoga, psychotherapy, and behavioral therapy are other methods that can be tried to help relieve neuropathic pain. Ask the doctor if any of these therapies may be helpful for treating the cause of the patient’s peripheral neuropathy.
Self-care
In addition to medicines for pain relief, many patients have seen relief for peripheral neuropathy through:
- Using an electric sock or heating pad
- Have a foot bath with nettle leaves or chamomile for at least 30 minutes
- Applying an ice pack to affected areas for 10 to 20 minutes twice daily in the evening and the morning
- Trying acupuncture
- Undergoing biofeedback
- Trying various types of holistic therapy such as tai chi, reflexology, or reiki
- Massaging affected areas to improve circulation
- Avoiding pressure on the affected area, like not leaning on elbows or crossing legs
- Seeking social activities and support from others
- Moderate, regular exercise can also help decrease discomfort.
- Avoiding caffeine and developing a regular bedtime routine to improve sleep habits
- If the patient drink alcohol or smoke, consider stopping or cutting back. Both tobacco and alcohol aggravate nerve pain and can cause nerve damage when in use for long periods.
Take precautions at home
If someone has peripheral neuropathy, they are potentially at higher risk for accidents in the home. someone can do the following to improve their safety:
- Use a stick or walker for stability purposes.
- Use safety guards and other things for sharp objects like knives and scissors.
- Use thermometers to measure the temperature of tap water or bath.
- Use gloves and potholders when handling hot things.
- Carefully wrap the patient’s feet and hands when it is cold outside.
- Install nightlights to avoid falling in the dark.
Physiotherapy treatment for peripheral neuropathy
Peripheral neuropathy is damage or disease affecting nerves, which may impair movement, sensation, organ or gland function, and affects other aspects of health, depending on the type of nerve affected. The treatment by a physiotherapist helps in the reduction of symptoms and improves the patient’s quality of life. As the type, cause, and symptoms of peripheral neuropathy can vary, the approach to managing the condition also varies.
Physiotherapy treatment will improve patients’ strength, mobility, function, and balance as well as their ability with daily tasks important to them.
The main role of Physiotherapy includes:
- To restore or maintain muscle strength, and prevent muscle deformity and shortening
- To improve coordination, balance, and functional training.
- To relieve pain e.g. provision of massage, TENS
- To prevent contractures and deformity, splints are needed
- To Educate, re-manage conditions, prevent damage, and give emotional support.
Treatment will depend on the individual symptoms of the patient, which may include:
Moderate intensity exercise
Physiotherapists may recommend moderate-intensity exercises to help improve the patient’s physical function and strength. A personal Individualized exercise program for every patient is required to strengthen muscles and improve fitness levels.
Strengthening exercises for peripheral neuropathy moderately increase muscle strength and power. When a patient can be done regularly, exercising can help. Exercises for strength training also reduce neuropathic pain and also help in controlling blood sugar levels. Strengthening muscles include exercising against increasing resistance, isometric exercise, and the use of weights.
Balance and coordination training
Balance exercises are an essential part of the recovery of peripheral neuropathy. A physiotherapist works on strategies to improve the patient’s coordination and balance, both of which may be altered by peripheral neuropathy. Improving coordination and balance helps to decrease patients’ risk of injuries and falls that happen due to this condition. Balance training helps in prevents falls and provides stability. Balance training is also vital in overcoming the feeling of unsteadiness and stiffness, especially among elderly patients.
Never gliding activities
To function correctly and well, nerves require 3 things: blood, movement, and space. Exercises that move and glide patients’ nerves are frequently effective at helping to manage symptoms of peripheral neuropathy, as well as promote nourishment and recovery of the nerve. Physiotherapists can show patients effective exercises that glide and move their nerves.
Education
The physiotherapist educates the patient on how to safely and carefully manage peripheral neuropathy. A patient’s education will vary based on their individual needs, and It mainly focuses on preventing further complications, improving their safety, and finding different ways to perform some tasks.
Kinetic therapy
It can not be started when progressive strength return can be seen until the late stage of nerve regeneration. After an injury or damage to the nerve, physiotherapeutic methods are used to avoid paresis and to restore the normal function of muscles along with improving the circulation of the body.
Electrostimulation
It plays a vital role in the treatment of different neuromuscular dysfunctions, which is given by the electrode placement on the affected area.
Magnetotherapy
It is used in this condition where a low-frequency pulsed magnetic field is applied. It has well-known effects on enhancing oxy-reductive processes, enzymatic activity, and proper blood circulation resulting in conduction characteristics and better oxidation of regenerating peripheral nerves. It improves the regeneration of nerve fibers.
Bio-laser stimulation
Low energy biostimulation lasers are used in palatial in a continuous proper manner. Laser radiation can also be used to again joining of the nerve stumps.
Bracing
The physiotherapist may prescribe bracing for peripheral neuropathy. Braces can be used to help you move safely or to protect injured nerves.
Maintain and improve functions via a range of motion or passive movement of joints and muscles through stretching.
Weight-bearing exercises through a joint.
Gait re-education to improve mobility and promote self-independence
Soft tissue massage
Task-specific activities using graded discrimination tasks, attentive exploration of objects without feedback, and vision.
Mirror imaging for stimulation of nerve pathways
Pain management
Hydrotherapy treatment increases circulation and relaxes muscles. This hydrotherapy treatment can also reduce pain and will enable patients to maximize their mobility in the water. Transcutaneous electrical nerve stimulation (TENS) is useful in pain relief.
Support and advice about diet
Advice about orthotics, walking aids, calipers, wheelchairs, braces, or splints can be used to improve balance and posture. Splinting is useful in the management of compression mononeuropathies, including carpal tunnel syndrome.
Exercises for peripheral neuropathy
There are mainly three types of exercises ideal for patients with peripheral neuropathy, which include
- Aerobic exercises
- Balance training
- Stretching exercise
Before the patient starts exercises, warm up muscles with dynamic stretching like arm circles, and rotations. This helps in improving flexibility and increases blood flow. It will activate nerve signals and also boost energy.
Aerobic exercises
Aerobic exercises cause a person to breathe deeply and move large muscles. This releases endorphins that act as the body’s natural painkillers and increase blood flow.
Best practices for aerobic exercising include routine activity for approximately 30 minutes a day, at least three days a week. If someone is just starting out, try this for 10 minutes a day to start. A few examples of aerobic exercises are:
- swimming
- brisk walking
- bicycling
Balance training
Peripheral neuropathy can leave a patient’s joints and muscles feeling stiff and often weak. Balance training can improve a patient’s strength and reduce feelings of tightness or stiffness. Improved balance also prevents or reduces the chances of falls. Beginning balance training exercises include calf and leg raises.
Calf raise
Using a counter or chair, steady the patient’s balance.
Lift the heels of both feet off the ground so the person is standing on his toes.
Slowly lower themself down.
Repeat for 10–15 reps.
Side leg raise
Using a counter or chair, steady the patient’s balance with one hand.
Stand straight with feet slightly apart.
Slowly lift one leg to the side and hold for 5–10 seconds.
Lower the leg at the same pace.
Repeat with the opposite leg.
As the patient improves balance, try this exercise without holding onto the counter.
Stretching exercises
Stretching increases patients’ flexibility and warms up their bodies for other physical activity. Routine stretching can also reduce their risk of developing an injury while doing exercise. Common techniques are seated hamstring stretches and calf stretches.
Seated hamstring stretch
Sit on the edge of a chair
Extend one leg in front of them-self with their toe pointed upward.
Bend the opposite knee with their foot flat on the floor.
Position their chest over their straight leg, and straighten their back until they feel a muscle stretch.
Hold this position for 20 – 30 seconds.
Repeat three times per leg.
Calf stretch
Place one leg behind the patient with their toe pointing forward.
Take a step forward with the opposite foot and slightly bend the knee.
Lean forward with the front leg while keeping the heel on their back leg planted on the floor.
Hold this stretch for 20 – 30 seconds.
Repeat three times per leg.




5 Comments